CHAPTER 7 Videofluoroscopy
Introduction
Videofluoroscopy of swallow (VFS) is defined by the Royal College of Speech and Language Therapists (RCSLT) (2006) as a modification of the standard barium swallow examination used in the assessment and management of oropharyngeal swallowing disorders. This instrumental swallowing evaluation is often described as the ‘gold standard’ for the assessment of dysphagia (Daniels et al., 1997; Robbins et al., 1999). Dysphagia is defined as a disorder of swallowing food (solid and/or liquid) from the mouth to the stomach (Logemann, 1998). Swallowing disorders can occur at every age and have various etiologies. Swallowing dysfunction can be caused by head and neck pathologies (e.g. inflammations and tumors of the oral cavity, oropharynx and larynx), neurological diseases and injuries (e.g. strokes, multiple sclerosis, motor neurone disease (MND), Parkinson’s disease, tumors and head injury) or other illnesses (e.g. psychological/functional, or as a side effect of medication). As stated by the RCSLT in their Policy Statement (2006), VFS can be used for assessment, treatment and management of swallowing where the suspected condition or disease process impacts upon swallow function and may result in a risk of death, pneumonia, dehydration, malnutrition and psychosocial issues related to discomfort and difficulty in eating and drinking.
Videofluoroscopy has the additional benefit of providing an objective baseline to which future examinations can be compared as a measure of improvement and enabling management strategies to be formulated. Martino et al. (2000) reinforced the importance of videofluoroscopy by stating that the validity of most other assessments and screening tools is often measured against videofluoroscopy and none comes close to VFS in terms of sensitivity and specificity. This chapter will provide the basis to enable a greater understanding of the videofluoroscopic procedure and the predisposing factors necessary to create a successful fluoroscopy team.
Purpose and benefits
Being both a time consuming and costly examination, it is vital that the actual VFS procedure runs as smoothly as possible. Communicating the plans of the procedure to all staff involved and prior explanation to the patient/carer will ensure minimal time delay. This should in turn prevent the patient and staff feeling rushed and anxious, both of which may result in a suboptimal examination. Patients must be fully informed about the VFS procedure prior to the examination. Consideration should be given to providing information in accessible spoken, written and/or visual formats, including the nature, purpose and likely effects of the examination (RSCLT 2006). Logemann (1998) categorically states that:
Also known as a modified barium swallow, a VFS is simply that – an adjustment to the traditional barium swallow. One modification is that low density contrast is utilized which highlights flow through the oropharynx much better than high density used in traditional barium swallows (where increased coating of the mucosal wall is desired). Further modifications are associated with the volumes and consistencies of the contrast agents provided, together with the speed at which they are given, attempting to replicate the consistencies of everyday food and fluid. This then demonstrates any dysfunction of oropharyngeal deglutition, enabling treatment and therapy aims to be devised. The primary aims of the VFS as described by the RCSLT (2006) are seen in Box 7.1.
BOX 7.1 Purpose of videofluoroscopy as defined by RCSLT (2006)
 Evaluation of swallowing physiology, including lip and tongue function, velopharyngeal closure, base of tongue retraction, hyolaryngeal elevation, pharyngeal contraction, upper esophageal sphincter function and airway protection mechanisms
Evaluation of swallowing physiology, including lip and tongue function, velopharyngeal closure, base of tongue retraction, hyolaryngeal elevation, pharyngeal contraction, upper esophageal sphincter function and airway protection mechanismsAs is stated by RCSLT (2006): ‘Patients must undergo an appropriate clinical assessment of swallowing by a Speech and Language Therapist (SLT) prior to VFS being undertaken’. The widely accepted standard procedure is for all patients to undergo a clinical swallowing evaluation (CSE) prior to completion of VFS. This will serve to fulfil many purposes, inclusive of enabling the aims of VFS to be established; assessment of candidate suitability for VFS; full explanation of the procedure (inclusive of aims of outcome); and obtaining of consent.
