Vulvar and Perineal Anatomy
The external genitalia in the female are homologues to structures in the male. The former are unfused, the latter are fused.
The labia majora are homologous to the scrotum; the labia minora, to the median raphe of the penis and scrotum. The glans clitoris, clitoral body, and corpora cavernosa clitoris are direct homologues to equivalent penile structures in the male. The hood of the clitoris and the penile foreskin are likewise of similar origin.
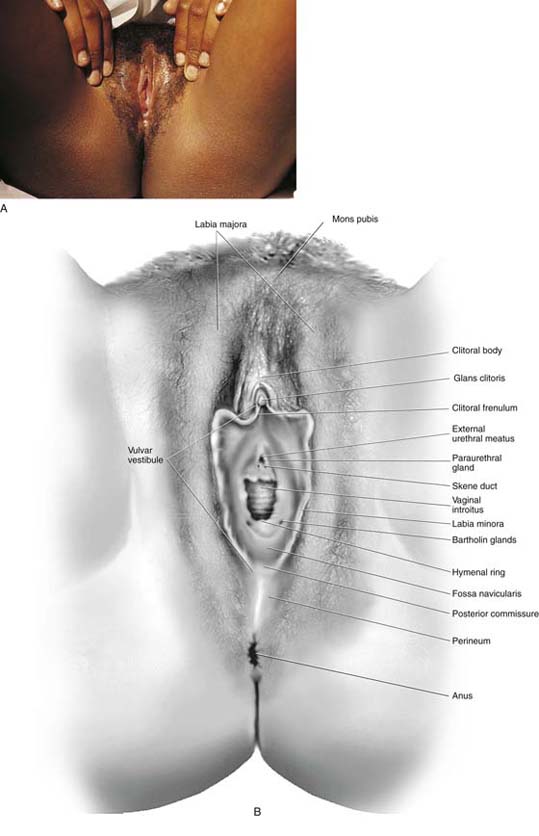
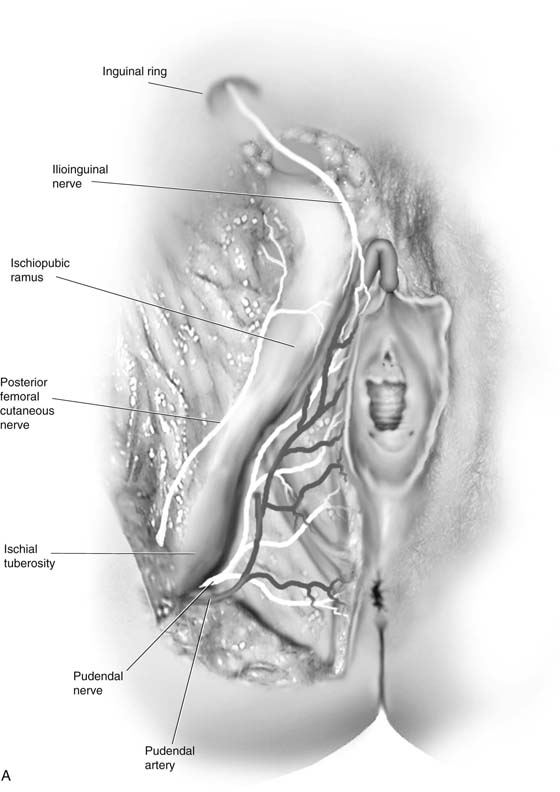
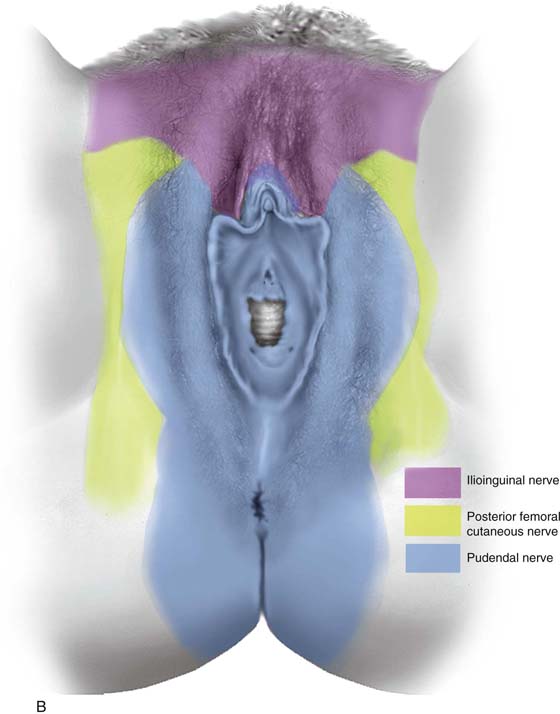
The labia majora consist of skin and appendages, including hair follicles, sebaceous glands, and sweat glands, and create two prominent swellings on either side of the vulva. Subdermal fat deposits produce these bulges (Figs. 64–1A, B and 64–2). The prominence diminishes with age as the fat atrophies. Superficial branches of the pudendal artery supply the labia, and branches of the pudendal, ilioinguinal, genital femoral, and femoral cutaneous nerves supply the neural components (Fig. 64–3A through E).
