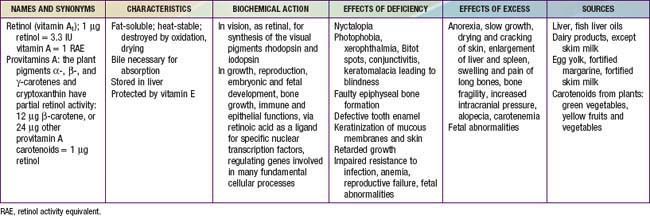
Chapter 45 Vitamin A Deficiencies and Excess
Overview of Vitamins
Vitamins are essential organic compounds that are required in very small amounts (micronutrients) and are involved in fundamental functions in the body, such as growth, maintenance of health, and metabolism. A vitamin can have several functions. Because our bodies cannot biosynthesize vitamins, vitamins must be supplied by the diet or as supplements. The dietary reference intakes (DRIs) for infants and children are summarized in Table 41-5. Vitamins are not chemically similar. Based on their chemical properties, they are classified as either water-soluble or fat-soluble; these 2 groups are handled differently by the body. The water-soluble vitamins (except vitamin C) are members of the B complex.
Deficiency states in developed countries are rare, except in some impoverished populations (Chapter 43) or after mistakes in food preparation or with fad diets, but they are common in many developing countries and are often associated with global malnutrition (Chapter 43). In the clinical setting, vitamin deficiencies can also occur as complications in children with various chronic disorders or diseases. Information obtained in the medical history related to dietary habits can be important in identifying the possibility of such nutritional problems. Except for vitamin A, toxicity from excess intake of vitamins is rare. The food sources, functions, and deficiency and excess symptoms of the vitamins are summarized in Tables 45-1 and 48-1.
Vitamin A
Absorption, Transport, Metabolism, Storage
The body acquires vitamin A either as preformed vitamin A (usually as esters) or as provitamin-A carotenoids. In the USA, grains and vegetables supply approximately 55% and dairy and meat products supply approximately 30% of vitamin A intake from food. Vitamin A and the provitamins-A are fat-soluble, and their absorption depends on the presence of adequate lipid and protein within the meal. Chronic intestinal disorders or lipid malabsorption syndromes can result in vitamin A deficiency. Ingested and absorbed provitamins-A are bioconverted to vitamin A molecules in the small intestine by the carotene cleavage enzyme dioxygenase; β-carotene provides twice the vitamin A activity of the other provitamins-A. Further processing in the enterocyte involves the esterification of vitamin A to retinyl palmitate for incorporation into chylomicrons, which are released into lymph and transported via the circulation to the liver for storage or to other tissues. The vitamin A content in the liver is low at birth, but it increases 60-fold during the first 6 mo of life. If the growing child has a well-balanced diet and obtains vitamin A from foods that are rich in vitamin A or provitamin-A (see Table 45-1), the risk of vitamin A deficiency is small. However, even subclinical vitamin A deficiency can have serious consequences.
Function and Mechanism of Action
Retinoic acid is among the most important signaling molecules in vertebrate ontogenesis. It affects many physiologic processes, including reproduction, growth, embryonic and fetal development, and bone development, in addition to respiratory, gastrointestinal, hematopoietic, and immune functions. The role of vitamin A in immune function and host defense is particularly important in developing countries, where vitamin A supplementation or therapy reduces the morbidity and mortality rates of various diseases, such as measles (Chapter 238).
Vitamin A Deficiency
Clinical Manifestations
The cornea protects the eye from the environment and is also important in light refraction. In early vitamin A deficiency, the cornea keratinizes, becomes opaque, is susceptible to infection, and forms dry, scaly layers of cells (xerophthalmia). In later stages, infection occurs, lymphocytes infiltrate, and the cornea becomes wrinkled; it degenerates irreversibly (keratomalacia), resulting in blindness. The conjunctiva keratinizes and develops plaques (Bitot spots [Fig. 45-1]). The pigment epithelium is the structural element of the retina and keratinizes. When the pigment epithelium degenerates, the rods and cones have no support and eventually break down, resulting in blindness. Advanced xerophthalmia is shown in Figure 45-2, and xerophthalmia with permanent damage to the eye is shown in Figure 45-3. These eye lesions are primarily diseases of the young and are a major cause of blindness in developing countries.

