Vulvectomy
Simple Vulvectomy
Vulvectomy of any sort is not a simple operation because it destroys an important part of a woman’s normal anatomy and psychologically is a significant blow to the individual’s self-esteem. The vulva is an integral element of feminine sexual anatomy and physiology, and its loss seriously compromises an important day-to-day function. This operation therefore should be performed as a last resort when wide excision, laser excision, or laser vaporization cannot be performed, or when the end result of these procedures would produce a similar outcome—vulvectomy. A modification to simple vulvectomy is “skinning vulvectomy,” which is a shallower excision. Logically, the need for very deep excision for intraepithelial disease is difficult to justify because the average thickness of involved mucosa (hair-bearing areas) ranges from 0.35 to 1.6 mm (mean thickness, 0.93 mm ± 0.37 mm). The depth of involved appendages ranges from 0.43 to 3.6 mm (mean depth, 1.53 mm ± 0.77 mm). Thus an excision of 2 to 3 mm will remove in excess of 95% of involved skin and appendages, predictably eradicating the disease. No justification is known for excising the vulva to a depth greater than 5 mm unless the operation is being performed for invasive carcinoma.
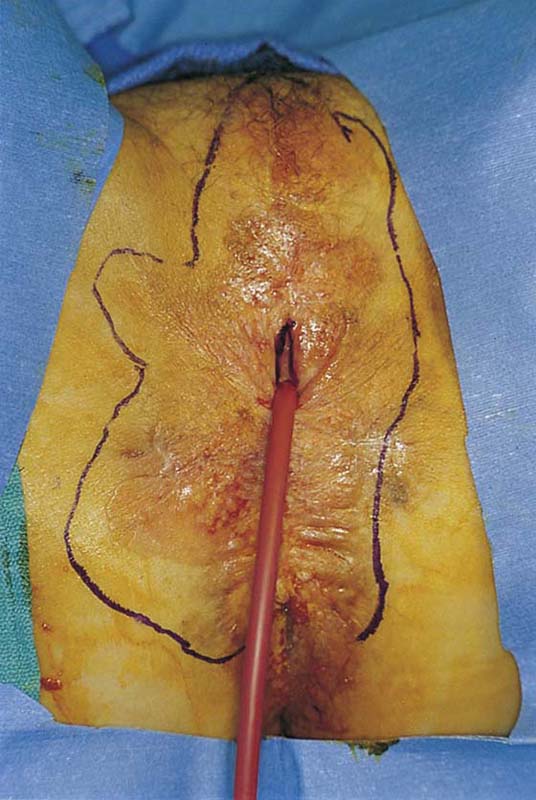
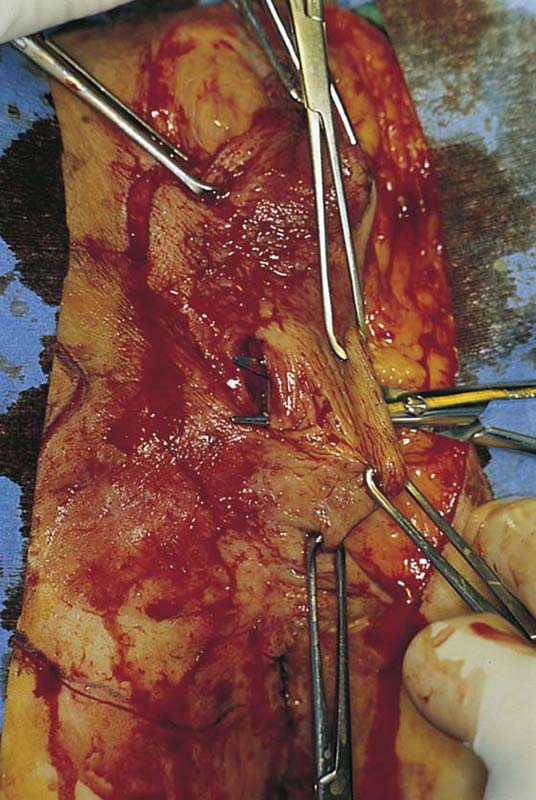
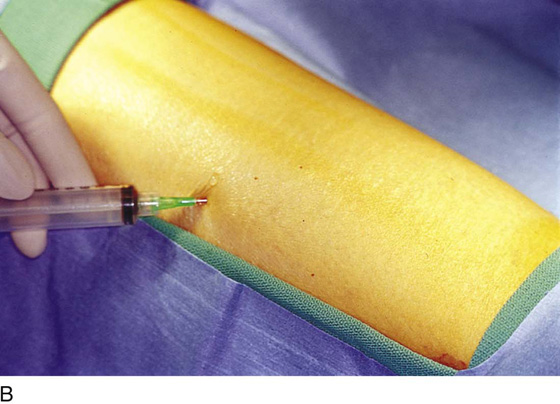
The patient is placed in the lithotomy position (not high lithotomy) (Fig. 71–1). After preparation, the extent of the incision should be sketched with a marking pen (Fig. 71–2). The incision is carried down from the lower mons to the lateral aspect of the labium majus with a 3-mm peripheral margin (from the lateral crease of the labium). This is continued to the lowest border of the labium majus, then across the perineum to the opposite side. The incision is brought upward on the opposite lateral margin of the labium to reach the starting point on the mons (Fig. 71–3). A vasopressin 1 : 100 solution is injected along the shallow cut edges of the incision. The incision then is carried into the fat to a depth of approximately 4 to 5 mm (from the surface) (Fig. 71–4A through C). If the clitoris and the labia minora are not involved, they should be preserved. Similarly, if the vestibule is not involved, it should be preserved. The defect created by excision of the labia majora and perineum is covered by a split-thickness skin graft, and a pressure dressing is applied.
