Vulvar Hematoma
Hematomas occurring in the vulva may result from a variety of causes: episiotomy, traumatic forceps delivery, therapeutic vulvar or lower vaginal injection, vulvar surgery, and vulvar trauma, to mention a few.
Regardless of the cause(s), the end result may be the deposit of a massive amount of blood subcutaneously, typically along the plane of Colles’ fascia or below it (Fig. 73–1). Coupled with the factors previously noted may be disruption of one of the structures forming the “blood lake” situated between Colles’ fascia and the fascia encompassing the levator ani muscles. These cavernous structures (clitoris, bulb and vestibule, and corpora cavernosa) can and will bleed without remission for long periods, as manifested by a constant slow ooze.
Pressure of the blood on the vulvar skin may compromise its blood supply, causing actual necrosis. Therefore, when this condition occurs, the hematoma must be drained to relieve the pressure. Before it reaches a state necessitating surgical intervention, bleeding may be controlled by the timely application of an ice pack to the lesion, as well as by postural drainage. After the first 6 to 8 hours, the patient will benefit from warm salt water tub soaks (Fig. 73–2A, B).
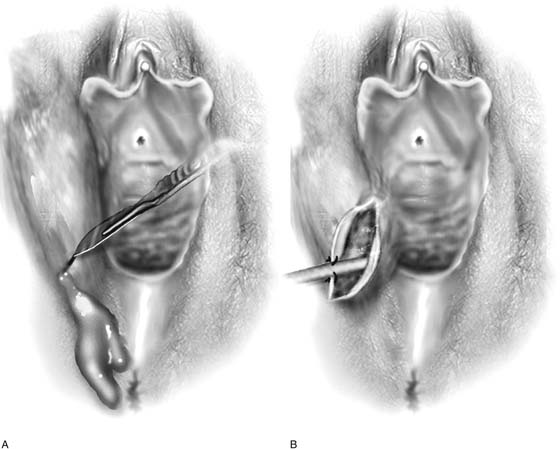
Drainage may be implemented by a small incision at the most dependent portion of the hematoma. After the incision is made, the edges of the wound are sutured with a running stitch of 3-0 Vicryl. The hematoma is compressed every 3 to 4 hours to promote drainage (Fig. 73–3).
Exploration to locate the bleeding site should be done only as a last resort because it is exceedingly difficult to find the bleeding vessel in the midst of the substantial clot and tissue edema.
FIGURE 73–1 Massive vulvar hematoma. Note that the blood has dissected so as to involve the right labium minus, labium majus, perineum, and mons. It has in fact extended to the contralateral labium majus. Dissection has progressed along a plane above Colles’ fascia.
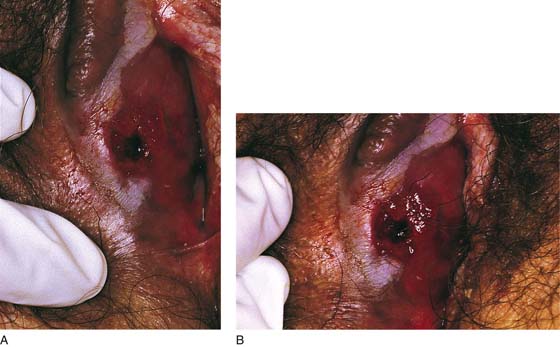
FIGURE 73–2 A. This hematoma occurred after a vestibular injection with a 27-gauge needle. The blood created tremendous swelling of the vestibule, perineum, and labium majus. The drainage site is noted in the lower right vestibule. B. Magnified view of drain site. The Penrose drain was removed 72 hours after drainage. The patient was admitted and catheterized for 24 hours. She was sent home with instructions to take salt water tub baths 3 times daily.
FIGURE 73–3 A. The drawing illustrates a hematoma that is drained at its dependent portion. A 1.5- to 2-cm hole is placed through the skin into the hematoma. B. A 0.25-inch Penrose drain is placed in the space, and its margins are anchored to the skin edges with 3-0 chromic catgut sutures. A large safety pin is placed through the terminal portion of the drain.