The labia minora contribute to the structure of the clitoral frenulum and sheath (Fig. 64–4A, B). These structures contain no hair follicles but are copiously supplied with sebaceous glands and sweat glands. The labia are sites for specially adapted large sweat glands, the apocrine glands. These are also present in the perineum and perianal skin.
The area bounded anteriorly by the clitoral frenula, laterally by the medial aspects of the labia minora, and posteriorly by the fossa navicularis and posterior commissure constitutes the vulvar vestibule (see Figs. 64–1B and 64–5A). The external urethral meatus opens into the vestibule, as does the vaginal introitus. The hymenal ring frames the vaginal opening and is considered to be a portion of the vestibule (Fig. 64–5B). Additionally, several mucous glands open into the vestibule [Bartholin (major vestibular), minor vestibular, Skene ducts, paraurethral] (see Figs. 64–1B and 64–5C, D).
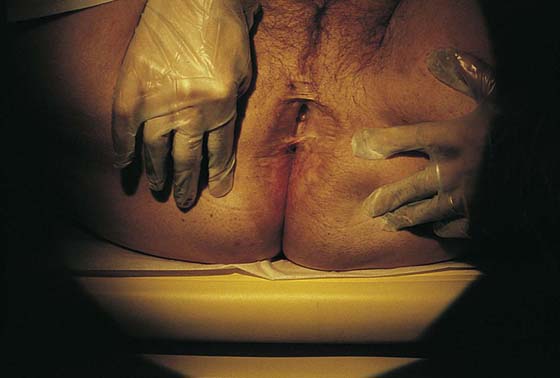
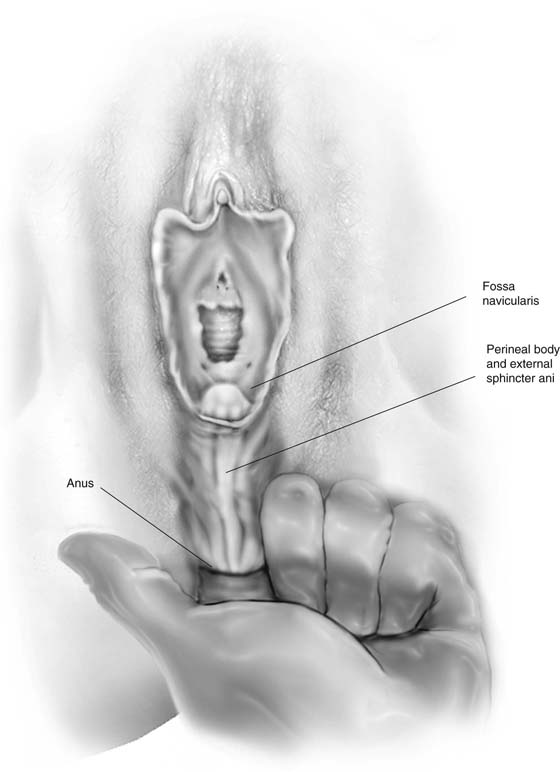
Below (caudad to) the external genitalia lies a flattened area extending between the anus and the lower portions of the labia majora and posterior commissure (Fig. 64–6). This region is referred to as the perineum, although the term also may encompass the whole area from the mons to the anus to the medial aspects of the buttocks and junction with the thighs. The perianal skin and anus constitute a part of the perineum and have much in common with the rest of the vulva (Fig. 64–7).