In addition, RCSLT (2006) state that an SLT-led CSE prior to VFS will also ‘assist in determining the nature and severity of the swallowing disorder and other factors contributing to the conduct of the VFS, such as cognition, presence of the carer, feeding arrangements, positioning and anxiety etc.’ It will also aid communication within the VFS to alert the radiographer and other multidisciplinary team (MDT) members what the plans for the procedure are and how they are to be completed. Communication with the patient during the VFS is imperative so that they are aware of every step of the procedure. The pre-VFS CSE should have prepared them with instructions, but anxiety and confusion can compound any complications and, if not treated accordingly, can waste the examination completely by altering the results from those aimed to be achieved, e.g. positional modification. The patient should be instructed clearly and concisely, by demonstration if necessary. If they do not complete the desired instruction they may aspirate contrast to such an extent that the examination has to be abandoned. Potential dangers of aspiration such as choking and pneumonia are also factors which correct communication should avoid.
It must be noted that patients rarely present with an isolated dysphagia. As previously mentioned, dysphagia usually arises as a result of a wide range of pathologies, which often have other associated motor, sensory and emotional/psychological problems. These must all be taken into account when planning and arranging a VFS. A patient who is bedbound and unable to support themselves in an upright position may not be a suitable candidate for a VFS due to poor strength and/or restricted movement, but accommodating alterations to the procedure are possible. This includes specialist seating equipment, physical supports or simple altered position of the x-ray table. It must be noted that within a VFS the ideal initial position for examination is a lateral view but, for a bedbound patient who is only able to manage supine positioning, anterior-posterior (AP) viewing may be the only possibility. Within a fluoroscopy suite equipped with a C-arm, manipulation of the x-ray tube to the side of the patient will enable lateral viewing but, in the traditional screening room, this is not possible and viewing is limited to AP positioning. While this has benefits for assessment of laterality of deficit, full assessment of laryngeal penetration and aspiration is not as clear as in the lateral position.
While the VFS is, as previously mentioned, the ‘gold standard’ within swallowing assessment, these motor, sensory and emotional/psychological constraints often limit the procedure and, in some cases, inhibit the examination. Langmore et al. (1991) summarize those groups of patients where VFS cannot be utilized:
Contrast agents
The benefits of barium sulfate are reported to be that it is non-toxic, relatively cheap and inert. Farrow and Stevenson (1997) state that barium is an excellent contrast agent for the GI tract provided that is where it stays. Barium aspirated into the lungs is usually harmless and can be expectorated either spontaneously or aided by a physiotherapist. However, barium is thought to cause inflammation and infection if aspirated into the lungs where expectoration is poor or suction is not available and should therefore be avoided if there is a significant risk of this occurring. However, there is extremely minimal evidence to support this, resulting in many institutions continuing to utilize barium as the contrast of choice. In cases where aspiration is suspected and the reason for it is the primary purpose of the investigation, administering small volumes initially would therefore be reasonable to limit the amount of contrast entering the airway.
Within a national health service VFS clinic, barium sulfate is the contrast agent of choice due to its reasonable cost and non-toxicity. It also mixes well with other food agents to alter its viscosity to enable holistic assessment of the oropharyngeal swallow with different consistencies. Meijing et al. (1992) argue that contrast viscosity is directly related to its density and can affect bolus transition at the oropharyngeal stage. However, during most VFS investigations, capability to manage altered consistencies is one of the key factors under investigation and, although lower density barium is preferred in case of aspiration, no modifications to the preparation (other than changes to viscosity) are seen to be necessary if high density barium is used.
Management strategies
Observation of swallowing function during a VFS may identify an inappropriate swallow, for example where the patient aspirates small quantities of fluid, or has residual pooling of contrast agent following the swallow. In these cases, it may be appropriate for the speech therapist or radiographer to trial under fluoroscopy control a number of modifications to the patient’s swallow. Table 7.1 outlines the potential modifications and therapy techniques available to the therapist during the VFS and the reasons for their use. If successful, these modifications can then be explained to patients and carers so that they can be employed when eating and drinking, thus enabling oral intake to commence safely. It is imperative that the patient/carer follows the modification advice given at all times to prevent later difficulties and potential aspiration occurring.
