Vogt–Koyanagi–Harada Disease
Clinical Features:
Initially, VKH was classified as two separate diseases:
▶ Vogt–Koyanagi syndrome: comprising chronic anterior uveitis, alopecia, poliosis, vitiligo, and dysacousia.
▶ Harada’s disease: comprising bilateral posterior, exudative uveitis, and neurological features.
Considering the considerable overlap in the features, the term VKH disease is now used.
At onset, patients may experience flu-like symptoms, central nervous system signs, optic neuropathy, sensitivity of hair and skin to touch, perilimbal vitiligo, alopecia, vitiligo poliosis and auditory signs. Blurred vision, photophobia, conjunctival hyperemia, and ocular pain also occur. Bilateral anterior and exudative posterior uveitis is typical. Shallow, serous retinal detachments are seen at the posterior pole with underlying choroidal infiltrates (Fig. 17.4.1). The optic disc is edematous and hyperemic.

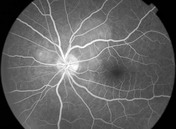
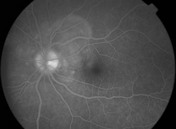
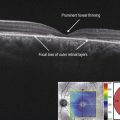
Figure 17.4.1 Color fundus photograph of a patient with Vogt–Koyanagi–Harada shows the classic exudative posterior pole detachment (arrows). Intermediate stage fluorescein angiography shows multiple hyperfluorescent spots at the choroidal level and some diffuse pooling of dye in the subretinal space. Late stage fluorescein angiography shows disc hyperemia and staining with pooling of dye in the serous retinal detachment.
OCT Features:
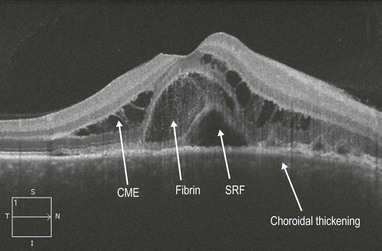
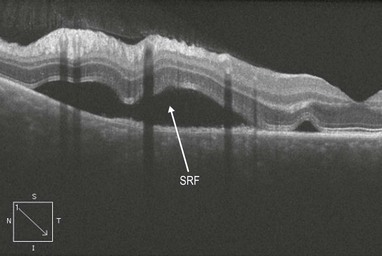
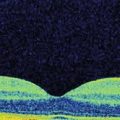
OCT reveals serous retinal detachments at the macula. The subretinal fluid may reveal a higher optical density than the vitreous, suggesting a higher level of protein content (Figs 17.4.2 and 17.4.3). Inner retinal layers are typically well preserved with cystic changes and complex infolding in the outer retinal layers. Subretinal fibrinoid deposits are seen, which may later evolve into subretinal fibrosis. Vitreoretinal interface alterations with cellular deposits may also be seen. There may be alteration and thickening of the IS–OS junction/ellipsoid layer, RPE and choroidal folds, and thickening of the choroid. Enhanced depth imaging OCT will show significant choroidal thickening, which resolves when treated.
Ancillary Testing:
▶ Ultrasonography: Ultrasound is helpful if the posterior segment is not visible, and reveals diffusely thickened posterior choroid with low to medium reflectivity, serous retinal detachments, vitritis, and thickened sclera or episclera.
▶ Cerebrospinal fluid analysis: cerebrospinal fluid pleocytosis and elevated protein levels are seen.