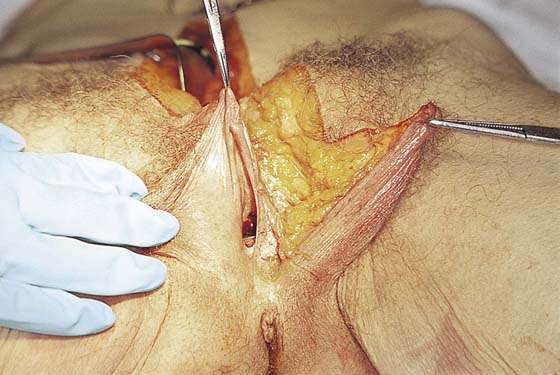
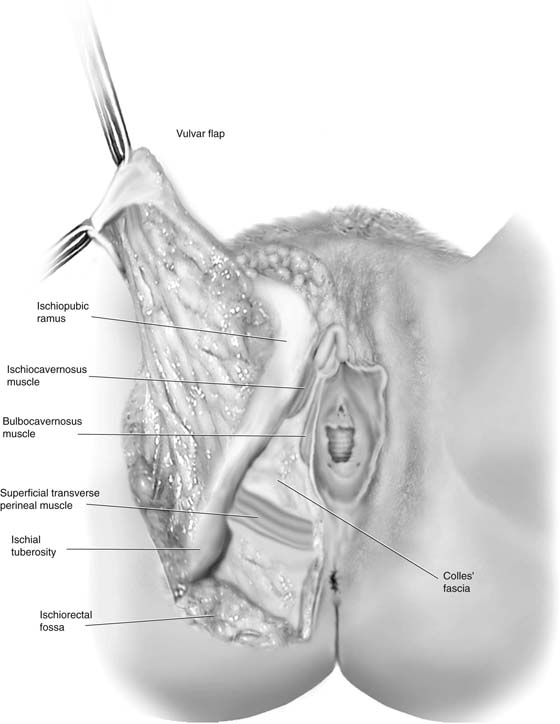
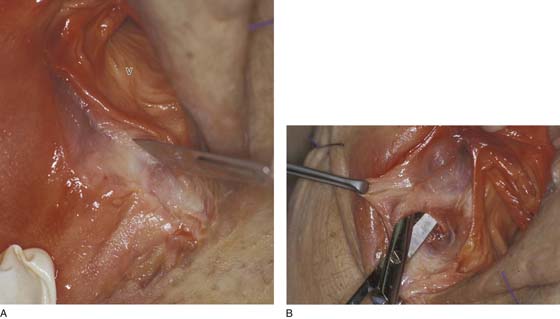
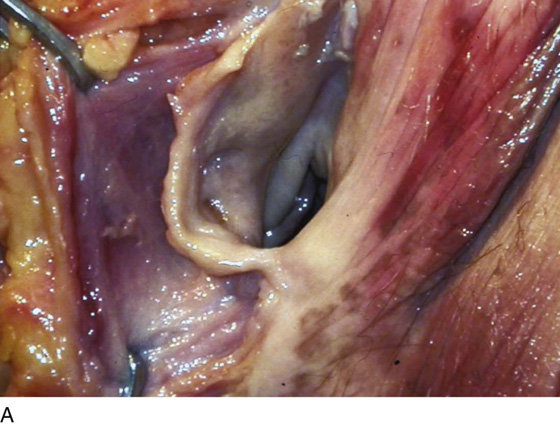
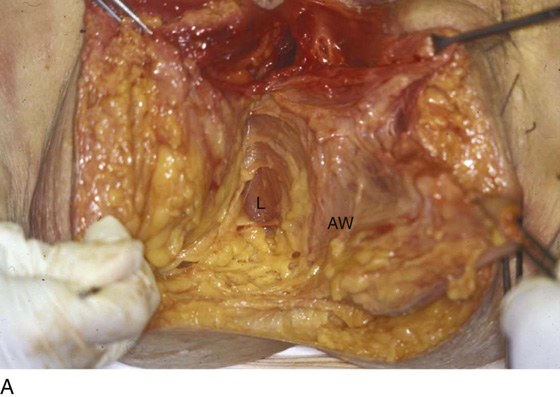
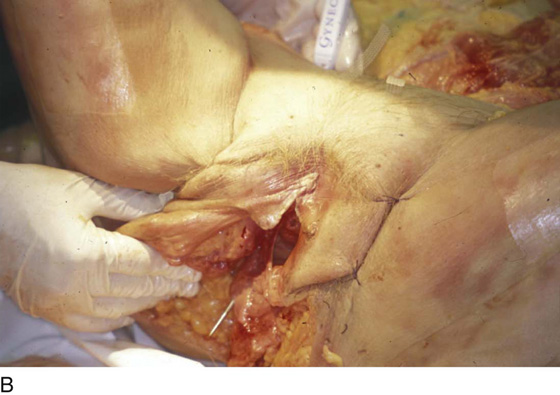
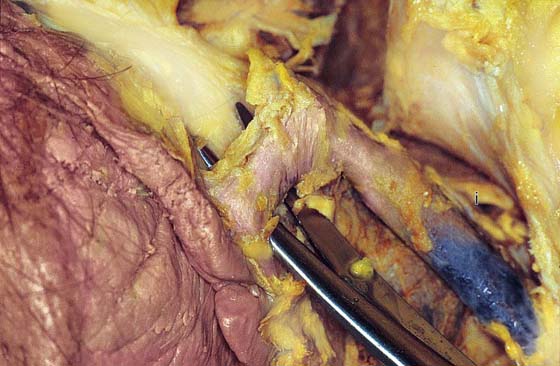
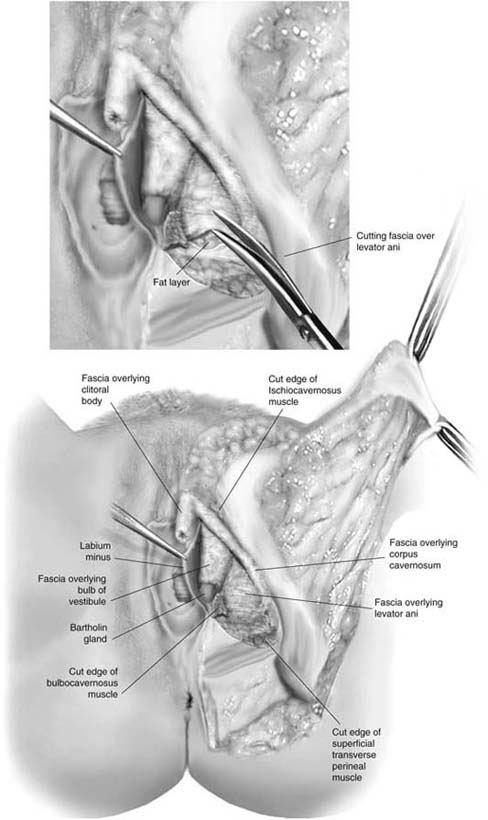
A flap may be cut to expose the underlying anatomy by incising from the top of the mons through the right or left interlabial sulcus to the perineum above the perianal skin. The flap is then cut from medial to lateral and is reflected laterally (Fig. 64–8). Ninety-five percent of the tissue beneath the skin of the labia majora is fat, through which course superficial vessels and nerves (branches of internal pudendal and pudendal) (Fig. 64–9). A membranous condensation of fat is located superficial to the thin muscles of the urogenital diaphragm. This is Colles’ fascia, which may easily be dissected with the fingers upward over the symphysis and above the inguinal ligament to Scarpa’s fascia of the anterior abdominal wall. Just lateral and juxtapositioned to the hymenal ring beneath the vestibular skin is the bulbocavernosus muscle (Fig. 64–10A, B). During actual dissection, the muscle is thinner than depicted in the schematic illustrations shown in most anatomic texts (Fig. 64–11A through C). The same can equally be said for superficial transverse perineal muscle, which extends anterolaterally from its junction with the bulbocavernosus to the ischial tuberosity (Fig. 64–12A, B). Inferior to the latter muscle is the septated and fat-filled ischiorectal fossa. The fossa borders the anus and rectum medially (Fig. 64–13A through F). The levator ani descends through the ischiorectal fossa peripheral to the external sphincter and rectum (Fig. 64–14A through C). The ischiocavernosus muscle lies directly along the superior ischial ramus partly overlying the corpora cavernosa clitoris (crus). In relative size, the crus dwarfs the muscle (Fig. 64–15). A tough membrane encompasses the clitoral crus, the bulb of the vestibule, and the body of the clitoris. The membrane is tightly adherent to the cavernous vascular structures, which constitute the bulb, clitoris, and corpora (Fig. 64–16). The deep perineum is in fact revealed to be a vascular lake, and the most