Chapter 3 Vertebral Augmentation: What Is the Role of Vertebroplasty and Kyphoplasty?
Osteoporosis is a disorder characterized by decre-ased bone density, disruption of trabecular architecture, and increased susceptibility to fractures. There are approximately 700,000 vertebral body compression fractures (VCFs) occur in the United States each year.1 Approximately 70,000 of those result in hospitalization, with an average hospital stay per patient of 8 days.2 The lifetime risk for a clinically evident vertebral fracture among postmenopausal white women older than 50 years has been estimated at about 16%, whereas the lifetime risk in white men is about 5%.3 Clinical evidence shows that, if untreated, up to 20% of patients with a prior VCF are likely to have an additional VCF within the same year.4 The diagnosis of a single osteoporotic VCF increases the risk for subsequent fractures by a factor of 5. Patient population studies suggest an increased mortality rate in patients with osteoporotic VCFs that correlates with the number of fractured vertebrae.1 A benign natural history has long been assumed for osteoporotic VCFs, but up to 30% of those who are symptomatic and seek treatment do not respond adequately to nonsurgical treatment.5,6
VERTEBRAL AUGMENTATION
Historically, “percutaneous vertebroplasty” was conceived in France in 1984 to reduce pain from symptomatic vertebral hemangiomas.7 A cervical vertebra was injected with acrylic cement during open surgery to strengthen the vertebral body. An analgesic effect was noted, and indications for the technique expanded to include both neoplastic disease and osteoporotic compression fractures through a percutaneous insertion of cannulas into the vertebral body, through which cement was injected.
The “kyphoplasty” technique was developed later in 1997; it is a minimally invasive technique that helps restore vertebral body height before cement augmentation.8 It involves inserting inflatable bone tamps, through percutaneously placed cannulas, into the vertebral body under fluoroscopic guidance. Once inflated, the bone tamps push up on the end plates, helping to reduce the loss of vertebral body height while creating a cavity for the bone cement.
The traditional indications for vertebral augmentation are progressive collapse of a vertebral body and intractable pain. Either a transpedicular or extrapedicular approach is used to reach the vertebral body. Contraindications to vertebral augmentation are systemic pathology such as sepsis, prolonged bleeding times, or cardiopulmonary pathology, which would preclude the safe completion of the procedure. Other relative contraindications include patients presenting with neurological signs or symptoms, nonosteolytic infiltrative spinal metastases, vertebral height collapse of more than 60%, burst fractures, or vertebral bodies with deficient posterior cortices9,10 (Tables 3-1 and 3-2).
REVIEW OF THE LITERATURE
Several reports with higher levels of evidence have been published. However, no blinded randomized trials have compared either technique against medical management. One was a multicenter prospective study of kyphoplasty.11 Two were concurrently controlled prospective studies comparing kyphoplasty with nonsurgical management.12,13 There were two concurrently controlled prospective studies,14,15 and one nonconcurrently controlled study comparing vertebroplasty with nonsurgical management.16 Several studies compared kyphoplasty and vertebroplasty. However, most were nonconcurrent comparisons,17–19and two were unclear.20,21 Several meta-analyses compared kyphoplasty and vertebroplasty,22–24 and there were also several meta-analyses of only kyphoplasty or only vertebroplasty.25–28
SYSTEMATIC REVIEW OF VERTEBRAL AUGMENTATION OUTCOMES
Taylor et al23 performed a systematic review and metaregression to compare the efficacy and safety of balloon kyphoplasty and vertebroplasty for the treatment of VCFs, and to examine the prognostic factors that predict outcome. They found Level III evidence to support both balloon kyphoplasty and vertebroplasty as effective therapies in the management of patients with symptomatic osteoporotic VCFs refractory to conventional medical therapy. However, balloon kyphoplasty appeared to offer a better adverse event profile.
