CHAPTER 11 VENTILATOR MANAGEMENT
PRETEST QUESTIONS
1. The following information has been obtained from a ventilator patient.
| Peak inspiratory pressure | 48 cm H2O |
| Plateau pressure | 27 cm H2O |
| VT | 850 mL |
| PEEP | 4 cm H2O |
2. A volume-cycled ventilator is in the control mode and the I:E inspiratory/expiratory ratio alarm is sounding. Which control adjustment would correct this problem?
3. Mechanical ventilation can lead to which of the following complications?
4. Static lung compliance will decrease as a result of which of the following?
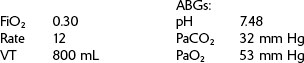
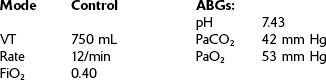
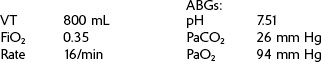
5. These data have been collected from a patient whose ventilator was in the control mode.
To increase this patient’s PaCO2 to 40 mm Hg, the ventilator rate should be adjusted to what level?
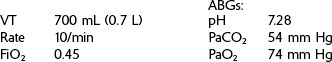
6. The following data have been collected from a patient using a volume ventilator in the control mode.
REVIEW
CRT Exam Content Matrix: IIA6a-b, IIA11a, d, IIID2c, IIID10, IIIF2i6,9, IIIG3f,i,k, l
RRT Exam Content Matrix: IIA2a-b, IIID2c, IIID8, IIIF2e6, IIIG3f,h,k
CRT Exam Content Matrix: IIID2b,d, IIIF2i1-5,11, IIIG3a-e
RRT Exam Content Matrix: IIID2b,d, IIIF2e1,2,3,4,5,9, IIIG3a-e
106 + [6 × (height in inches − 60 in)]
105 + [5 × (height in inches − 60 in)]
EXAMPLE:
Set VT at 200 mL (0.2 L). Peak pressure reached is 40 cm H2O.
This means that once the patient has started using the ventilator, 5 mL of the set tidal volume will be lost in the tubing for every 1 cm H2O registering on the manometer.
EXAMPLE:
Tubing compliance, 5 mL/cm H2O
Peak inspiratory pressure, 20 cm H2O
EXAMPLE:
Calculate the inspiratory time if the I:E ratio is 1 : 2 and the ventilator rate is 10/min.
EXAMPLE:
| PEEP (cm H2O) |
PaO2 (mm Hg) |
PvO2 (mm Hg) |
|---|---|---|
| 4 | 68 | 34 |
| 6 | 74 | 37 |
| 8 | 78 | 33 |
| 10 | 82 | 32 |
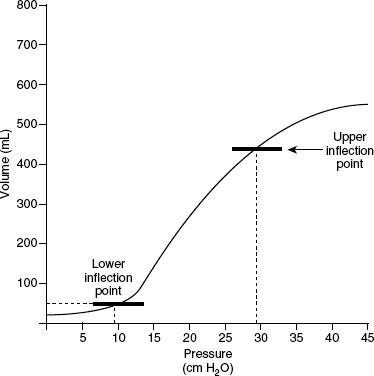
Figure 11-2 shows the lower inflection point (best PEEP level) to be about 10 cm H2O and the upper inflection point (best PIP level) to be about 28 to 30 cm H2O. Using a PEEP of 10 cm H2O keeps the alveoli from collapsing at end exhalation. Using a PIP of 28 to 30 cm H2O ventilates the lungs effectively while preventing overdistention of the alveoli.
III. VENTILATOR ALARMS AND MONITORING
CRT Exam Content Matrix: IA7d-e, IB9c,m, IB10c, IC6, IC9, IIIE4e, IIIE7b, IIIE9, IIIF2i7, IIIG3g
RRT Exam Content Matrix: IA7d-e, IB9c,m, IB10c, IIIE4b, IIIE5, IIIE7b
![]() Exam Note
Exam Note
The PIP level should be maintained at less than 35 to 40 cm H2O to prevent lung tissue damage.
 is commonly measured by a digital reading on a
is commonly measured by a digital reading on a  monitor, or it may be calculated with the use of the following equation
monitor, or it may be calculated with the use of the following equation
 is the level that improves oxygenation and ventilation without resulting in cardiovascular side effects and barotrauma.
is the level that improves oxygenation and ventilation without resulting in cardiovascular side effects and barotrauma. decreases, it indicates less pressure required to ventilate the patient’s lungs or an increased static lung compliance. An increased
decreases, it indicates less pressure required to ventilate the patient’s lungs or an increased static lung compliance. An increased  indicates higher pressure required to ventilate or a decreased static lung compliance.
indicates higher pressure required to ventilate or a decreased static lung compliance.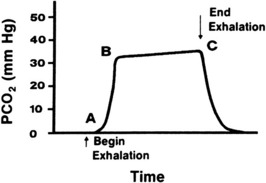
FIGURE 11-3 Capnography.