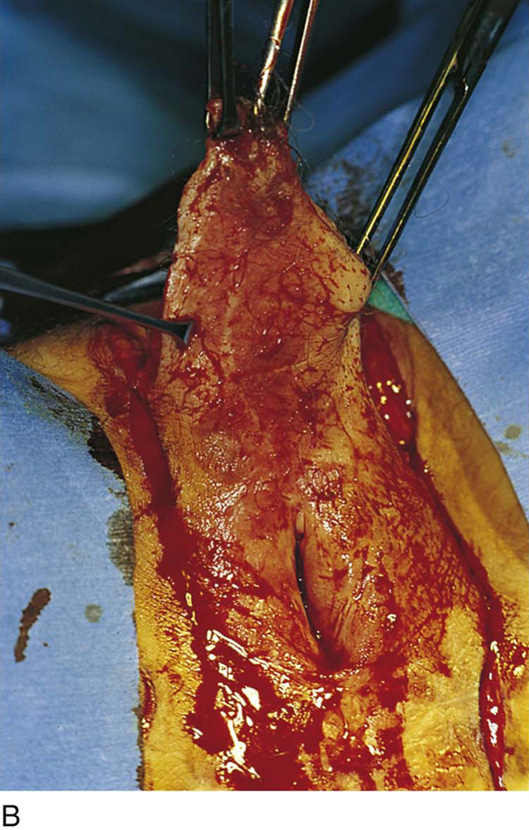
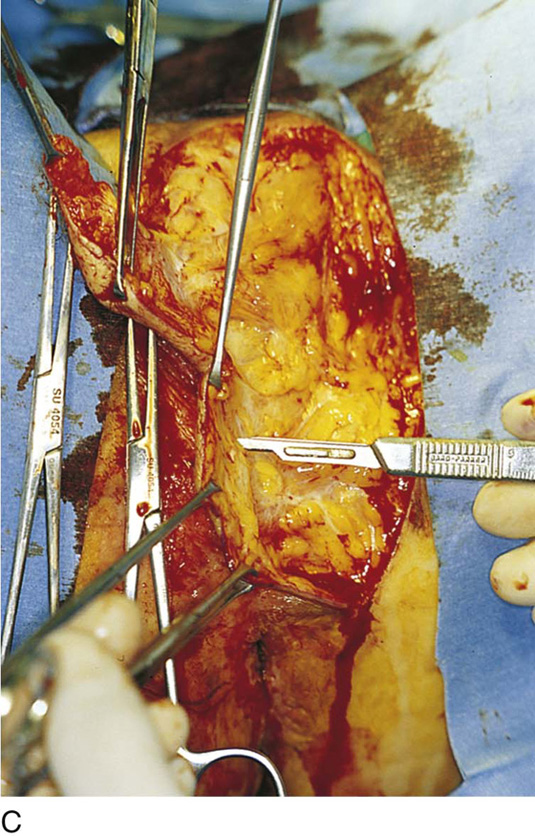
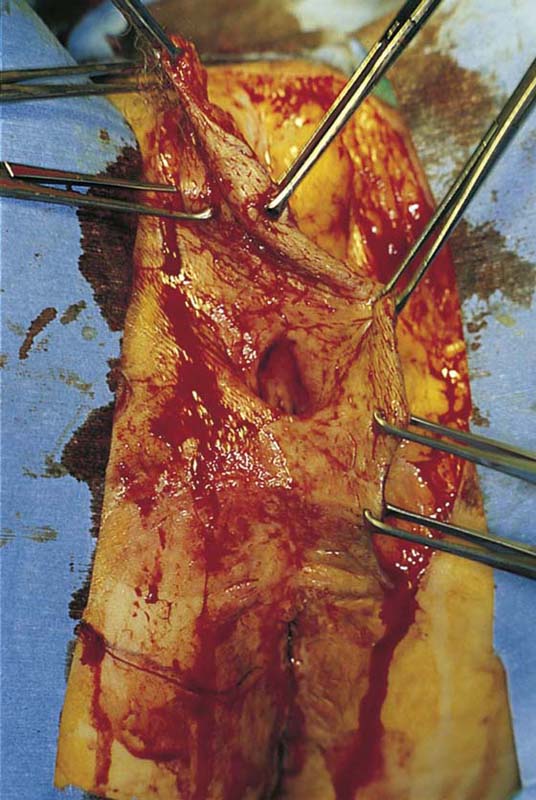
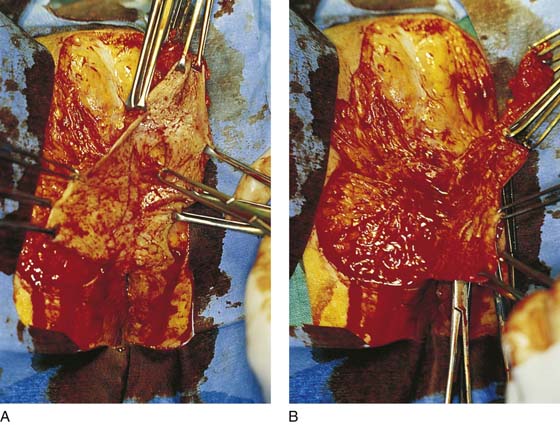
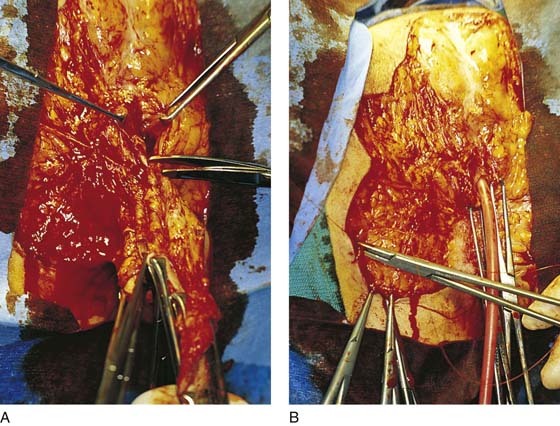
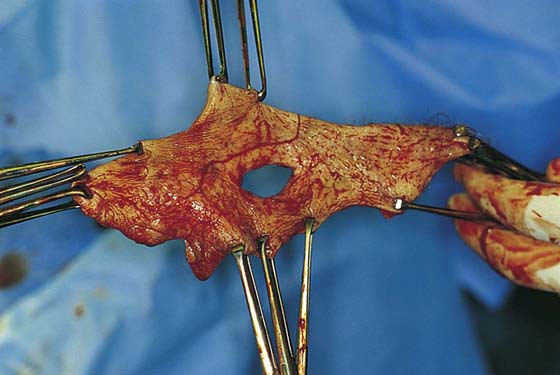
If the labia minora, vestibule, and clitoris are involved in the intraepithelial neoplasia, then excision should include these structures. The depth of incision should not extend below Colles’ fascia (Fig. 71–5). The dissection progresses from above downward and from lateral to medial (Figs. 71–6 through 71–8A). The body of the clitoris should be preserved. If the hood and glans are involved and have biopsy-proven carcinoma in situ, then the glans clitoris, the sheath, and the frenulum should be excised with the labia minora. The body of the clitoris is never exteriorized to simulate any part of the removed glans. Hemostasis is maintained by clamping off any and all bleeding vessels; this is followed by suture ligation with 3-0 Vicryl (Fig. 71–8B). Electrosurgical coagulation and dissection should be avoided in this area because it devitalizes tissue and increases the risk of necrotizing fasciitis. The dissection is carried to the vaginal margin, which is then circumscribed (Fig. 71–9). The specimen is removed (Fig. 71–10).