In a follow-up study, the authors concluded that in direct comparison with conventional medical management, patients undergoing kyphoplasty experienced superior improvements in pain, functionality, vertebral height, and kyphotic angle at least up to 3 years after the procedure. Reductions in pain with kyphoplasty appeared to be greatest in patients with newer fractures. The authors concluded that balloon kyphoplasty appeared to be more effective than medical management of osteoporotic VCFs and as least as effective as vertebroplasty.26
Hulme22 conducted a systematic review of 69 studies in the literature. The objective of the review was to evaluate the safety and efficacy of vertebroplasty and kyphoplasty using the data presented in published clinical studies, with respect to patient pain relief, restoration of mobility and vertebral body height, complication rate, and incidence of new adjacent vertebral fractures. A large proportion of subjects had some pain relief, including 87% with vertebroplasty and 92% with kyphoplasty. Vertebral height restoration was possible using kyphoplasty (average, 6.6 degrees) and for a subset of patients using vertebroplasty (average, 6.6 degrees). Cement leaks occurred for 41% and 9% of treated vertebrae for vertebroplasty and kyphoplasty, respectively. New fractures of adjacent vertebrae occurred for both procedures at rates that are greater than the general osteoporotic population but approximately equivalent to the general osteoporotic population that had a previous vertebral fracture. The authors concluded that the problem with stating definitively that vertebroplasty and kyphoplasty are safe and effective procedures was the lack of comparative, blinded, randomized, clinical trials.22
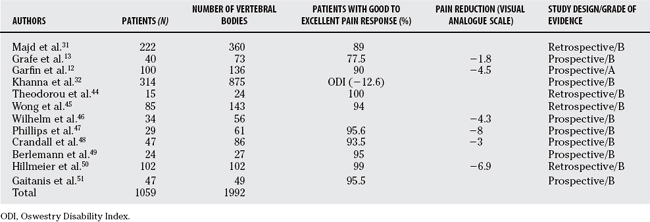
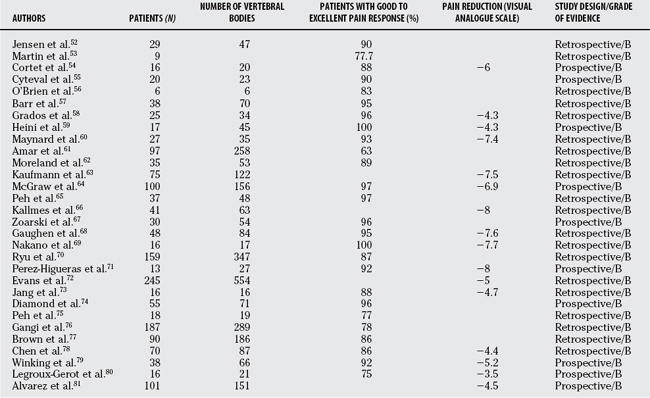
In a review of cumulative data from 1279 vertebral bodies treated with kyphoplasty and 2729 vertebral bodies treated with vertebroplasty, Hadjipavlou and researchers30 found that the mean good to excellent pain response was reported by 90% of patients treated with vertebroplasty and 95.6% of patients treated with kyphoplasty. Vertebroplasty was associated with a 29% rate of cement leakage compared with 8.4% for kyphoplasty. The rate of epidural leakage was 10.7% with vertebroplasty and 1.2% for kyphoplasty. The series included VCF secondary to osteoporosis and tumor.29
DOES VERTEBRAL AUGMENTATION IMPROVE OUTCOME IN PATIENTS WITH VERTEBRAL COMPRESSION FRACTURES?
In a prospective, nonrandomized, “intention-to-treat” study, Diamond and investigators14 treated 126 consecutive patients (39 men and 87 women; ages 51–95 years) with acute osteoporotic vertebral fractures. Eighty-eight patients were treated by percutaneous vertebroplasty and 38 by conservative therapy. The primary outcome measure was change in the patients’ pain score and level of function at 24 hours, 6 weeks, 6 to 12 months, and 24 months after therapy. Secondary outcome measures were occurrence of new clinical or radiological vertebral fractures and survival at 2 years. Outcomes in patients treated with vertebroplasty showed greater reduction in visual analogue pain scores, faster return to normal function, and lower rates of hospitalization when compared with those treated conservatively (P < 0.001 for the comparison of all variables at 24 hours). Lower pain scores persisted in the group treated with vertebroplasty at 6 weeks (P < 0.001), but no differences between the two groups were evident at 12 and 24 months. In the group treated with vertebroplasty, compared with the control group, the rates of new vertebral fractures and death showed no significant difference. The authors concluded that the analgesic benefit of percutaneous vertebroplasty and the low complication rates suggest that cement augmentation is a useful therapy for acute painful osteoporotic vertebral fractures.14
Alvarez and colleagues15 performed a prospective study consisting of 101 consecutive patients who underwent vertebroplasty and 27 patients who refused operative treatment and were managed conservatively. Patients who elected for vertebroplasty as a treatment of their fractures had significantly more pain and functional impairment before the procedure than the patients in the conservative group (P < 0.001). Vertebroplasty demonstrated a rapid and significant relief of pain and improved the quality of life.15
Majd and researchers30 prospectively followed 222 osteoporotic patients with 360 VCFs who were treated with kyphoplasty. Immediate pain relief was reported by 89% of patients at the first follow-up visit. One patient experienced postoperative pain as a result of radiculopathy related to leakage into the foramen. Sixty-nine percent of fractures exhibited restoration of lost vertebral height. Twelve percent (30/254) of the patients required additional kyphoplasty procedures to treat 36 symptomatic, new adjacent and remote fractures.30
Studies comparing kyphoplasty with conventional medical treatment found that kyphoplasty consistently improved pain and physical function, with results sustained at 12 months.12 In addition, the authors found that there were significantly fewer patients with new vertebral fractures of the thoracic and lumbar spine, after 12 months, in the kyphoplasty group than in the group treated medically. Another benefit of the kyphoplasty technique is the restoration of mobility. Garfin and investigators11 demonstrated that elderly patients with VCFs had rapid, significant, and sustained improvements in back pain, back function, and quality of life after balloon kyphoplasty.