impressive structures in the deep perineum are these cavernous vascular structures. The cavernous structures impart a bluish hue because of the venous blood held within the vascular sinuses (Fig. 64–17A, B). The bulb is closely applied to the lateral aspect of the vaginal wall, which is also honeycombed with large cavernous and venous sinuses. Between the lateral margin of the bulb, the pubic, and the ischial rami is the fascia-muscle complex of the levator ani (Fig. 64–18). Similarly, the urethra is covered by an umbrella-like mass of cavernous tissue emanating from the bulb of the vestibule (Fig. 64–19A, B). The urethra, vagina, and cavernous structures are intimately applied to one another immediately below and at the urethrovesical junction (Fig. 64–20).
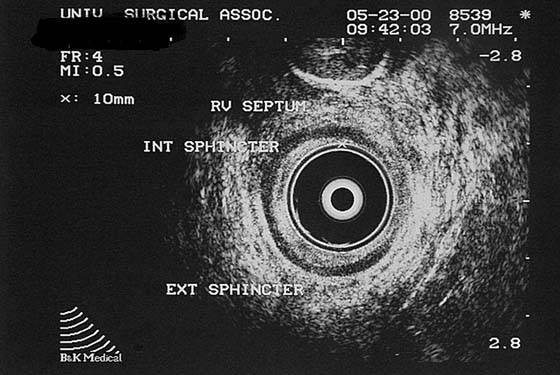
The anal opening is below the perineum. The course of the anus/rectum is upward (cephalad), deep to the broad anal sphincter and perineum, to situate itself 3 to 4 mm beneath the fossa navicularis and the lower vagina. The rectum is located in the posterior midline directly beneath the perineum (see Fig. 64–20). The space between the perineal and vestibular skin surfaces and the rectum depends to a great extent on the development, mass, and integrity of the perineal body and the anterior sphincter ani muscle (Fig. 64–21). At the point where the rectum reaches within a few millimeters of the posterior vagina, it parallels the vagina and follows a posterior and cephalad course (Fig. 64–22). The vagina may be freed from the rectum by careful incision and dissection of the rectovaginal septum from below upward, or by entry into the rectouterine space from above.
FIGURE 64–1 A. The labia majora form two prominent swellings that are produced by fat deposits lying between the dermis and Colles’ fascia. These hair-bearing areas are rich in sebaceous glands, hair follicles, and sweat glands. B. This panoramic view of the vulva details the outermost areas, consisting of the mons (anteriorly), the labia majora (laterally), and the perineum (posteriorly). The innermost portions consist of the labia minora, the vestibule, the hymenal ring, the clitoral hood, and the glans clitoris. The clitoral body lies deep to the glans clitoris and is suspended from the pubic symphysis by a ligament.
