Viral infections – Warts and other viral infections
Unlike bacteria and yeasts, viruses are not thought to exist on the skin surface as commensals. However, studies in patients with viral warts have shown viral DNA in epidermal cells of seemingly normal skin next to warty areas.
Viral warts
Aetiopathogenesis and pathology
Over 96 subtypes of DNA HPV have been identified. The virus infects by direct inoculation and is caught by touch, sexual contact or at the swimming baths. Certain HPV subtypes are associated with specific clinical lesions, e.g. types 2, 27 and 57 with common hand warts, types 1, 2, 4, 27 and 57 with plantar warts, types 3 and 10 with plane warts, types 6 and 11 with genital warts. Genital HPV subtypes cause cytological dysplasia of the cervix, which may be precancerous. Immunosuppressed individuals, such as those with organ transplants, are particularly susceptible to viral warts (p. 57). The epidermis is thickened and hyperkeratotic. Keratinocytes in the granular layer are vacuolated due to being infected with the wart virus.
Clinical presentation
Certain clinical patterns are well recognized:
 Common warts. These present as dome-shaped papules or nodules with a papilliferous surface. They are usually multiple, and are commonest on the hands (Fig. 1) or feet in children but also affect the face and genitalia. Their surface interrupts skin lines. Some facial warts are ‘filiform’ with fine digit-like projections.
Common warts. These present as dome-shaped papules or nodules with a papilliferous surface. They are usually multiple, and are commonest on the hands (Fig. 1) or feet in children but also affect the face and genitalia. Their surface interrupts skin lines. Some facial warts are ‘filiform’ with fine digit-like projections.
 Plane warts. These are smooth flat-topped papules, often slightly brown in colour, and commonest on the face (Fig. 2) and dorsal aspects of the hands. They are usually multiple and resist treatment, but eventually resolve spontaneously, often after becoming inflamed. They can show the Koebner phenomenon.
Plane warts. These are smooth flat-topped papules, often slightly brown in colour, and commonest on the face (Fig. 2) and dorsal aspects of the hands. They are usually multiple and resist treatment, but eventually resolve spontaneously, often after becoming inflamed. They can show the Koebner phenomenon.
 Plantar warts. These are seen in children and adolescents on the soles of the feet; pressure causes them to grow into the dermis. They are painful and covered by callus, which, when pared, reveals dark punctate spots (thrombosed capillaries). Mosaic warts are plaques on the soles that comprise multiple individual warts.
Plantar warts. These are seen in children and adolescents on the soles of the feet; pressure causes them to grow into the dermis. They are painful and covered by callus, which, when pared, reveals dark punctate spots (thrombosed capillaries). Mosaic warts are plaques on the soles that comprise multiple individual warts.
 Genital warts. In males, these affect the penis and, in homosexuals, the perianal area. In females, the vulva, vagina and perianal area maybe involved (Fig. 3). The warts may be small or may coalesce into large cauliflower-like ‘condylomata acuminata’. Proctoscopy (if perianal warts are present) and colposcopy (for female genital warts) are needed to identify and treat any rectal or cervical warts because of the risk of neoplastic change. Sexual partners need to be examined.
Genital warts. In males, these affect the penis and, in homosexuals, the perianal area. In females, the vulva, vagina and perianal area maybe involved (Fig. 3). The warts may be small or may coalesce into large cauliflower-like ‘condylomata acuminata’. Proctoscopy (if perianal warts are present) and colposcopy (for female genital warts) are needed to identify and treat any rectal or cervical warts because of the risk of neoplastic change. Sexual partners need to be examined.
Differential diagnosis and complications
The diagnosis of viral warts is usually obvious. Occasionally, corns on the sole or hand, or molluscum contagiosum elsewhere, are confused. With viral warts under the fingernails and toenails, it is important to consider amelanotic malignant melanoma, periungual fibroma (of tuberous sclerosis, p. 92) and bony subungual exostosis. Genital warts may resemble the condyloma lata of secondary syphilis. HPV types 16 and 18 in genital warts carry a risk of malignant change. HPV infections in organ transplant patients have been linked with skin cancers.
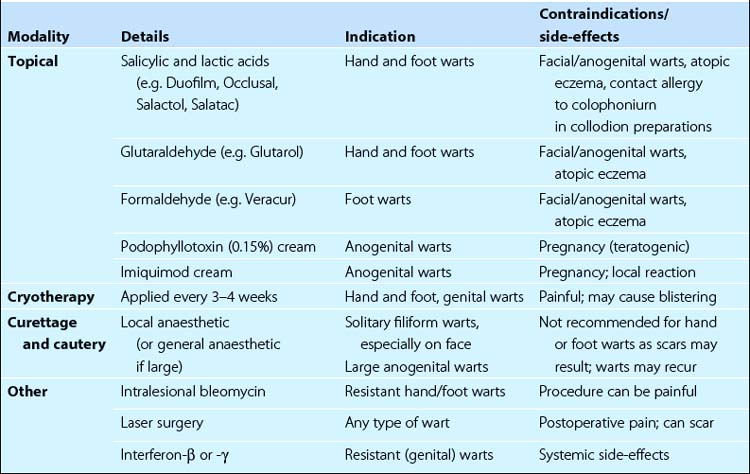
Management
In children, 30–50% of plantar warts disappear spontaneously within 6 months. Hand and foot warts should be pared by a scalpel or using an emery board. This gets rid of keratotic skin and allows easier treatment. Table 1 shows the available treatments. Immunosuppressed patients, especially those with organ transplants, are prone to wart infections. They need special management and should be inspected and treated for warts before being given their grafts.
Other viral infections
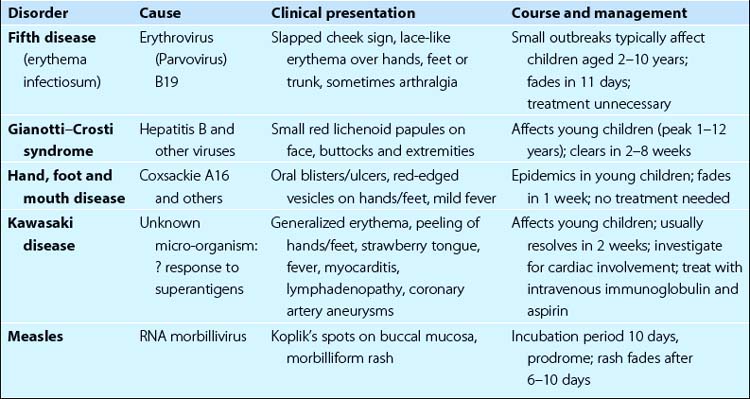
Other viral infections include molluscum contagiosum, orf, HIV (p. 56) and those in Table 2.
Molluscum contagiosum
Molluscum contagiosum are discrete pearly-pink umbilicated papules that are caused by a DNA pox virus. Mollusca mainly affect children or young adults. Spread is by contact, including sexual transmission or on towels. The dome-shaped papule, a few millimetres in diameter, has a punctum and, if squeezed, releases a cheesy material. The lesions are usually multiple and grouped, sometimes with a localized eczema. They are commonest on the face, neck and trunk (Fig. 4). Isolated ones may go unrecognized. Untreated, they may persist for several months.
Orf
A solitary red papule appears, usually on a finger, after an incubation period of about 6 days (Fig. 5). It grows rapidly to 1 cm or so in size, evolving into a painful purple pustule, which often has a necrotic umbilicated centre. Erythema multiforme (p. 82) and lymphangitis are complications. Spontaneous resolution takes 2–4 weeks. Secondary infection requires a topical or systemic antibiotic.