Khanna and colleagues31 prospectively followed 155 patients with VCFs secondary to osteoporosis and 56 patients with malignant osteolysis for a mean 55.0 weeks after kyphoplasty. The average Owestry Disability Index score decreased by 12.6 points (P < 0.001) in the overall group, by 11.8 points (P < 0.001) at short-term follow-up, and by 8.6 points (P < 0.001) at long-term follow-up. All Health Survey Short Form-36 subscores except for general health and role-emotional showed statistically significant improvement from baseline values at the same time points. No statistically significant difference was found for functional outcome in the osteoporosis and multiple myeloma subgroups.31
DOES VERTEBRAL AUGMENTATION RESTORE VERTEBRAL HEIGHT AND SAGITTAL ALIGNMENT?
In a study of vertebroplasty, Jang and coworkers32 report that the mean anterior vertebral height, as measured on the standing flexion radiographs before operation, improved from 14.8 mm to 21.8 mm with extension of the spine in a series of patients with single fractures. After vertebroplasty, the mean anterior height was 19.8 mm, suggesting that considerable height restoration can be achieved by postural extension and then be preserved by vertebroplasty. Some reports suggest that the age of the fracture is a major determinant in achieving an optimal reduction,33,34 whereas others demonstrate that significant correction can be achieved even in fractures older than 3 months.33,35 In a study of kyphoplasty, Crandall and coauthors33 reported failure of significant correction in 20% of chronic fractures compared with 8% of acute fractures.33
Pradhan and colleagues36 examined the effects of single-level and multilevel kyphoplasty procedures on local and overall sagittal alignment of the spine. The authors found that the majority of kyphosis correction is limited to the vertebral body treated. The majority of height gained after kyphoplasty occurs in the midbody. Higher correction over longer spans of the spine can be achieved with multilevel kyphoplasty procedures, in proportion to the number of levels addressed. The authors felt that it would be unrealistic to expect a one- or two-level kyphoplasty to significantly improve the overall sagittal alignment of the spine.
Shindle and coworkers37 prospectively followed 25 consecutive patients with a total of 43 osteoporotic VCFs to evaluate the effect of postural changes and balloon inflation on vertebral fracture reduction. Their findings support the concept that many VCFs can be moved with positioning. However, balloon kyphoplasty enhanced the height reduction by an amount equal to or greater than 4.5-fold over the positioning maneuver alone and accounted for more than 80% of the ultimate reduction. The authors concluded that if height restoration is the goal, kyphoplasty is clearly superior in most cases to the positioning maneuver alone.37
Voggenreiter has demonstrated that placement of the patient in the prone position displayed a significant spontaneous reduction in deformity of 6.5 degrees ± 4.1 degrees Cobb angle. Inflation of the inflatable bone tamp demonstrated a further reduction of the fracture and a significant improvement of the Cobb angle of 3.4 degrees compared with baseline prone position. After deflation and removal of the inflatable bone tamp and placement of the cement, no significant loss of fracture reduction was seen. Postoperative measurement of the Cobb angle by means of standing radiographs demonstrated a 3.1-degree loss of reduction compared with the intraoperative measurement in prone position after cement application.38
DOES VERTEBRAL AUGMENTATION PREDISPOSE TO FURTHER VERTEBRAL COMPRESSION FRACTURES?