FIGURE 64–2 The fresh cadaver specimen illustrates labial atrophy secondary to fat mobilization and deterioration following menopause.
FIGURE 64–3 A. The vascular and neural supply to the vulva emanates from the internal pudendal artery (perineal branches) and from the pudendal nerve as they emerge from Alcock’s canal and from beneath the ischial tuberosity. The posterior femoral cutaneous, ilioinguinal, and genital femoral nerves also supply portions of the vulva. B. The pink areas (mons, upper labia majora) are supplied by the ilioinguinal and genital femoral nerves. The yellow crural areas are supplied by the posterior femoral cutaneous nerves. The remainder of the vulva and the perianal skin are supplied by the pudendal nerves. C. The tip of the scissors points to the external inguinal ring. The genital femoral (genital branch) and ilioinguinal nerves emerge in the fat, accompanied by the round ligament, which itself extends to the labium majus. The external inguinal ring illustrated in this photo is prominent because of the herniated fat emerging from it. D. The scissors are spread beneath the round ligament. The round ligament traverses the mons fat to terminate within the fat of the labium majus. E. The ilioinguinal nerve has been dissected free from the round ligament and surrounding fatty tissue. The branches of the nerve supply the mons skin and the upper aspects of the labia majora.
FIGURE 64–4 A. The labia minora are finely sculpted, hairless folds of skin that enclose the vestibule. The labia minora receive a rich neural and vascular supply and are more sensitive to touch than are the labia majora. B. This photograph illustrates the contribution of the labium minus to the clitoral frenulum and hood. As the labia come together beneath (posterior to) the clitoral glans, they form the upper limits of the vestibule. Note the external urethral meatus opening into the vestibule.
FIGURE 64–5 A. The vestibule is bounded anteriorly by the fused labia minora and the clitoral frenula. Laterally, the vestibular margins coincide with the medial surfaces of the labia minora. The posterior boundary of the vestibule is constituted by the fossa navicularis and the posterior commissure (see also Fig. 64–1B). B. The hymenal ring extends from the lower paraurethral area to the upper margin of the fossa navicularis. It frames the boundary between the vestibule and the entrance to the vagina. C. Paraurethral gland ducts are prominent and are located on either side of the urethral meatus (see also Fig. 64–1B). D. The opening of the left Bartholin gland duct is seen adjacent to the lower lateral aspect of the hymen. The gland is located 12 mm deep to the surface and slightly posterior and lateral to the duct opening.
FIGURE 64–6 The perineum constitutes part of the vulva. It lies between the posterior commissure and the perianal skin. Deep to the skin are the “perineal body” and the external sphincter ani.
FIGURE 64–7 The perianal skin lies in the immediate vicinity of the anus and is subject to fecal contamination and inflammation if it is not kept clean and relatively dry. The skin in this area is usually more pigmented than the skin peripheral to it.
FIGURE 64–8 A flap has been cut in the skin of the left labium majus. Ninety-five percent of the subdermal content is fat. The glistening white membrane at the bottom of the incision is Colles’ fascia.
FIGURE 64–9 The fascia has been dissected away from the three superficial perineal muscles. These muscles are very thin structures and are represented in the drawing as they are seen during cadaver dissection. Between and covering the muscles is the tough Colles’ fascia. Although others have described another fascial layer below Colles’ fascia, the author has not found this layer to be a separate entity.
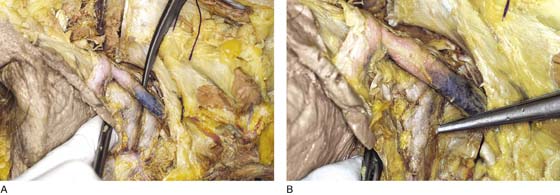
FIGURE 64–10 A. An incision is made immediately lateral to the hymenal ring. The white membrane is Colles’ fascia. The vagina (V) is seen medial to the incision. B. Colles’ fascia has been incised, and the bulbocavernosus muscle is dissected.