Table 7.1 The role of positional modifications to the VFS procedure
| Positional modification | Disorder and presentation |
|---|---|
CVA, cerebrovascular accident
Multidisciplinary working in VFS
As has previously been outlined, there is a need for close communication between all members of the VFS team. This can include radiologists, radiographers, speech and language therapists and radiology nurses and assistant practitioners. Standardization of the procedure is important (allowing modifications where necessary), particularly as patients may be examined more than once to check response to treatment following a baseline assessment. Even where the examination was conducted by different staff members, consistency of approach is essential. This consistency is achieved by working within an agreed protocol, which is a detailed framework in which a patient is managed (College of Radiographers, 1999). Owen et al. (2004) state that, in the context of imaging and therapy, the primary purpose of the protocol is to provide clear indication of how certain categories of patients will be managed and by whom.
When considering VFS, Power et al. (2006) exemplify through research the lack of clarity and blurring of roles that can exist between SLTs, radiographers and radiologists. Distinct role definition via the formation of a protocol ensures that the professional roles are outlined and minimizes risk to the patient(s) and staff involved. An evidence-based protocol also displays good clinical practice and offers a degree of medico-legal protection for staff undertaking delegated roles (Nightingale, 2008). Within protocol development, all professionals involved in the VFS procedure should contribute to enable precise documentation of the details of the procedure and the respective individuals’ responsibilities.
Skills for Health (2005) published excellent working competences and core skills to enable professionals involved in VFS to offer the highest quality to patients, by demonstrating what is required of the VFS team. The implications of this workforce competence are that the team involved in examination must be just that – a team. It is impossible to complete a VFS without a strong team involvement and knowledge of other’s working. The SLT and the radiographer must collaborate with each other to enable the patient to receive the highest quality of examination, from organization of the clinic to completion of the procedure with final reporting. An area which demonstrates the need for understanding of each other’s role within the Skills for Health competencies, is listed within the section entitled ‘Clinical Knowledge and Technical Knowledge’. Historically, the SLT involved within VFS would have the clinical knowledge and the radiographer would have the technical knowledge. While it is accepted that within VFS the SLT will always have an increased clinical knowledge of the ‘anatomy and physiology of related structures of the areas being examined’, and the radiographer will have the increased ‘working knowledge of production, interactions and properties of x-rays’, there are definite areas of cross-over which are now accepted as being important to the safe and efficient running of such an MDT clinic. These include the SLT having ‘a working knowledge of harmful effects of radiation to the human body’ and the radiographer having a ‘working knowledge of signs and symptoms of aspiration’ (direct quotations from Skills for Health, 2005). When forming a local protocol and developing guidelines for clinical expertise required of the clinicians within the VFS, the working competence document offered by Skills for Health (2005) is a highly useful tool for reference. Despite its name of a working competence, it should also be considered as national standards, as without these credentials the VFS clinic would not benefit the patient.
Image interpretation
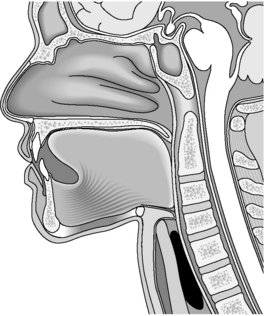
The normal anatomy and physiology of the swallowing mechanism is best demonstrated through simple illustration of the structures involved (Figure 7.1, see color insert).
Logemann (1998) distinguishes four phases of deglutition: the oral preparatory phase; the oral phase; the pharyngeal phase and the esophageal phase.
