21 Ventricular septal defect
Salient features
Examination
• There are normal findings on palpation (there may be either left or right ventricular enlargement).
• With substantial left-to-right shunting and little or no pulmonary hypertension, the left ventricular impulse is dynamic and laterally displaced, and the right ventricular impulse may not be felt. The murmur of a moderate or large defect is pansystolic, loudest at the lower left sternal border, and usually accompanied by a palpable thrill.
• A short mid-diastolic apical rumble (caused by increased flow through the mitral valve) may be heard.
• A decrescendo diastolic murmur of aortic regurgitation may be present if the ventricular septal defect (VSD) undermines the aortic valve annulus.
• Small, muscular VSDs may produce high-frequency systolic ejection murmurs that terminate before the end of systole (when the defect is occluded by contracting heart muscle) (Fig. 21.1).
• If pulmonary hypertension develops, a right ventricular heave and a pulsation over the pulmonary trunk may be palpated. The pansystolic murmur and thrill diminish and eventually disappear as flow through the defect decreases, and a murmur of pulmonary regurgitation (Graham Steell’s murmur) may appear. Finally, cyanosis and clubbing are present.
• The second sound may be normal when the defect is small; A2 is obscured by the pansystolic murmur of large defects. A single second sound indicates that the ventricular pressures are equal and a loud P indicates pulmonary hypertension.
Questions
How would you investigate this patient?
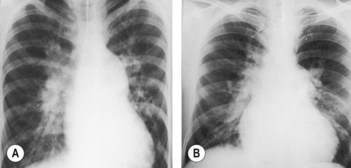
• ECG and chest radiography provide insight into the magnitude of the haemodynamic impairment: with a small ventricular septal defect, both ECG and chest radiograph are normal:
• Doppler echocardiography can identify the presence and location of the ventricular septal defect, and Doppler colour-flow mapping can identify the magnitude and direction of shunting.
• Magnetic resonance imaging (MRI).
• Cardiac catheterization and angiography can confirm the presence and location of the ventricular septal defect, as well as determine the magnitude of shunting and the pulmonary vascular resistance.
Advanced-level questions
What types of ventricular septal defect do you know?
• The supracristal type (above the crista supraventricularis, a muscular ridge that separates the main portion of the right ventricular cavity from the infundibular or outflow portion) is a high defect just below the pulmonary valve and the right coronary cusp of the aortic valve. The latter may not be adequately supported, resulting in aortic regurgitation. In Fallot’s tetralogy, this defect is associated with a rightward shift of the interventricular septum, and in double-outlet LV with subaortic stenosis the supracristal defect is associated with a leftward shift of the septum.
• The infracristal defect, which may be in either the upper membranous portion of the interventricular septum or the lower muscular part (<5% of the defects):
Mention other cardiac lesions that may be associated with a ventricular septal defect
What is the effect of pregnancy in women with a ventricular septal defect?
• Small defects should present with no problems.
• Moderate-sized defects and moderate pulmonary hypertension are at the risk of developing acute right ventricular failure and rapidly worsening pulmonary hypertension in pregnancy.
• Pregnancy should be avoided in pulmonary hypertension and pregnancy.
What is the management of patients with a ventricular septal defect?
• The natural history of ventricular septal defect depends on:
• Adults with small defects and normal pulmonary arterial pressure are usually asymptomatic, and pulmonary vascular disease is unlikely to develop. Such patients do not require surgical closure of their defect, but they are at risk for infective endocarditis and should, therefore, receive antibiotic prophylaxis.
• Patients with large VSDs who survive to adulthood usually have left ventricular failure or pulmonary hypertension with associated right ventricular failure. Surgical closure of such defects is recommended, if the magnitude of pulmonary vascular obstructive disease is not prohibitive. Once the ratio of pulmonary to systemic vascular resistance exceeds 0.7, the risk associated with surgery is excessive.
Which patients merit surgical attention?
• Development of aortic regurgitation caused by prolapse of the right coronary cusp through the septal defect
• Progressive left ventricular dilatation caused by volume overload imposed by the shunt (pulmonary to systemic ratio is 3:1)
• When the defect is caused by an acute rupture of the ventricular septum.