From Wilkins RL, Stoller JK, Kacmarek R: Egan’s fundamentals of respiratory care, ed 9, St Louis, 2009, Mosby.
IV. INDICATIONS FOR MECHANICAL VENTILATION
CRT Exam Content Matrix: IA7c,e, IB9d-e,j, IB10d,f
RRT Exam Content Matrix: IA7c,e, IB9d-e,j, IB10d,f
V. COMMON CRITERIA FOR INITIATION OF MECHANICAL VENTILATION
CRT Exam Content Matrix: IA7b,c,e, IB9d-e,j,m, IB10d-f
RRT Exam Content Matrix: IA7b,c,e, IB9d-e,j,m, IB10d-f
VI. COMPLICATIONS OF MECHANICAL VENTILATION
CRT Exam Content Matrix: IA7a, IB2-4, IB7a-b, IIIE6
RRT Exam Content Matrix: IA7a, IB2-4, IIIE6
CRT Exam Content Matrix: IB9k, IB10i, IB10k
RRT Exam Content Matrix: IB10i
CRT Exam Content Matrix: IA7d, IB9m, IB10m, IC6
RRT Exam Content Matrix: IA7d, IB9m, IB10n, IC7
EXAMPLE:
Given the following data, calculate the patient’s dynamic lung compliance.
| VT | 600 mL |
| PIP | 35 cm H2O |
| PEEP | 5 cm H2O |
EXAMPLE:
| VT | 800 mL |
| Plateau pressure | 25 cm H2O |
| PEEP | 5 cm H2O |
| Peak pressure | 45 cm H2O |
EXAMPLE:
| Time | Peak Pressure | Plateau Pressure |
|---|---|---|
| 6:00 AM | 28 cm H2O | 10 cm H2O |
| 7:00 AM | 34 cm H2O | 10 cm H2O |
| 8:00 AM | 42 cm H2O | 10 cm H2O |
EXAMPLE:
| Time | Peak Pressure | Plateau Pressure |
|---|---|---|
| 1:00 PM | 34 cm H2O | 16 cm H2O |
| 2:00 PM | 40 cm H2O | 22 cm H2O |
| 3:00 PM | 44 cm H2O | 26 cm H2O |
![]() Exam Note
Exam Note
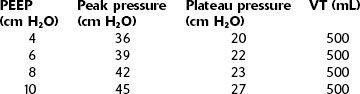
Calculation of lung compliance is also important in the determination of optimal PEEP level.
EXAMPLE:
The following data have been collected from a patient using a volume ventilator.
| Peak inspiratory pressure | 35 cm H2O |
| Plateau pressure | 20 cm H2O |
| Flow rate | 60 L/min = 1 L/s |
Because normal RAW in an intubated patient is around 5 cm H2O/L/s, this example reflects a high RAW.
IX. VENTILATION IN THE PATIENT WITH HEAD TRAUMA
X. WEANING FROM MECHANICAL VENTILATION
CRT Exam Content Matrix: IIID7, IIIF2i12, IIIG1g
RRT Exam Content Matrix: IIID6, IIIF2e10, IIIG1g
XI. HIGH-FREQUENCY VENTILATION
CRT Exam Content Matrix: IIID4
RRT Exam Content Matrix: IIA2c, IIID4
XII. ESTIMATING DESIRED VENTILATOR VARIABLE CHANGES
CRT Exam Content Matrix: IIID2b, IIIF2i2-3, IIIG3b-c
RRT Exam Content Matrix: IIID2b, IIIF2e2-3, IIIG3b-c
EXAMPLE:
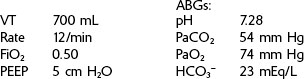
The data below are from a patient using a volume ventilator.
To increase this patient’s PaO2 to 80 mm Hg, to what level must the FiO2 be changed?
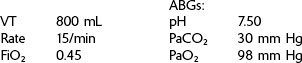
EXAMPLE:
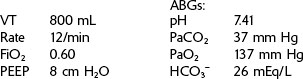
Data collected from a patient using a volume ventilator in the control mode.
To raise the patient’s PaCO2 to 35 mm Hg, the ventilator rate should be adjusted to what level?
EXAMPLE:
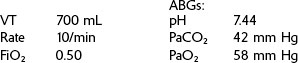
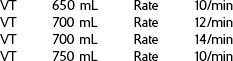
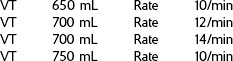
Below are data collected from a patient using a volume ventilator in the control mode.
Which of the following ventilator settings would decrease the patient’s PaCO2 to 45 mm Hg?
EXAMPLE:
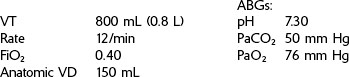
Below are data from a patient who is using a volume ventilator in the control mode.
Which of the following ventilator settings would decrease the patient’s PaCO2 to 40 mm Hg?