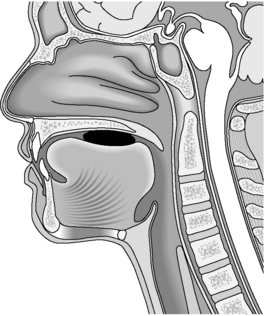
The oral preparatory phase consists of food entering the mouth, masticated if necessary, being mixed with saliva and formed into a bolus. It is at this stage that the individual distinguishes taste, temperature and volume of food. This stage is completely voluntary and movements involved include those of the lips, tongue, mandible and cheeks. The airway remains open and the soft palate lowered at this stage and the individual is able to breathe through the nose (Figure 7.2).
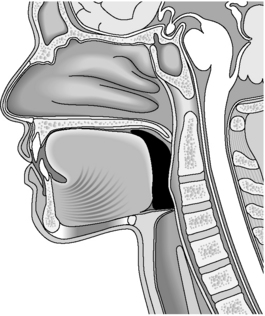
The oral phase (also voluntary) consists of lip closure and increased pressure of the buccal musculature (cheeks), plus anterior–posterior ‘wave-like’ motion of the tongue against the hard palate forcing the prepared bolus to be propelled to the base of the tongue. Nasal breathing remains possible throughout this stage as the soft palate has not yet been raised and the airway is still open (Figure 7.3).
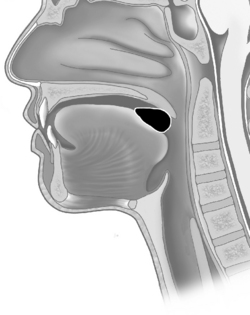
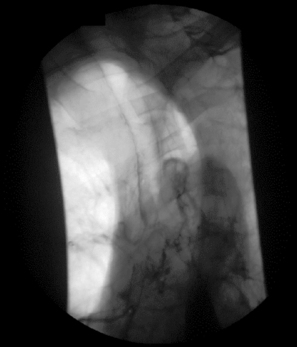
The pharyngeal phase is the first stage of the ‘voluntary to involuntary’ swallowing mechanism. The soft palate is raised and articulates with the posterior pharyngeal wall to ensure none of the bolus enters the nasopharynx. The base of the tongue raises and forms a seal with the posterior pharyngeal wall, while the pharyngeal constrictor muscles contract at the same time to meet the base of tongue. This propels the bolus through positive pressure inferiorly as the swallow is triggered. As an involuntary reflexive response, the hyoid bone is drawn in a superior–anterior triangular motion which, in turn, elevates the larynx to form a seal with the lowered epiglottis. The vocal cords adduct to form an additional airway seal to prevent the passage of food. The cricopharyngeus, situated posterior in relation to the larynx at the proximal esophagus within the pharynx, also relaxes facilitating bolus entry into the esophagus (Figure 7.4).
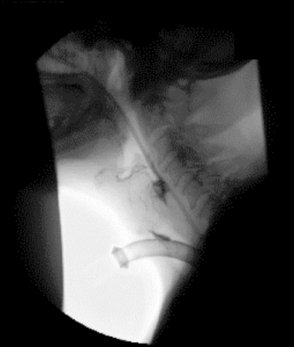
It is during this stage that many disorders are commonly observed. These may be due to neurological dysfunction (motor and/or sensory) causing barium pooling or residue with subsequent overspill into the laryngeal inlet with secondary aspiration (Figure 7.5); structural abnormality, e.g. pharyngeal pouch (Figure 7.6); or the presence of a foreign body such as a tracheostomy tube which can ‘anchor’ the larynx in place and reduce elevation necessary to create complete airway protection (Figure 7.7).
The esophageal phase of the swallow is completely involuntary. Once the cricopharyngeus has constricted behind the bolus, the esophageal peristaltic wave commences which transports the bolus to the lower esophageal sphincter into the stomach (Figure 7.8).
