Chapter 41 Vomiting and Gastroesophageal Reflux
ETIOLOGY
How Do I Categorize Causes of Vomiting?
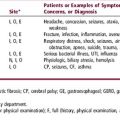
It is useful to classify causes of vomiting depending on the age of children. Table 41-1 lists some common and uncommon causes of vomiting in three different age groups. Remember that regurgitation or spitting up is common in infants and indicates physiologic gastroesophageal reflux, not true vomiting. Viral gastroenteritis and gastroesophageal reflux are common causes at all ages, although they tend to occur predominantly in infants and younger children. Infections outside the gastrointestinal tract (extraintestinal infections), such as otitis media, pneumonia, and urinary tract infection, are more likely to cause vomiting in younger children than in adolescents. Persistent vomiting in neonates or infants should raise suspicion about anatomic obstructions in the gastrointestinal tract such as intestinal atresia, malrotation, or pyloric stenosis. Peptic disorders such as Helicobacter gastritis or duodenal ulcer are seen most often in adolescents. Raised intracranial pressure is an important condition that can cause vomiting at any age. The likely causes of raised intracranial pressure are meningitis and hydrocephalus in infants and brain tumors in older children. Motion sickness can cause vomiting in children and adolescents. Cyclic vomiting syndrome is an uncommon disorder characterized by recurrent episodes of vomiting separated by symptom-free intervals, without any obvious organic cause.
| Infant (< 1 yr) | Child (1–12 yrs) | Adolescent (> 12 yrs) |
|---|---|---|
| Common | ||
| Gastroesophageal reflux | Gastroesophageal reflux | Gastroesophageal reflux |
| Gastroenteritis | Gastroenteritis | Peptic disorders |
| Viral (rotavirus) | Viral (rotavirus) | Duodenal ulcer |
| Bacterial | Bacterial | Gastritis (Helicobacter) |
| Anatomic obstruction | Extraintestinal infections | Gastroenteritis |
| Pyloric stenosis | Otitis media | Toxic/medications |
| Intestinal atresia | Urinary tract infection | Extraintestinal infections |
| Intussusception | Sinusitis | Sinusitis |
| Malrotation | Pneumonia | Pyelonephritis |
| Extraintestinal infections | ||
| Otitis media | ||
| Urinary infection | ||
| Pneumonia | ||
| Uncommon | ||
| ↑Intracranial pressure | Anatomic obstruction | ↑Intracranial pressure |
| Meningitis | Malrotation | Meningitis |
| Hydrocephalus | ↑Intracranial pressure | Brain tumor |
| Inborn errors of metabolism | Meningitis | Pancreatitis |
| Milk protein intolerance | Brain tumor | Appendicitis |
| Pancreatitis | Cancer chemotherapy | |
| Appendicitis | Cyclic vomiting syndrome | |
| Cancer chemotherapy | Pregnancy | |
| Cyclic vomiting syndrome | Migraine | |
| Motion sickness | Motion sickness | |
| Psychogenic | ||
EVALUATION
How Does the Nature of Vomiting Help with Diagnosis?
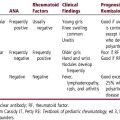
Details about the nature of vomiting can provide important diagnostic clues that help you focus your history and examination. Start with an open-ended question, such as “Tell me more about the vomiting.” Then, ask specific questions to identify duration, temporal pattern, relation with meals, color, and intensity of vomiting. Table 41-2 provides some diagnostic clues for the nature of vomiting. It is important to remember that bilious vomiting indicates intestinal obstruction unless proven otherwise.
| Clue | Causes |
|---|---|
| Duration | |
| Acute | Gastrointestinal infection, extraintestinal infection |
| Acute, progressive | Anatomic obstruction, intraabdominal pathology |
| Chronic, mild | Gastroesophageal reflux, peptic disorders |
| Cyclic, intermittent | Migraine, cyclic vomiting syndrome |
| Temporal Association | |
| Postprandial | Gastroesophageal reflux, peptic disorders |
| Early morning | Raised intracranial pressure, pregnancy |
| Color | |
| Bloody | Active bleeding in upper gastrointestinal tract (e.g., esophagitis, duodenal ulcer, Mallory-Weiss tear) |
| Coffee ground | Recent-onset bleeding in upper gastrointestinal tract |
| Bilious | Intestinal obstruction (beyond pancreatic ampulla) |
| Intensity | |
| Effortless regurgitation | Gastroesophageal reflux (common in infancy) |
| Projectile | Obstruction in upper gastrointestinal tract (e.g., pyloric stenosis) |