Painful osteoporotic compression fractures can be effectively treated with methylmethacrylate vertebral augmentation, but the effect of intervention on the generation of future remote and adjacent fractures remains a topic of debate. A VCF causes a local kyphotic deformity. This deformity moves the center of gravity forward, resulting in an increased forward bending moment. This increases the load on the adjacent vertebrae and predisposes it to fracture. Silverman et al4 showed that, if untreated, up to 20% of patients with a prior VCF are likely to have an additional VCF within the same year. The authors also reported that 58% of women with one or more fractures had adjacent fractures.39 The rates of new fracture after cement augmentation procedures are not comparable among patients treated with vertebroplasty (0–52%), kyphoplasty (5.8–36.8%), and conservative approaches (19.2–58%), because of the poor scientific design of the studies. Most are retrospective or nonrandomized prospective reports29 (Table 3-3).
TABLE 3-3 Literature Regarding Possible Predisposition of Vertebral Augmentation to Further Vertebral Compression Fractures
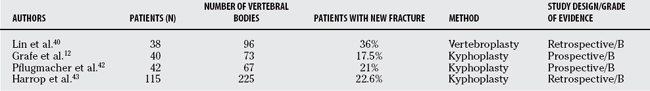
Lin and colleagues40 treated 38 patients with vertebroplasty and found that 14 patients developed new fractures during the follow-up period. Seventy-one percent of patients with secondary fractures had intradiscal leakage of cement. In their study, vertebral bodies adjacent to a disc with leakage of cement had a 58% chance of developing a new fracture compared with 12% of vertebral bodies adjacent to a disc without leakage. The authors concluded that leakage of cement into the disc, by impeding the flexibility, may increase the risk for a secondary fracture in an adjacent vertebral body.40 Trout and coworkers44 performed a retrospective review of 86 patients treated with vertebroplasty to identify those who developed adjacent segment fractures.41 They found that 186 incident fractures developed in these 86 patients. Seventy-seven (41%) of these incident fractures occurred adjacent to treated vertebrae.
Reduction of the kyphotic deformity with kyphoplasty may potentially decrease the risk for new fractures. Two prospective, nonrandomized studies compared kyphoplasty with conservative treatment. Grafe and coworkers12,13 found that at 12-month follow up, 50% of patients who had been treated conservatively developed secondary fractures, compared with 17.5% of patients who had undergone kyphoplasty.12,13 Komp and coauthors12,13 report that at 6-month follow-up examination, the incidence of new fractures in 17 conservatively treated patients was 65%, compared with 37% in 19 patients treated by kyphoplasty.13,14 However, these were not randomized studies.
Pflugmacher and researchers42 conducted a 2-year prospective follow-up to evaluate the incidence of adjacent vertebral fractures in patients treated with balloon kyphoplasty. It did not include comparison or control groups. The authors reported an annualized refracture rate of 10%.42 In 8 patients (21.6%; 5 female and 3 male patients), an adjacent fracture occurred in 11 vertebrae (18.3%) within 3 weeks to 22 months of follow-up (after 22 months, no adjacent fracture occurred). In three patients, the adjacent fractures were asymptomatic. Five patients with symptomatic adjacent fractures (eight vertebrae) were treated again with balloon kyphoplasty.
Harrop and colleagues43 treated 225 vertebral bodies in 115 patients using the kyphoplasty technique, and patients were followed prospectively. Of those, 26 patients developed 34 subsequent compression fractures. The mean follow-up was 11 months (range, 3–33 months). The incidence of subsequent fracture per procedure per kyphoplasty was 15.1% (34 of 225). The overall incidence rate per patient was 22.6% (26 of 115). Seventeen of the 26 (65%) patients with subsequent fracture had secondary steroid-induced osteoporosis, while only 9 of the 26 (35%) had primary osteoporosis. Therefore, the incidence of postkyphoplasty vertebral compression fractures in patients with primary osteoporosis was 11.25% (9 of 80), and the incidence in patients with steroid-induced osteoporosis was 48.6% (17 of 35). This increased fracture rate in the steroid-dependent patients was significantly greater than in patients with primary osteoporosis (P < 0.0001), together with a significantly greater proportion of adjacent fractures (12 of 19 taking steroids; P = 0.0009) and remote fractures (7 of 9 taking steroids; P = 0.027) compared with the patients with primary osteoporosis.43
As the population ages and osteoporosis becomes more prevalent, the incidence of symptomatic vertebral compression fractures will increase. For those with severe pain or progressive collapse, early vertebral augmentation, either kyphoplasty or vertebroplasty, affords excellent early pain relief, early return to function, and some restoration of local sagittal alignment. Recent 2-year follow-up data suggest that the benefits of the procedure persist with time. Table 3-4 provides a summary of recommendations