If primary closure can be accomplished without excessive tension on the suture line, then this type of closure is preferred; otherwise a split-thickness graft should be applied to the defect and sutured medially to the vaginal margins and laterally to the residual skin of the vulva and perineum (Fig. 71–11A through E). Care should be taken not to cause deviation of the axis of the urethra. It is obvious that the surgeon should dissect superficial to the external anal sphincter, perineal muscles, and levator ani muscles during the perineal portion of the vulvectomy. Exposure of muscle indicates that the surgeon has dissected unnecessarily too deep.
Unfortunately, these wounds cannot be practically dressed. The operative site should be covered with Silvadene cream 3 times per day and at bedtime when primary closure has been implemented. When a split-thickness graft has been applied, a pressure dressing consisting of fine-mesh gauze (Xeroform) followed by fluffed 4 × 4-inch sterile gauze pads should be applied and remain in place undisturbed for 1 week (Fig. 71–12). A Foley catheter must be inserted because voiding will be impossible (Fig. 71–13).
FIGURE 71–1 The patient is placed in the lithotomy position. Pneumatic compression boots have been placed on both inferior extremities. The inferior extremities are lightly flexed and minimally abducted. Neither extremity touches the stirrups. The patient’s buttocks are in firm contact with the operating table.
FIGURE 71–2 The vulva is distorted from prior surgery and scar formation. The introitus is shrunken. The vulva shows the characteristic red appearance of Paget’s disease. This diagnosis has been made by preoperative biopsies. A sterile marking pen has traced the outline of the intended excision.
FIGURE 71–3 Light scalpel pressure follows the trace pen lines to again outline the boundaries for excision. A 1 : 100 vasopressin solution is injected subdermally.
FIGURE 71–4 A. The scalpel cuts deeply at the 12-o’clock location into the subcutaneous fat. The edges of the specimen margins are grasped with Allis clamps, and the tissue is pulled outward and slightly inferiorly to create traction. B. The flap is rapidly developed. Hemostasis is maintained by applying mosquito clamps to any bleeding vessel. The margins of the excision are continuously checked. C. The depth of the excisional tissue plane is approximately 4 to 5 mm. Traction and countertraction are exceedingly important to ensure uniform thickness of the tissue that is to be removed.
FIGURE 71–5 The entire upper half of the vulva has been separated from the underlying connective tissue.
FIGURE 71–6 An incision is made circumferentially around the lower vagina. The vestibule is cut away together with a 5-mm margin of lower vagina.
FIGURE 71–7 A. The lower right side of the vulva is dissected to the level of the anal verge. B. The lower left side of the vulva is dissected to the level of the anus.
FIGURE 71–8 A. The last connections of the vagina to the vulva are cut. B. The specimen has been removed. Bleeding sites are sutured (figure-of-8 suture) with 3-0 Vicryl.
FIGURE 71–9 The vagina is grasped with Allis clamps, and the margins are closely evaluated for adequacy.
FIGURE 71–10 The specimen is oriented and sent to pathology. The author prefers to wrap the specimen in a saline-soaked sponge and transport it immediately to the gross pathology laboratory.