The esophageal phase of swallowing can give rise to many disorders, but those presenting most like a true ‘aspiration-based’ disorder may arise from a tracheo-esophageal fistula, where fluids, foodstuffs (and during videofluoroscopy an x-ray contrast) enter the airway through a small ‘puncture’ between the esophageal and tracheal walls (Figure 7.9). They may in childhood be caused by congenital abnormality but, in adulthood, they are usually as a result of radiation burns, spread of tumor or the sequela of surgical procedures, e.g. laryngectomy.
Logemann (1998) later states that the radiographic study may be done to examine the physiology of the swallowing mechanism or to evaluate the effectiveness of a particular treatment strategy or the effects of recovery, and to identify the presence and cause of dysphagia. This therefore highlights the need for the aims of the VFS to be completed prior to the procedure so that the clinician has a plan in mind as to what to prepare, what to feed the patient and what to look for. If there are no specific aims, e.g. effect of lateral head turn, the patient may be placed at some degree of danger of unnecessary aspiration due to incorrect head positioning.
Familiarizing yourself with the normal anatomical features and common anatomical variants of the structures involved in swallowing, plus other structures of the head and neck as shown in Figure 7.1 (e.g. level and positioning of cervical and thoracic spine in relation to cricopharyngeus etc.) will undoubtedly help to increase understanding as to the interpretation of images obtained during a videofluoroscopy. In addition to this, observation of a normal oropharyngeal swallow during videofluoroscopy/barium swallow, as in the timing, strength and location of trigger of swallow, bolus management at each of the stages listed and anatomical shift during swallowing will help to appreciate and evaluate the images obtained when difficulties with the swallow arise. Accurate interpretation is essential by the team to allow the therapist, medical team and, inevitably, the patient manage the dysphagia in a safe and productive manner. This then gives rise to repeat examinations to evaluate the change/improvement and increase skills even further.
College of Radiographers. Clinical governance. London: College of Radiographers, 1999.
Daniels S.K., McAdam C.P., Brailey K., Foundas A.L. Clinical assessment of swallowing and prediction of dysphagia severity. Am. J. Speech. Lang. Patho.. 1997;6(4):17-23.
Farrow R., Stevenson G.W. Gastrointestinal tract. In: Armstrong P., Wastie M.L., editors. Diagnostic and interventional radiology in surgical practice. London: Chapman & Hall, 1997.
Langmore S.E., Schatz K., Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann. Otol. Rhinol. Laryngo.. 1991;100:678-681.
Logemann J.A. Evaluation and treatment of swallowing disorders, second ed. Austin: PRO-ED, 1998.
Martino R., Pron G., Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia. 2000;15(1):19-30.
Meijing L., Brasseur J.G., Kern M.K., Dodds W.J. Viscosity measurements of barium sulfate mixtures for use in motility studies of the pharynx and esophagus. Dysphagia. 1992;7:17-30.
Nightingale J. Developing protocols for advanced and consultant practice. Radiography. 2008. doi:10.1016/j.radi.2008.04.001
Owen A., Hogg P., Nightingale J. A critical analysis of a locally agreed protocol for clinical practice. Radiography. 2004;10:139-144.
Power M., Laasch H.U., Kasthuri R.S., Nicholson D.A., Hamdy S. Videofluoroscopic assessment of dysphagia: a questionnaire survey of protocols, roles and responsibilities of radiology and speech and language therapy personnel. Radiography. 2006;12:26-30.
Robbins J.A., Coyle J.L., Rosenbek J.C., Roecker E.B., Woods J.L. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia. 1999;14(4):228-232.
Royal College of Speech and Language Therapists. Videofluoroscopic evaluation of oropharyngeal swallowing disorders (vfs) in adults: the role of speech and language therapists. 2006. RCSLT Policy Statement
Skills for Health. Direct and report on video fluoroscopic examinations of the oro-pharynx and oesophagus using contrast media. 2005. Online http://www.skillsforhealth.org.uk/tools/view_framework.php?id=103 [Accessed 19.11.07]