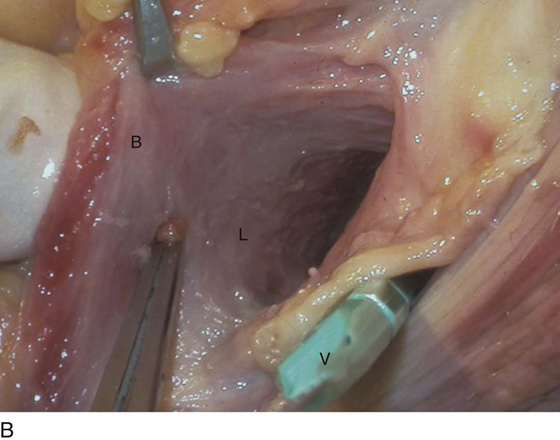
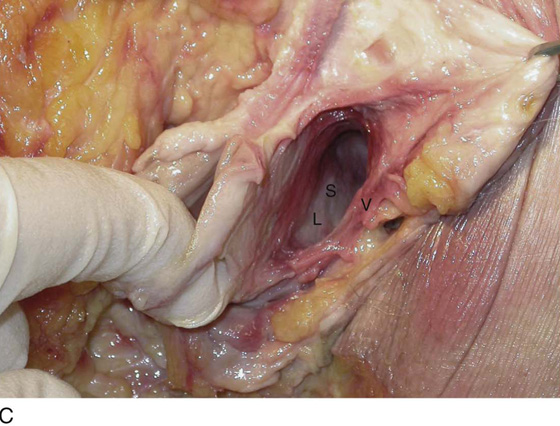
FIGURE 64–11 A. The bulbocavernosus muscle is held on edge with two Allis clamps. B. The green scalpel handle has been placed into the vagina (V). The scissors point to the junction of the bulbocavernosus (B) with the deeper lying levator ani muscle (L). The surgeon’s gloved finger is behind and lateral to the bulbocavernosus muscle. C. The surgeon’s finger is lateral to the right bulbocavernosus muscle. The space (S) dissected along the right inner vaginal wall (V) exposes the levator ani muscle (L).
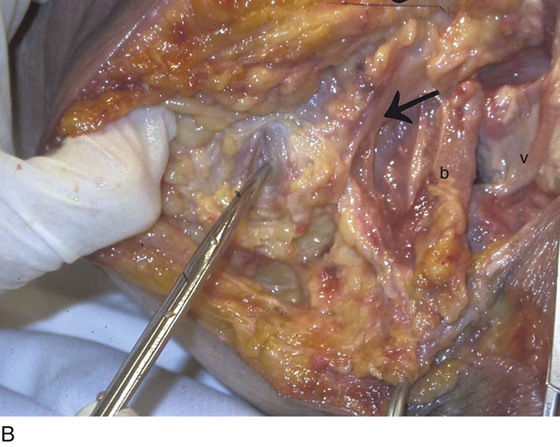
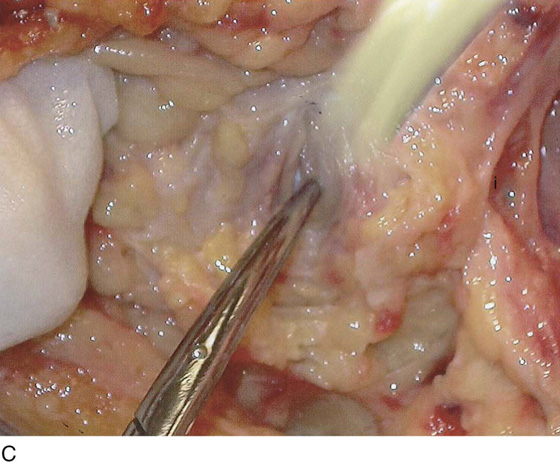
FIGURE 64–12 A. The scissors point to the superficial transverse perineal muscle. The ischiocavernosus muscle (i) lies along the pubic and ischial ramus. The perineal membrane has been removed to expose the underlying levator ani muscle (L). The vagina (V) has been dissected anteriorly, producing the hole in the anterior wall. B. The scissors point to the ischial tuberosity. The arrow points to the ischiocavernosus muscle. The bulbocavernosus (b) muscle is to the right of the vagina (V). C. Same photo as part B, but the ischial ramus has been added. The ischiocavernosus muscle (i) lies along the ramus.