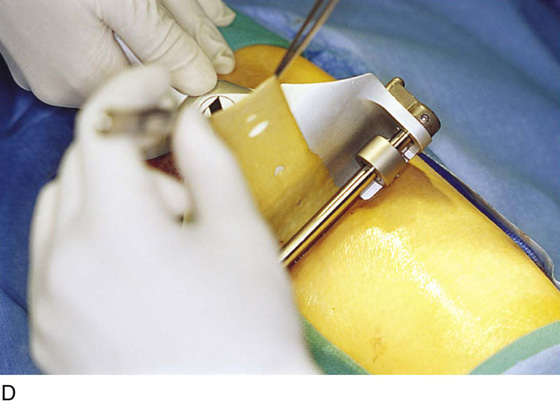
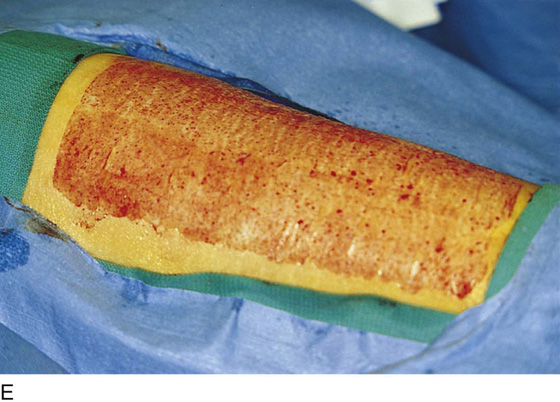
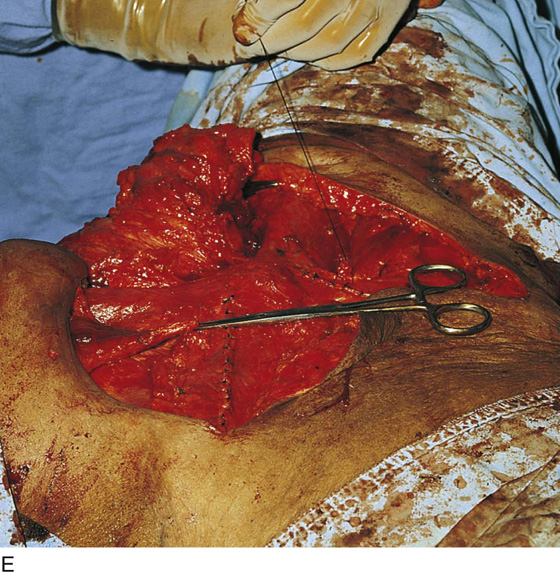
FIGURE 71–11 A. If a skin graft is anticipated, it should be obtained from the patient’s thigh before placement in the lithotomy position. B. The skin is prepared and draped. Sterile saline is injected into the subdermal tissues with a 22-gauge needle and a 10-mL syringe. C. The skin is flattened and the dermatome is applied to the upper margin of the donor site. The blade of the dermatome has been adjusted for the desired thickness of the graft. D. As the skin is cut, an assistant grabs the upper edges of the graft with forceps. E. The donor site is checked for hemostasis, and a urethane dressing is applied. This will remain in place until it virtually disintegrates. F. In this case, the excised area was so large that four pieces of skin graft sutured together with 3-0 and 4-0 Vicryl were needed to cover the wound defect. The edges of the graft were sutured to vaginal, perineal, and anal margins.
FIGURE 71–12 A Foley catheter has been placed in the urinary bladder. Fine-mesh Xeroform gauze is applied directly to the grafted skin.
FIGURE 71–13 A uniform pressure dressing consisting of fluffed 4 × 4-inch gauze pads and Corlex is taped into place. This will remain in place for at least 1 week.
Radical Vulvectomy
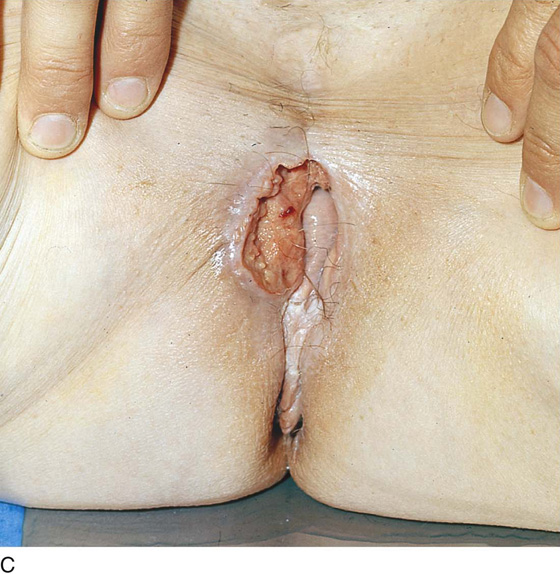
Radical vulvectomy, which is usually combined with bilateral groin dissections (lymphadenectomy), is performed for the treatment of invasive cancer of the vulva (Fig. 71–14A through C). The principles of this operation are to deeply resect the tumor with wide peripheral margins and to extend the zone of resection to the vaginal and anal mucosa. This is coupled with an en bloc resection of the superficial inguinal and deep femoral lymph nodes. For large tumors, the iliac lymph nodes are also removed.
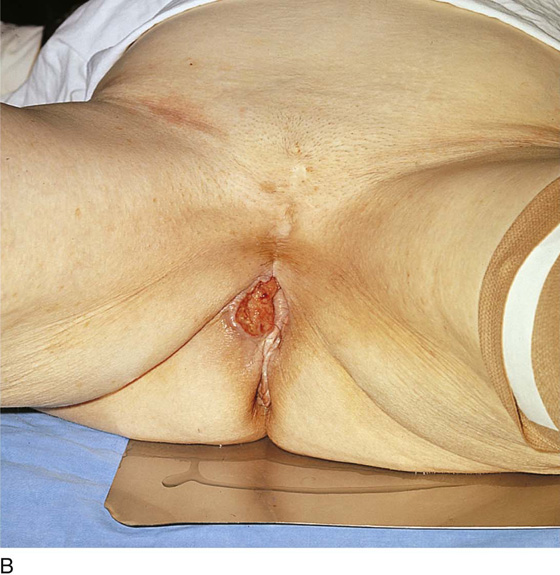
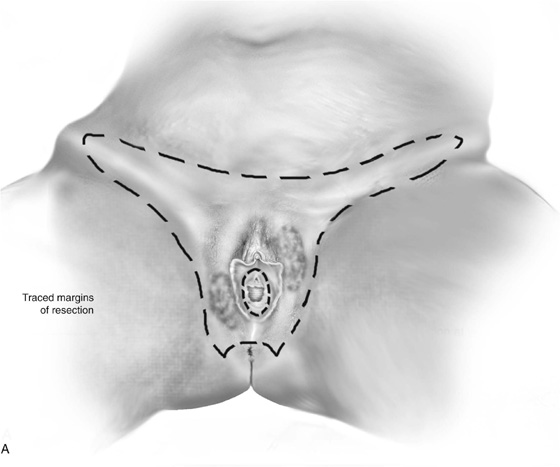
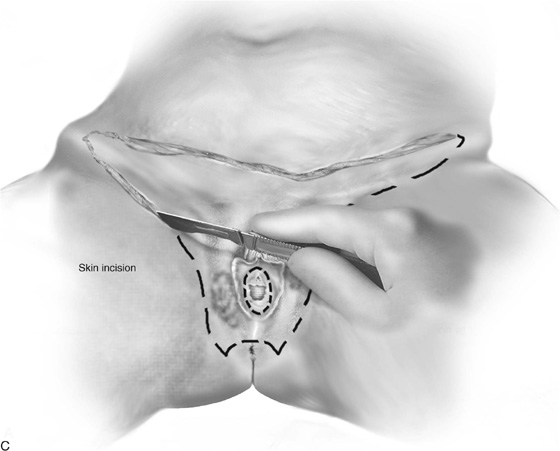
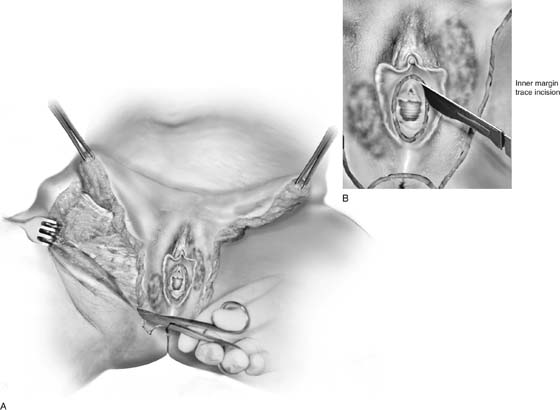
The patient is placed in Allen leg and foot supports in a position similar to that used for operative laparoscopy (Fig. 71–15). The inferior extremities are placed in compression boots. The patient is given a prophylactic antibiotic 1 hour before surgery. With a marking pen, the margins of resection are traced (Fig. 71–16A, B). The incisions are cut transversely across the lower abdomen just above the symphysis and curving upward to the anterior superior iliac spine (i.e., parallel to the inguinal ligament) (Fig. 71–16C). Then the incision is carried downward and medially on the thigh side of the inguinal ligament and over the femoral triangle to the mons veneris (Fig. 71–17A). The incision is continued in a fashion identical to that described for simple vulvectomy (i.e., arcing peripherally around the lateral margin of the labia majora, perineum, and perianal skin). The inner margin of the cut is made into the vestibule at the hymenal ring (Fig. 71–17B).
