Vulvar Biopsy
A number of techniques have been reported that use vulvar biopsy. Regardless of the technique selected, the vulvar skin, unlike the cervix, has many pain receptors, and biopsy specimens cannot be taken without the aid of local anesthesia. Injection of 1% lidocaine with a 27-gauge needle will create sufficient anesthesia to permit the biopsy to be done painlessly. The injection discomfort itself may be significantly diminished by having the patient apply EMLA cream 30 minutes before the anticipated injection.
Dermatologists prefer to use a dermal punch and scissors for biopsies. The major advantage of the punch relates to the fact that it creates a flat disc sample that is easy for the pathologist to orient. This type of sample therefore is unlikely to result in a tangential tissue section.
After the creation of adequate anesthesia (objectively tested by squeezing the site with toothed forceps), the skin is flattened with one hand, and the sharp punch is applied and twisted back and forth two or three times until a full-thickness cut has been made through the skin (Fig. 65–1A, B). Next, with a fine forceps, the skin disc is elevated and its base cut away from surrounding fat and connective tissue (Fig. 65–2A through C). The sample is placed into fixative and transported to the pathology laboratory. The biopsy site is compressed with a sterile sponge and then is closed with two or three interrupted Vicryl sutures.
The dermal punch may be omitted by elevating the piece of skin to be biopsied and then simply cutting it off at the base with scissors or a knife (Fig. 65–3). As with the dermal punch technique, this requires the placement of sutures for hemostasis.
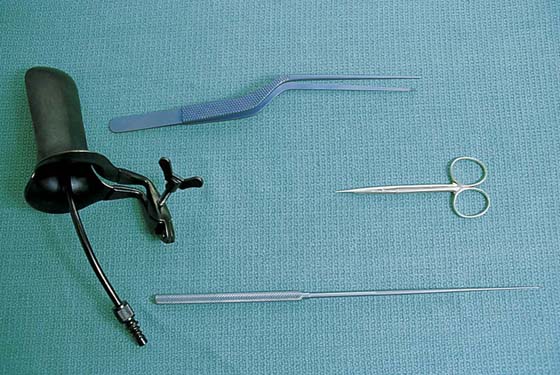
The least complex method for sampling vulvar skin is the punch biopsy technique. The same biopsy instrument used for the cervix and vagina is applied to the vulva. After the specimen is obtained, the biopsy skin defect is touched with Monsel’s solution (ferric subsulfate) to stop bleeding (Fig. 65–4A through E).
The use of electrosurgical devices (e.g., loop electrodes) to perform a skin biopsy is decried because thermal injury devitalizes the skin and slows healing; it also increases the risk of infection. The same argument may be made when the use of Monsel’s solution is discussed. Here, the amount of caustic Monsel’s solution is a critical factor in that a large glob of the solution will retard healing and devitalize tissue, whereas a sparing application will not have significant detrimental actions.
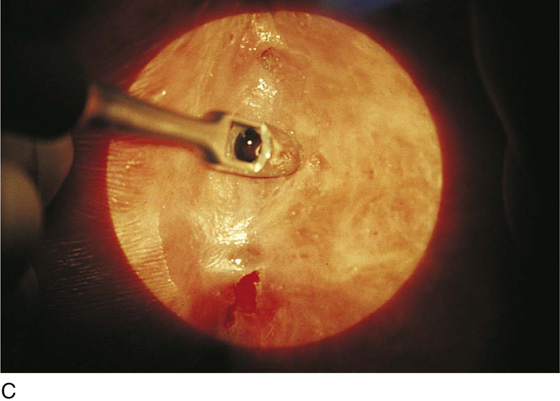
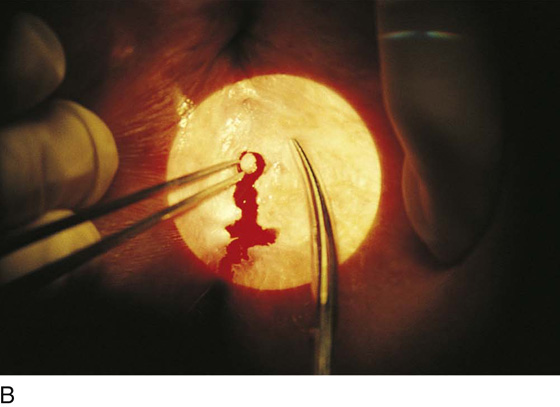
FIGURE 65–1 A. The vulva pictured here shows several areas suggestive of carcinoma in situ. These include flat warts and pigmented warty areas. B. The vulvar skin is anesthetized with a local anesthetic. The skin is flattened. The dermal punch is applied over the area of skin that will be subsequently sampled. C. The punch is rotated back and forth two or three times.
FIGURE 65–2 A. The disc of skin that has been cut by the sharp edge of the punch is now elevated with forceps. B. The disc is cut free from its base with fine, sharp scissors. C. After the specimen is separated from the surrounding skin, it is placed in fixative. If necessary, one or two 3-0 Vicryl sutures are placed for hemostasis.
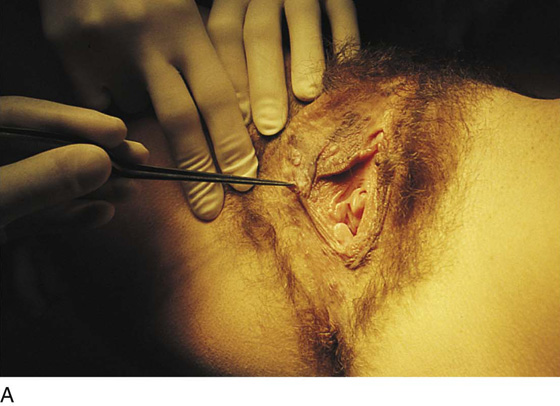
FIGURE 65–3 Another technique for biopsy utilizes a forceps or hook and a fine scissors. The skin to be sampled is elevated by a hook or forceps. The scissors snip across the base of the elevated skin, and the specimen is removed. As with the dermal punch technique, one or two stitches may be required for hemostasis.
FIGURE 65–4 A. A punch biopsy forceps grabs the anesthetized tissue, much in the same manner by which vaginal and cervical specimens are obtained. B. The biopsy clamp closes on the tissue and cuts out an oval piece of tissue. C. A dry cotton-tipped applicator is placed into the wound to maintain hemostasis. D. Next, a swab impregnated with Monsel’s solution is placed into the wound and held for 15 to 20 seconds. E. When the vessels have been coagulated by Monsel’s solution, the swab is removed. The wound is dry.