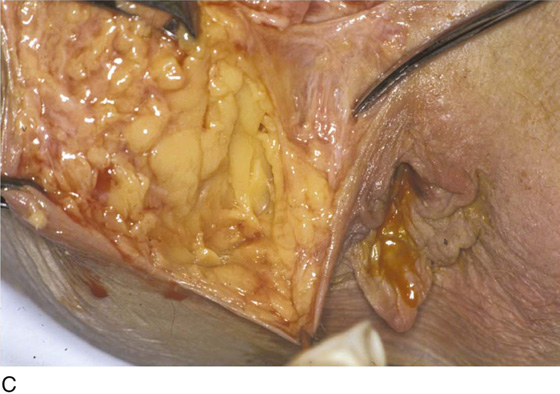
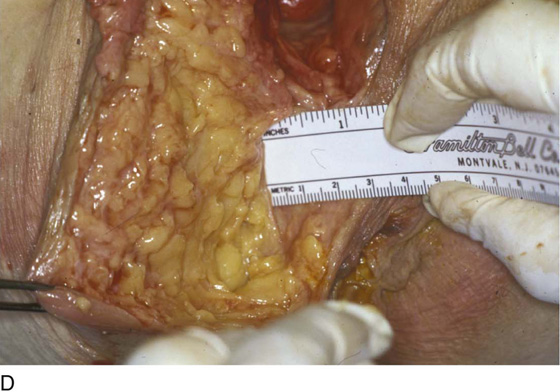
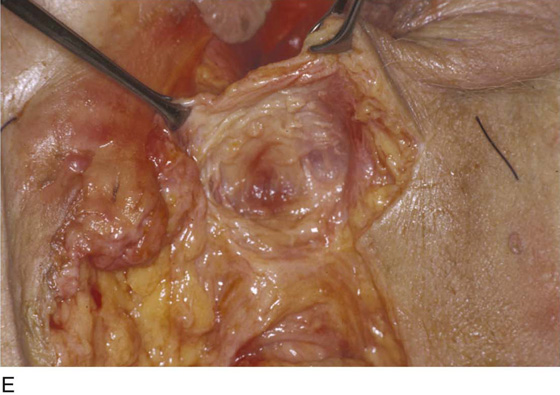
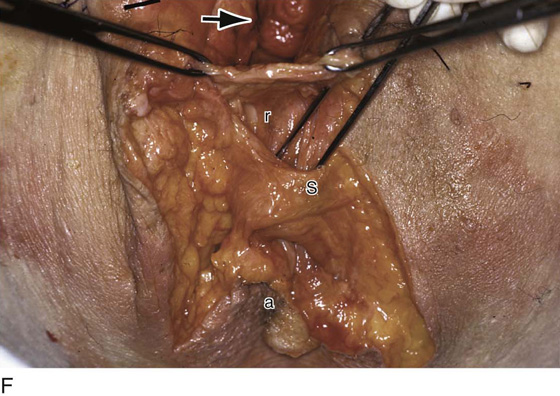
FIGURE 64–13 A. An inverted-U incision has been made in the perineum and perianal skin, exposing the fat in the ischiorectal fossa. B. Magnified view of part A. The anal sphincter lies within the fat peripherally around the anus. It measures approximately 1 inch in width. C. The forceps point to the right lateral margin of the pink external anal sphincter. D. The ruler documents the width of the right portion of the external anal sphincter. E. The posterior vaginal wall, which measures 4 mm thick, has been dissected free from the rectum. F. The arrow points to the vagina. The Allis forceps hold the dissected posterior vaginal wall. The outer wall of the rectum (r) constitutes the inner sphincter mechanism. The external sphincter (S) has been partially separated from the rectum (r). The anal opening (a) is seen at the lower margin of the photo.
FIGURE 64–14 A. The levator ani (L) is seen adjacent to the anal sphincter and the anorectal inner wall (AW). B. A needle has been placed to mark the location of the levator ani muscle. The handle of the needle is seen above the mons in the retropubic space. The needle tip emerges in the dependent portion of the levator ani lateral to the anorectal wall, where it interdigitates with the external sphincter ani. C. Close-up of the right levator ani muscle (L). The upper Allis forceps hold the edge of the posterior vagina (V). The lower Allis forceps hold the edge of the anus (A).
FIGURE 64–15 The scissors are spread beneath the body of the clitoris. The large left corpora of the clitoris lies along the pubic ramus and is more prominent than is the ischiocavernosus muscle (i).
FIGURE 64–16 The tissues situated deep to the superficial perineal muscles and Colles’ fascia constitute a “blood lake” and are composed of a tightly applied tough connective tissue membrane overlying cavernous vascular spaces. These constitute the clitoral crura, the vestibular bulbs, and the body of the clitoris. The bulb of the vestibule shares a common wall with the urethra (anterior and lateral). Situated deep to and exposed between the bulb and the clitoral crus is the fascia covering the levator ani muscle. Between the fascia and the muscle is a thin layer of fat.
FIGURE 64–17 A. A portion of the fascia has been stripped from the left clitoral crus (corpora), revealing the deep blue coloration produced by the engorged cavernous spaces. B. The scissors point to the bulb of the vestibule.
FIGURE 64–18 The tip of the scissors lifts the fascia of the levator ani muscle. If one were to push the scissors upward, the tip of the scissors would be seen to emerge in the retropubic space.