FIGURE 71–14 A. The large fungating mass destroyed the entire right labium majus and extended laterally to the crura (thigh) and inferiorly into the ischiorectal fossa. A biopsy of the lesion confirmed the diagnosis of invasive squamous cell carcinoma. B. Although less impressive than the cancer shown in Figure 71–14A, nevertheless this is a rather large malignancy involving the right side of the vulva and the clitoris. In this case, the entire clitoris must be removed. C. A magnified view of Figure 71–14B reveals that this lesion extended across the midline to involve the left side of the vulva as well as the right side.
FIGURE 71–15 The patient is positioned for a combined abdominal and perineal approach. Her inferior extremities are placed in Allen stirrups, and compression hose are applied to the legs.
FIGURE 71–16 A. The extent of the dissection is traced with a sterile marking pen. B. The tracing encompasses incisions over the inguinal ligaments to the anterior superior iliac spine and circumscribes the vulva with generous margins, particularly around the gross lesion. C. A knife cut is made through the skin into the fat while following the tracing that was made previously. Flaps will be developed in the groin as the dissection progresses.
FIGURE 71–17 A. The groin fat is excised from lateral to medial. The saphenous vein is located and traced cranially to the cribriform fascia and fossa ovalis. The femoral vein is located, and all nodal tissue overlying and between the femoral vessels is excised. B. At a convenient time, the margin of separation between the vulva and the vestibule or between the vulva and the vagina is gently marked with a shallow scalpel cut.
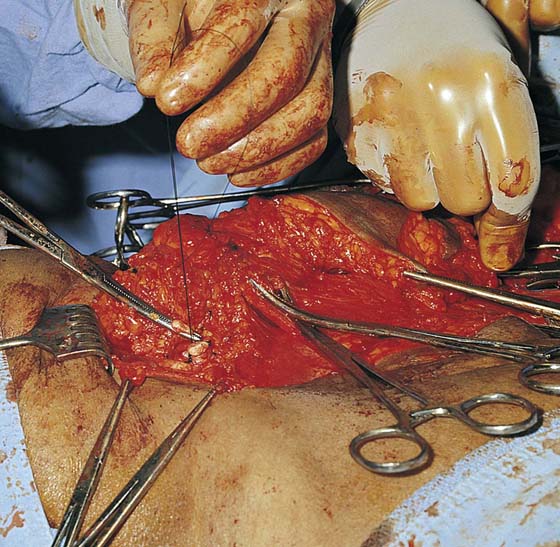
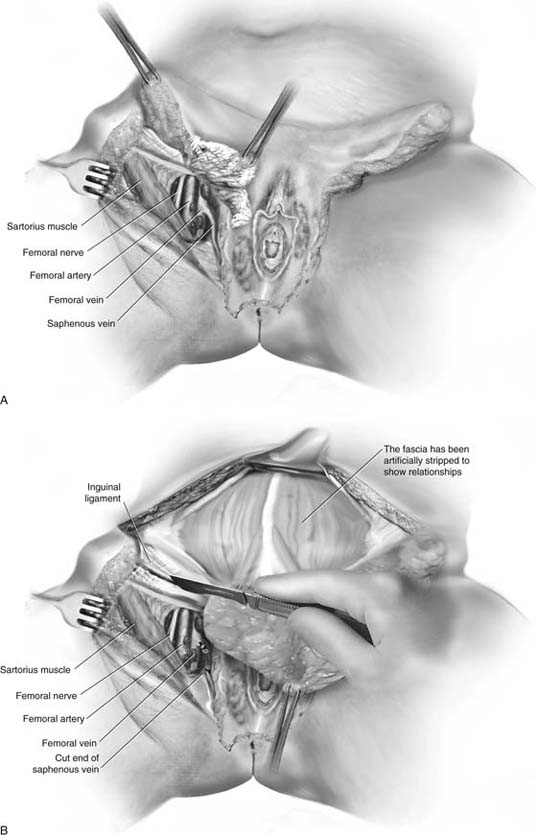
The deeper dissection is initiated at the level of the abdomen and is continued over the femoral triangle. The fatty tissue containing the superficial nodes is swept downward, clearing the fat from the investment fascia covering the rectus and external oblique muscles and exposing the inguinal ligaments (Fig. 71–18). The sartorius fascia (fascia lata) and muscle are exposed, and the node-bearing tissue is dissected downward (caudally) to the depth of the underlying fascia lata (Fig. 71–19A). The node dissection proceeds medially toward the saphenous vein. In turn, the femoral nerve, femoral artery, and upper saphenous vein are dissected free of fat, lymph nodes, and connective tissue (see Fig. 71–22). The