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
1 Cooper C, et al. Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res. 1992;7:221-227.
2 Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006;6:479-487.
3 Melton LJ3rd, Kallmes DF. Epidemiology of vertebral fractures: Implications for vertebral augmentation. Acad Radiol. 2006;13:538-545.
4 Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1992;13(suppl 2):S27-S31.
5 Melton LJ3rd, et al. Epidemiology of vertebral fractures in women. Am J Epidemiol. 1989;129:1000-1011.
6 Wasnich RD. Vertebral fracture epidemiology. Bone. 1996;18(3 suppl):179S-183S.
7 Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie. 1987;33:166-168.
8 Lieberman IH, et al. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:1631-1638.
9 Bai B, et al. The use of an injectable, biodegradable calcium phosphate bone substitute for the prophylactic augmentation of osteoporotic vertebrae and the management of vertebral compression fractures. Spine. 1999;24:1521-1526.
10 Cotten A, et al. Percutaneous vertebroplasty: State of the art. Radiographics. 1998;18:311-323.
11 Garfin SR, Buckley RA, Ledlie J. Balloon kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine. 2006;31:2213-2220.
12 Grafe IA, et al. Reduction of pain and fracture incidence after kyphoplasty: 1-year outcomes of a prospective controlled trial of patients with primary osteoporosis. Osteoporos Int. 2005;16:2005-2012.
13 Komp M, Ruetten S, Godolias G. Minimally invasive therapy for functionally unstable osteoporotic vertebral fracture by means of kyphoplasty: prospective comparative study of 19 surgically and 17 conservatively treated patients. J Miner Stoffwechs. 2004;11(suppl 1):13-15.
14 Diamond TH, et al. Clinical outcomes after acute osteoporotic vertebral fractures: A 2-year non-randomised trial comparing percutaneous vertebroplasty with conservative therapy. Med J Aust. 2006;184:113-117.
15 Alvarez L, et al. Percutaneous vertebroplasty: Functional improvement in patients with osteoporotic compression fractures. Spine. 2006;31:1113-1118.
16 Nakano M, et al. Calcium phosphate cement-based vertebroplasty compared with conservative treatment for osteoporotic compression fractures: A matched case-control study. J Neurosurg Spine. 2006;4:110-117.
17 Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 2003;98:21-30.
18 Grohs JG, Matzner M, Trieb K, Krepler P. Minimal invasive stabilization of osteoporotic vertebral fractures: A prospective nonrandomized comparison of vertebroplasty and balloon kyphoplasty. J Spinal Disord Tech. 2005;18:238-242.
19 Masala S, Schillaci O, Massari F. MRI and bone scan imaging in the preoperative evaluation of painful vertebral fractures treated with vertebroplasty and kyphoplasty. In Vivo. 2005;19:1055-1060.
20 Pflugmacher R, Kandziora F, Schröder R, et al. [Vertebroplasty and kyphoplasty in osteoporotic fractures of vertebral bodies—a prospective 1-year follow-up analysis]. Rofo. 2005;177:1670-1676.
21 Köse KC, Cebesoy O, Akan B, et al. Functional results of vertebral augmentation techniques in pathological vertebral fractures of myelomatous patients. J Natl Med Assoc. 2006;98:1654-1658.
22 Hulme PA, et al. Vertebroplasty and kyphoplasty: A systematic review of 69 clinical studies. Spine. 2006;31:1983-2001.
23 Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: A comparative systematic review of efficacy and safety. Spine. 2006;31:2747-2755.
24 Hadjipavlou AG, Tzermiadianos M, Katonis PG, Szpalski M. Percutaneous vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures and osteolytic tumours. J Bone Joint Surg Br. 2005;87:1595-1604.