Figure 45-1 Bitot spots with hyperpigmentation seen in a 10 mo old Indonesian boy.
(From Oomen HAPC: Vitamin A deficiency, xerophthalmia and blindness, Nutr Rev 6:161–166, 1974.)
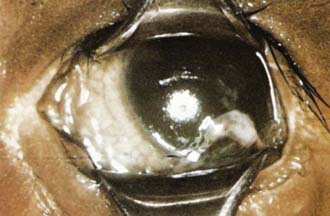
Figure 45-2 Advanced xerophthalmia with an opaque, dull cornea and some damage to the iris in a 1 yr old boy.
(From Oomen HAPC: Vitamin A deficiency, xerophthalmia and blindness, Nutr Rev 6:161–166, 1974.)
Prevention
The daily recommended dietary allowance (RDA) is expressed as retinol activity equivalents (RAEs; 1 RAE = 1 µg all-trans-retinol; equivalents for provitamin-A in foods = 12 µg β-carotene, 24 µg α-carotene, or 24 µg β-cryptoxanthin). The RAE for infants 0-1 yr of age is 400-500 µg; for children 3 yr of age is 300 µg; for children 4-8 yr of age is 400 µg; for children 9-13 yr of age is 600 µg; for boys 14-18 yr of age and men is 900 µg; and for girls 14-18 of age and women is 700 µg (also see Table 41-8). During pregnancy, the RDA is 750-770 µg, and during lactation, the RDA is increased to 1,200-1,300 µg to ensure sufficient vitamin A content during breast-feeding. A daily tolerable upper level of vitamin A for adults is 3,000 µg of preformed vitamin A. Approximately 80% of dietary vitamin A is absorbed as long as the meal contains some fat (>10 g). Low-fat diets may need to be supplemented with vitamin A. In disorders with poor fat absorption or increased excretion of vitamin A, water-miscible preparations should be administered in amounts higher than the RDAs. Premature infants have poor lipid absorption and thus should receive water-miscible vitamin A and be monitored closely.
Hypervitaminosis A
Chronic hypervitaminosis A results from excessive ingestion of vitamin A for several weeks or months. Toxicity can be induced in adults and children with chronic daily intakes of 15,000 µg and 6,000 µg, respectively. Symptoms subside rapidly on withdrawal of the vitamin. Signs of subacute or chronic toxicity can include headache; vomiting; anorexia; dry, itchy desquamating skin; seborrheic cutaneous lesions; fissuring at the corners of the mouth; alopecia and/or coarsening of the hair; bone abnormalities; swelling of the bones; enlargement of the liver and spleen; diplopia; increased intracranial pressure; irritability; stupor; limited motion; and dryness of the mucous membranes. In addition, desquamation of the palms and the soles of the feet is common. Radiographs show hyperostosis affecting several long bones, especially in the middle of the shafts (Fig. 45-4). Serum levels of vitamin A are elevated. Hypercalcemia and/or liver cirrhosis may be present. Hypervitaminosis A is distinct from cortical hyperostosis (Chapter 691).
Benn CS, Martins C, Rodrigues A, et al. Randomized study of effect of different doses of vitamin A on childhood morbidity and mortality. BMJ. 2005;331:1428-1430.
Blomhoff R, Blomhoff HK. Overview of retinoid metabolism and function. J Neurobiol. 2006;66:606-630.
Erhardt J. Biochemical methods for the measurement of vitamin A deficiency disorders (VADD). Sight Life. 2003;2:5-7.
Labadarios D, Randal P. Presentation highlights: vitamin A and the common agenda for micronutrients. XXII IVACG meeting, 15–17 November 2004, Lima, Peru. Sight Life. 2005;1:9-17.
Sommer A. Vitamin A deficiency and clinical disease: an historical overview. J Nutr. 2008;138:1835-1839.
Stipanuk MH, editor. Biochemical, physiological, and molecular aspects of human nutrition, ed 2, Philadelphia: Saunders, 2006.
Tielsch JM. Vitamin A supplements in newborns and child survival. BMJ. 2008;336:1385-1386.
Tielsch JM, Klemm R, West KPJr, et al. Newborn vitamin A dosing and early infant survival: current evidence and controversy. Sight Life. 2008;2:22-26.