cribriform fascia covering the fossa ovale has been exposed and dissected away. The saphenous vein is divided above its junction with the femoral vein (Fig. 71–19B). The vein again is ligated at the lower portion (apex) of the femoral triangle because a segment of this vein is included with the lymph node and fat specimens. The small branches of the femoral artery and the tributaries of the femoral vein have been clamped, cut, and suture-ligated with 3-0 Vicryl as they are encountered. If deep pelvic node dissection is to be performed, it is done at this point by excising over the inguinal ligament, locating the iliac vessels, and carrying out the dissection as described previously for radical hysterectomy (see Chapter 12) (Fig. 71–20A, B). When this has been completed, the incision above the inguinal ligament (at the level of the aponeurosis of the external oblique muscles) is closed with 0 Vicryl sutures (Fig. 71–21). Whether or not deep node dissection is carried out, the lowest external iliac node should be extricated and sampled. This is Cloquet’s node (Fig. 71–22).
The femoral vessels are now completely exposed (Fig. 71–23). It is worthwhile to transplant the sartorius muscle to cover these vessels and provide a modicum of protection for them (Fig. 71–24A). The muscle is easily separated via curved Mayo scissors from its origin on the anterior superior iliac spine. Next, the muscle is freed from its bed for a distance of 2 or 3 inches and is swung medially to cover the femoral vessels (Fig. 71–24B through D). The free end of the sartorius muscle is sutured onto the inguinal ligament with 0 Vicryl or polydioxanone (PDS) sutures (Figs. 71–24E, F and 71–20A).
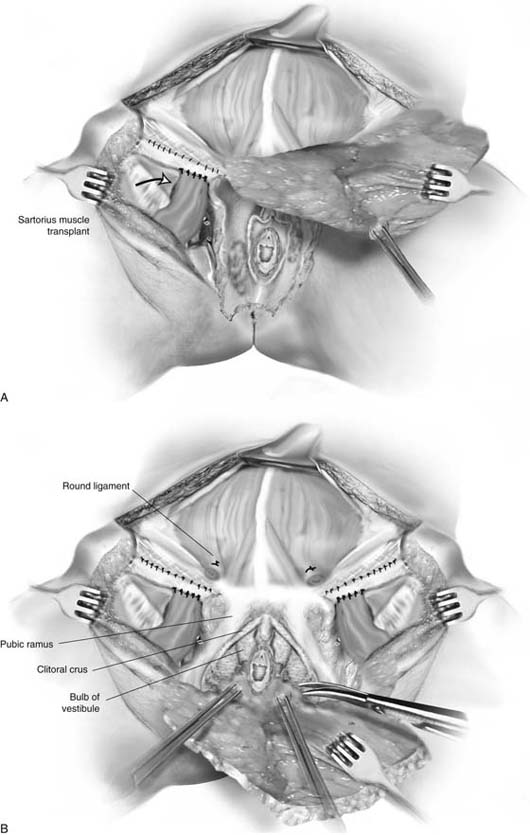
Attention is directed to excising the vulva proper (see Figs. 71–20 and 71–25). The incision at the superior portion of the mons is extended on the right and left sides. The mons fat, including the suspensory ligament of the clitoris, is dissected free and cut away from the symphysis pubis (see Fig. 71–20B). Care is taken not to injure the urethra, the clitoral crus, or the bulb of the vestibule. The deep plane of this vulvar dissection is carried out above the tough membrane covering the corpora cavernosa, the bulb, the levator fascia, and the clitoral body (see Fig. 71–25). The dissection will remove the bulbocavernosus, ischiocavernosus, and transverse perineal muscles, as well as Colles’ fascia (Fig. 71–26A through C). A small portion of the clitoral body and the glans clitoris will be removed. The urethra and the lower vagina are left intact. Thus, the medial incision is made circumferentially around the vaginal outlet above the urethra and between the urethra and glans clitoris (see Figs. 71–25 and 71–27).