25 Taylor RS, Fritzell P, Taylor RJ. Balloon kyphoplasty in the management of vertebral compression fractures: An updated systematic review and meta-analysis. Eur Spine J. 2007;16:1085-1100.
26 Bouza C, Lopez T, Magro A, et al. Efficacy and safety of balloon kyphoplasty in the treatment of vertebral compression fractures: A systematic review. Eur Spine J. 2006;15:1050-1067.
27 Ploeg WT, Veldhuizen AG, The B, Sietsma MS. Percutaneous vertebroplasty as a treatment for osteoporotic vertebral compression fractures: A systematic review. Eur Spine J. 2006;15:1749-1758.
28 Hochmuth K, Proschek D, Schwarz W, et al. Percutaneous vertebroplasty in the therapy of osteoporotic vertebral compression fractures: A critical review. Eur Radiol. 2006;16:998-1004.
29 Hadjipavlou AG, et al. Percutaneous vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures and osteolytic tumours. J Bone Joint Surg Br. 2005;87:1595-1604.
30 Majd ME, Farley S, Holt RT. Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J. 2005;5:244-255.
31 Khanna AJ, et al. Functional outcomes of kyphoplasty for the treatment of osteoporotic and osteolytic vertebral compression fractures. Osteoporos Int. 2006;17:817-826.
32 Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine. 2003;28:1588-1592.
33 Crandall D, et al. Acute versus chronic vertebral compression fractures treated with kyphoplasty: Early results. Spine J. 2004;4:418-424.
34 Berlemann U, et al. Kyphoplasty for treatment of osteoporotic vertebral fractures: A prospective non-randomized study. Eur Spine J. 2004;13:496-501.
35 Gaitanis IN, et al. Restoring geometric and loading alignment of the thoracic spine with a vertebral compression fracture: Effects of balloon (bone tamp) inflation and spinal extension. Spine J. 2005;5:45-54.
36 Pradhan BB, et al. Kyphoplasty reduction of osteoporotic vertebral compression fractures: Correction of local kyphosis versus overall sagittal alignment. Spine. 2006;31:435-441.
37 Shindle MK, et al. Vertebral height restoration in osteoporotic compression fractures: Kyphoplasty balloon tamp is superior to postural correction alone. Osteoporos Int. 2006;17:1815-1819.
38 Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30:2806-2812.
39 Silverman SL, et al. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: Results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum. 2001;44:2611-2619.
40 Lin EP, et al. Vertebroplasty: Cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25:175-180.
41 Trout AT, Kallmes DF, Kaufmann TJ. New fractures after vertebroplasty: adjacent fractures occur significantly sooner. AJNR Am J Neuroradiol. 2006;27(1):217-223.
42 Pflugmacher R, Schroeder RJ, Klostermann CK. Incidence of adjacent vertebral fractures in patients treated with balloon kyphoplasty: Two years’ prospective follow-up. Acta Radiol. 2006;47:830-840.
43 Harrop JS, et al. Primary and secondary osteoporosis’ incidence of subsequent vertebral compression fractures after kyphoplasty. Spine 2004. 2004;29:2120-2125.
44 Theodorou DJ, Theodorou SJ, Duncan TD, Garfin SR, Wong WH. Percutaneous balloon kyphoplasty for the correction of a spinal deformity in painful vertebral compression fractures. Clin Imaging. 2002;26:1-5.
45 Wong WH, Olan WJ, Belkoff SM. Balloon kyphoplasty. In: Mathis JM, Deramond H, Belkoff SM, editors. Percutaneous vertebroplasty. New York: Springer-Verlag; 2002:109-124.
46 Wilhelm K, Stoffel M, Ringel F, et al. Preliminary experience with balloon kyphoplasty for the treatment of painful osteoporotic compression fractures. Rofo. 2003;177:1690-1696. (in German)
47 Phillips FM, Ho E, Campbell-Hupp M, et al. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003;28:2260-2267.
48 Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J. Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine J. 2004;4:418-424.
49 Berlemann U, Franz T, Orler R, Heini PF. Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J. 2004;13:496-501.
50 Hillmeier J, Grafe I, Da Fonseca K, et al. The evaluation of balloon kyphoplasty for osteoporotic vertebral fractures: an interdisciplinary concept. Orthopade. 2004;33:893-904. (in German).
51 Gaitanis I, Hadjipavlou AG, Katonis PG, et al. Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J. 2005;14:250-260.