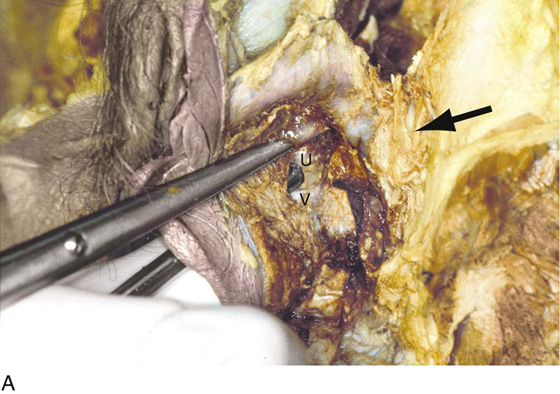
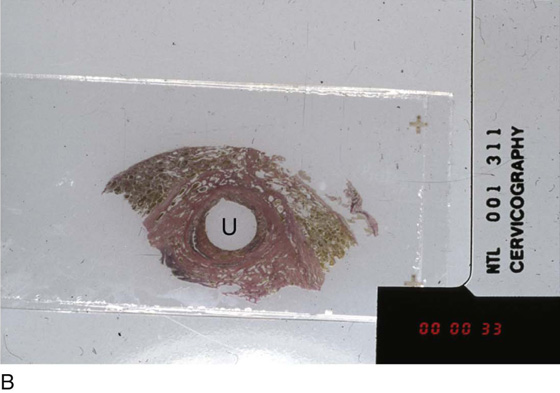
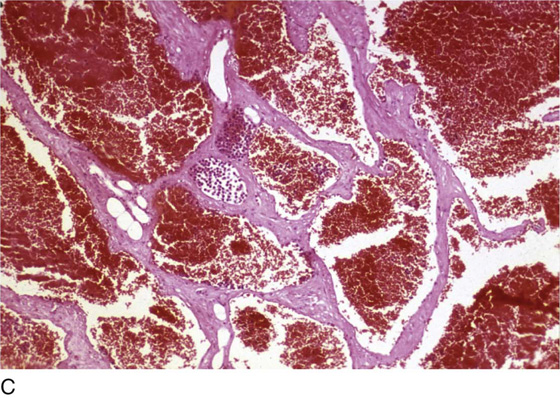
FIGURE 64–19 A. The surgeon’s gloved finger has been inserted into the vagina of the cadaver. The metal tube has been placed into the urethra. The scissors have dissected through the bulb of the vestibule and have opened through the lateral urethral wall (U). A small bit of the white gloved finger (V) can be seen beneath the metal urethral cannula. The arrow points to the left corpora and pubic ramus. B. Microscopic section shows the urethra covered in umbrella-like fashion by the cavernous and blood-filled spaces of the bulb of the vestibule (Verhoeff–van Gieson stain). The urethral lumen is labeled (U). C. High-powered view of part B (hematoxylin and eosin stain).
FIGURE 64–20 The anus passes along the axis of the vagina after initial anterior vectoring. The mass of tissue between the perineum and the anorectal wall is the anterior sphincter ani muscle.
FIGURE 64–21 Anal ultrasound image showing the relationship of the anus to its sphincter and the posterior wall of the vagina.
FIGURE 64–22 This patient has an anovaginal sinus tract. Note the direction of the anal canal. The whitish discharge (arrow) emits from the lower, posterior wall of the vagina.
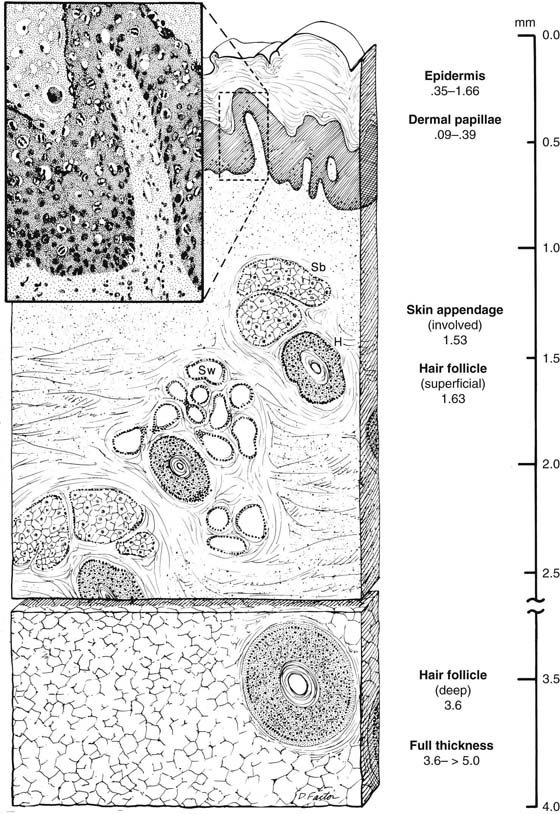
The microanatomy of the vulva is essentially that of specialized skin. The epithelium is composed of stratified and cornified squamous cells. Where the epithelium abuts the underlying stroma, it is characterized by finger-like downward-plunging pegs and upward-extending projections of the dermis known as the dermal papillae. Within the connective tissue stroma lie the sebaceous glands, ordinary sweat glands, and the large modified sweat (scent) glands, that is, the apocrine glands. In close proximity to the sebaceous glands are hair shafts and follicles. The follicles may extend deeply (3 to 4 mm) into the underlying fat. The dermis itself is divided into a small zone of papillary dermis and a larger zone of recticular dermis (Fig. 64–23).
FIGURE 64–23 Schematic microanatomic cross-section of vulvar skin based on micrometer measurements of actual histologic material. The papillary dermis is located directly beneath the epithelial pegs. The reticular dermis extends down to the subcutaneous tissue. H, hair follicle/shaft; Sb, sebaceous glands; Sw, sweat glands.