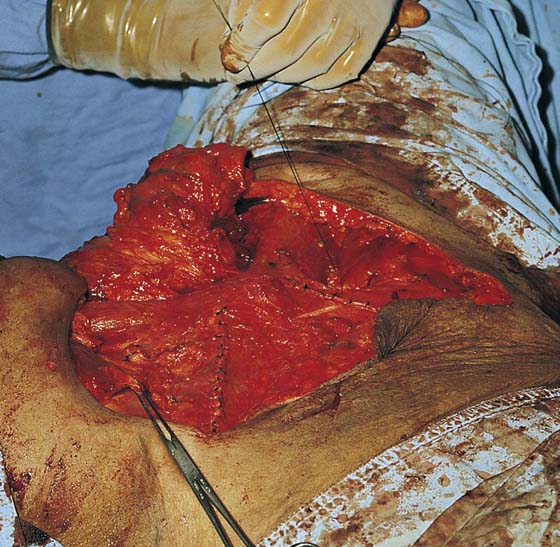
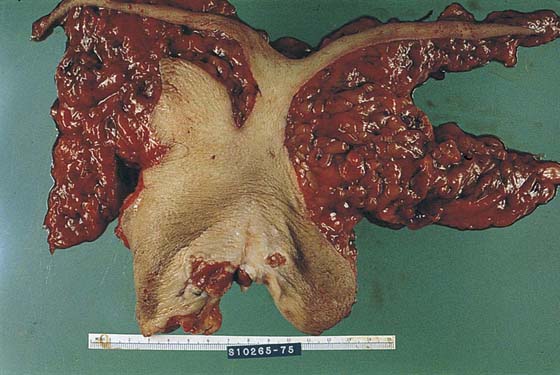
The final dissection is made to separate the vulva from the retained vestibule or vagina (see Fig. 71–25). The perineum is dissected with the specimen, but the anal sphincter and levator ani muscles are not disturbed. During this portion of the dissection, the pudendal vessels are secured and cut. These vessels are suture-ligated with 3-0 Vicryl sutures after adequate hemostasis has been obtained. The wound is now ready to be closed. The specimen is oriented and soaked in saline sponges and then is sent intact to pathology (Fig. 71–28). Closure is made per primum if possible but never under excessive tension. Tension closures result in wound separation and tend to then heal by granulation (i.e., secondary intention). This delayed healing is not optimal and results in prolonged hospitalization (Fig. 71–29).
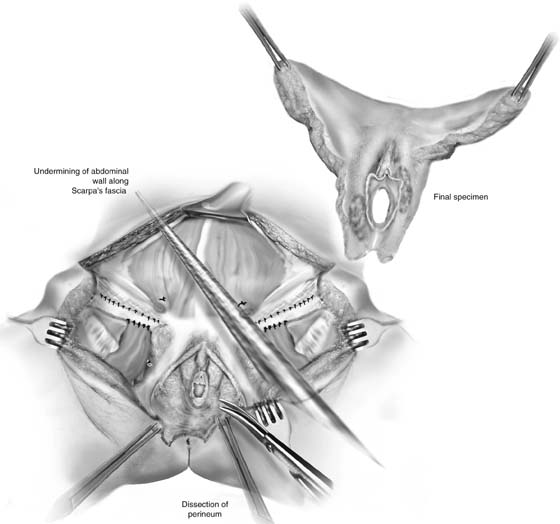
The abdominal wall may be mobilized by bluntly dissecting along Scarpa’s fascial plane up to the navel and pulling downward on the anterior abdominal wall (Fig. 71–30). If the vulvar wound cannot be closed adequately, a skin graft should be applied. Jackson-Pratt drains are placed under the groin flaps, anchored to the skin with 3-0 Vicryl, and attached to suction bags (Fig. 71–31). The subcutaneous tissue is sutured with 3-0 Vicryl interrupted sutures and is approximated above the drains. The skin is closed with 3-0 nylon or PDS interrupted sutures. The vestibule is sutured to the remaining perineal skin with interrupted 3-0 Vicryl sutures. The inferior extremities should be kept elevated to enhance lymphatic drainage (wrapped in elastic bandages or pressure stockings) during the postoperative course. If a graft is required, a pressure dressing should be placed. The Foley catheter is attached to a drainage bag to monitor urine output.
FIGURE 71–18 The superficial and deep nodes are dissected and swept inferiorly and medially. Small branches and tributaries of the femoral vessels are clamped with tonsil clamps and are suture-ligated with 3-0 Vicryl.
FIGURE 71–19 A. The sartorius muscle, femoral nerve, femoral artery, and femoral vein are cleared. The tough fascial sheaths are excised. B. The saphenous vein is clamped above the lower portion of the femoral triangle. It is excised with the fat to the point where it flows into the femoral vein. At this location it is clamped, double suture-ligated with 3-0 Vicryl, and cut.
FIGURE 71–20 A. If a pelvic node dissection is to be performed, the aponeurosis of the external oblique is incised along the inguinal ligament. The external iliac vessels are located, and a lymphadenectomy is performed. B. The inguinal ligaments have been sutured. The sartorius muscles have been transplanted. Colles’ fascia has been excised, exposing the tough membranes covering the “blood lake” (corpora cavernosa, clitoral body, and bulb of the vestibule). The vulva is in the process of being separated from the vestibular remnant.
FIGURE 71–21 The sartorius muscle is grasped with an Allis clamp. The deep node dissection is complete, and the inguinal ligament has been sutured.
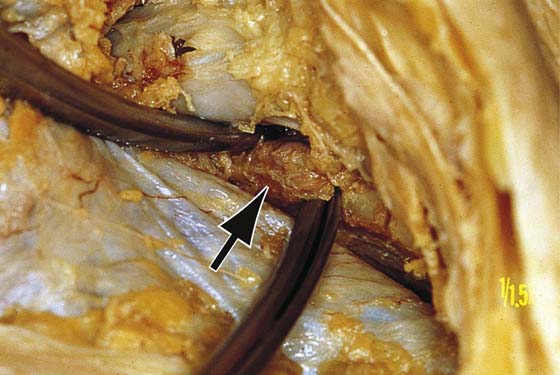
FIGURE 71–22 Cloquet’s node is seen at the arrow. The clamp is at the lower pole of the node. This would correspond to the upper part of the femoral canal. The scissors are under the femoral vein (bluish tint).