52 Jensen ME, Evans AJ, Mathis JM, et al. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol. 1997;18:1897-1904.
53 Martin JB, Jean B, Sugiu K, et al. Vertebroplasty: clinical experience and followup results. Bone. 1999;25(2 Suppl):11-15.
54 Cortet B, Cotten A, Boutry N, et al. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: an open prospective study. J Rheumatol. 1999;26:2222-2228.
55 Cyteval C, Sarrabère M, Roux JO, et al. Acute osteoporotic vertebral collapse: open study on percutaneous injection of acrylic surgical cement in 20 patients. AJR Am J Roentgenol. 1999;173:1685-1690.
56 O’Brien JP, Sims JT, Evans AJ. Vertebroplasty in patients with severe vertebral compression fractures: a technical report. AJNR Am J Neuroradiol. 2000;21:1555-1558.
57 Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000;25:923-928.
58 Grados F, Depriester C, Cayrolle G, et al. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology. 2000;39:1410-1414.
59 Heini PF, Wälchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results: a prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000;9:445-450.
60 Maynard AS, Jensen ME, Schweickert PA, et al. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am J Neuroradiol. 2000;21:1807-1812.
61 Amar AP, Larsen DW, Esnaashari N, et al. Percutaneous transpedicular polymethylmethacrylat vertebroplasty for the treatment of spinal compression fractures. Neurosurgery. 2001;49:1105-1114.
62 Moreland DB, Landi MK, Grand W. Vertebroplasty: techniques to avoid complications. Spine J. 2001;1:66-71.
63 Kaufmann TJ, Jensen ME, Schweickert P, Marx WF, Kallmes DF. Age of fracture and clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2001;22:1860-1863.
64 McGraw JK, Lippert JA, Minkus KD, et al. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol. 2002;13:883-886.
65 Peh WC, Gilula LA, Peck DD. Percutaneous vertebroplasty for severe osteoporotic vertebral body compression fractures. Radiology. 2002;223:121-126.
66 Kallmes DF, Schweickert PA, Marx WF, Jensen ME. Vertebroplasty in the mid and upper thoracic spine. AJNR Am J Neuroradiol. 2002;23:1117-1120.
67 Zoarski GH, Snow P, Olan WJ, et al. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J Vas Interv Radiol. 2002;13:139-148.
68 Gaughen JR, Jensen ME, Schweickert PA, et al. Relevance of antecedent venography in percutaneous vertebroplasty for the treatment of osteoporotic compression fractures. AJNR Am J Neuroradiol. 2002;23:594-600.
69 Nakano M, Hirano N, Matsura K, et al. Percutaneous transpedicular vertebroplasty with calcium phosphate cement in the treatment of osteoporotic vertebral compression and burst fractures. J Neurosurg Spine. 2002;97:287-293.
70 Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg Spine. 2002;96:56-61.
71 Perez-Higueras A, Alvarez L, Rossi R, Quinones D, Al-Assir I. Percutaneous vertebroplasty: long-term clinical and radiological outcome. Neuroradiology. 2002;44:950-954.
72 Evans AJ, Jensen ME, Kip KE, et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty: retrospective report of 245 cases. Radiology. 2003;226:366-372.
73 Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine. 2003;28:1588-1592.
74 Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med. 2003;114:257-265.
75 Peh WC, Gelbart MS, Gilula LA, Peck DD. Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol. 2003;180:1411-1417.
76 Gangi A, Guth S, Imbert JP, Marin H, Dietermann JL. Percutaneous vertebroplasty: indications, technique, and results. Radiographics. 2003;23:10.
77 Brown DB, Glaiberman CB, Sehgal M, Shimony JS. Treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. Am J Roentgenol. 2004;182:319-322.
78 Chen LH, Niu CC, Yu SW, et al. Minimally invasive treatment of osteoporotic vertebral compression fracture. Chang Gung Med J. 2004;27:261-267.
79 Winking M, Stahl JP, Oertel M, Schnettler R, Boker DK. Treatment of pain from osteoporotic vertebral collapse by percutaneous PMMA vertebroplasty. Acta Neurochir (Wien). 2004;146:469-476.
80 Legroux-Gerot I, Lormeau C, Boutry N, et al. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol. 2004;23:310-317.
81 Alvarez L, Pérez-Higueras A, Quinones D, Calvo E, Rossi RE. Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life. Eur Spine J. 2003;12:356-360.