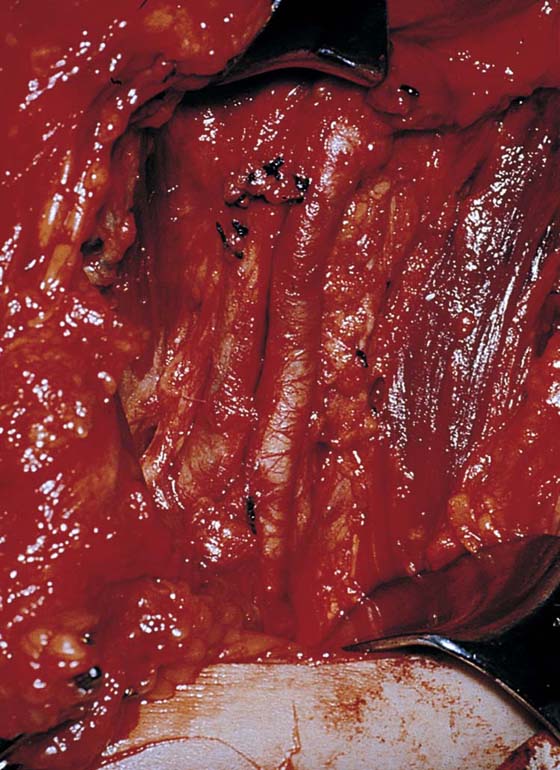
FIGURE 71–23 The dissected femoral vessels devoid of fat and fascia are exposed and at risk for injury. The sartorius muscle is located to the right in this photo.
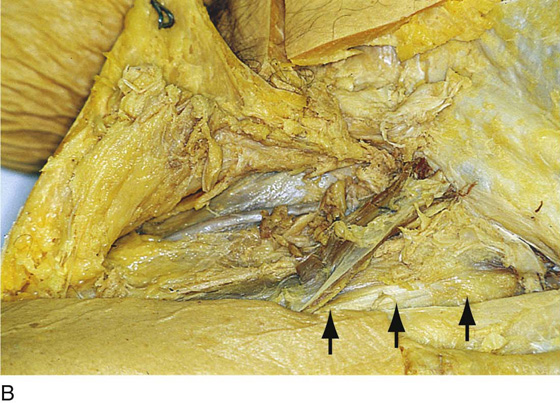
FIGURE 71–24 A. The instrument points to the sartorius muscle. The inguinal ligament is above it, coursing obliquely toward the pubic bone. B. The bed of the sartorius muscle is indicated by the arrows. The muscle has been detached from the anterior superior iliac spine and transposed to cover the femoral vessels. C. The original location of the sartorius muscle lies between the two instruments. The scissors (upper) point to where the muscle was cut free from its insertion on the anterior superior iliac spine. D. Magnified detail of the sartorius transposition to cover the femoral vessels. The cut end of the muscle will be sutured to the inguinal ligament. E. The sartorius muscle has been freed from its bed and insertion into the iliac spine. It has been moved medially and is held in the clamp. F. The sartorius muscle has been sutured to the inguinal ligament.
FIGURE 71–25 The specimen has been excised. To facilitate skin closure, the abdominal wall is undermined over Scarpa’s fascia. The abdominal wall can then be mobilized to approximate the cut groin and vulvar skin margins.
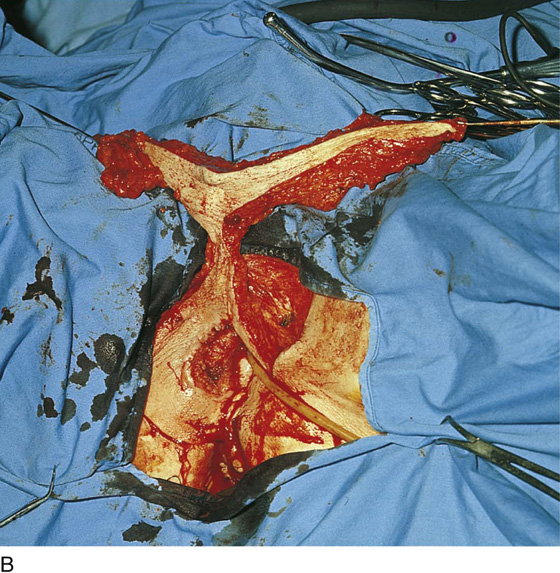
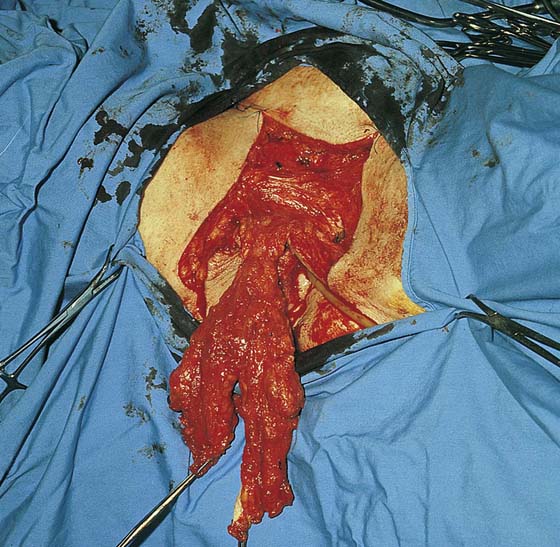
FIGURE 71–26 A. This details the final steps in separating the vulva from its underlying attachments and cutting the vestibule (or vagina) free. B. The specimen is held up for orientation. The vulva must be freed from the perineal skin and connective tissue. C. This details the final stages of the vulvectomy. The vulva has been separated superiorly and laterally.
FIGURE 71–27 The specimen hangs to the perineum by a thin bridge of tissue.
FIGURE 71–28 The specimen has been deeply and widely excised. The node-bearing fat is attached, and the specimen is sent en bloc to pathology.
FIGURE 71–29 If the wound edges are approximated under tension, the edges will separate, resulting in prolonged healing by second intention.
FIGURE 71–30 The wound edges are approximated. The vaginal margin has been sutured to the perineal and thigh skin margins.
FIGURE 71–31 The flaps came together nicely in this case. Jackson-Pratt drains have been placed under the flaps.