XIII. PRACTICE VENTILATOR PROBLEMS
CRT Exam Content Matrix: IIID2b, IIIF2i2-3, IIIG3b-c
RRT Exam Content Matrix: IIID2b, IIIF2e2-3, IIIG3b-c
What is the most appropriate ventilator change to recommend at this time?
What is the most appropriate recommendation at this time?
| VT | 800mL |
| Rate | 10/min |
| FiO2 | 0.35 |
| pH | 7.50 |
| PaCO2 | 29 mmHg |
| PaO2 | 97 mmHg |
| HCO3− | 25 mEq/L |
What would be the most appropriate ventilator change to make at this time?
What is the appropriate ventilator change at this time?
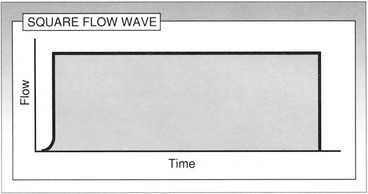
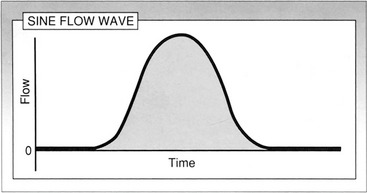
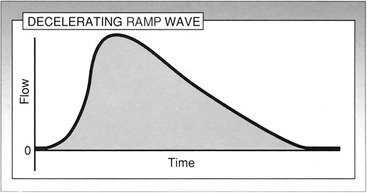
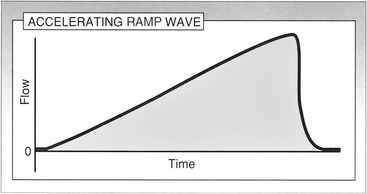
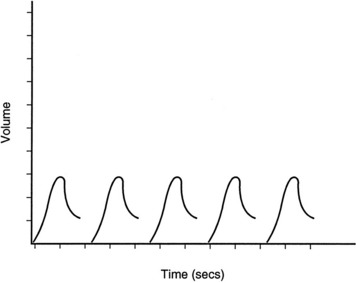
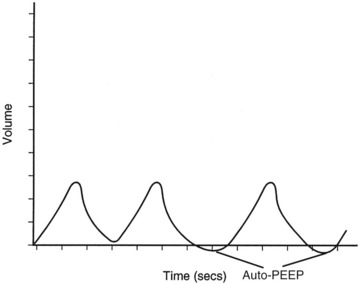
XIV. VENTILATOR FLOW, VOLUME, AND PRESSURE WAVEFORMS
CRT Exam Content Matrix: IIID3, IIIF2i8, IIIG3h,k
RRT Exam Content Matrix: IIID3, IIIF2e7, IIIG3g,j
FIGURE 11-8 Typical volume waveform.
Modified from Branson R, Hess D, Chatburn R: Respiratory care equipment, Philadelphia, 1999, Lippincott, Williams, and Wilkins.
XV. SUMMARY OF VENTILATOR ADJUSTMENTS ACCORDING TO ABG RESULTS
CRT Exam Content Matrix: IIID2b, IIIF2i2-3, IIIG3b-c
RRT Exam Content Matrix: IIID2b, IIIF2e2-3, IIIG3b-c
| ABG Abnormality | Ventilator Adjustment |
|---|---|
| No ventilator changes are necessary; administer HCO3−. |
XVI. MAINTENANCE OF THE VENTILATOR CIRCUIT
CRT Exam Content Matrix: IIB3, IIIF2i10, IIIG3j
XVII. VENTILATOR-ASSOCIATED PNEUMONIA
POSTCHAPTER STUDY QUESTIONS
1. Pressure control ventilation is most commonly used for adults with what lung condition?
2. What effect does decreasing lung compliance have on delivered VT in a neonate receiving pressure-limited ventilation?
3. What level of pressure support should be used for weaning so that airway resistance is overcome while breathing is spontaneous?
4. As the oxygenation status of a patient worsens while using an O2 mask, at what point should CPAP be employed?
5. How is minute ventilation calculated?
6. How is alveolar minute ventilation calculated?
7. Calculate the ventilator tubing compliance when the volume is set at 200 mL (0.2 L) and an inspiratory pressure of 50 cm H2O is generated.
8. Using the tubing compliance in question number 7, calculate the corrected VT when the patient is receiving a VT of 700 mL with a peak inspiratory pressure of 20 cm H2O.
9. On the initial ventilator setup, at what range should the ventilator rate be set?
10. How should the appropriate ventilator VT be determined?
11. List six indications for the use of PEEP.
12. List four hazards of PEEP.
14. After the PEEP level is increased, how can it be determined that cardiac output has been adversely affected?
15. How may the ventilator low-pressure alarm be activated?
16. List ways that the ventilator high-pressure alarm may be activated.
17. How should the high-pressure alarm be set?
18. List some factors that affect airway resistance (RAW).
20. List four conditions that result in a decreased PETCO2 reading.
21. List two conditions that result in an increased PETCO2 reading.
22. List six criteria that indicate mechanical ventilatory assistance is necessary.
23. List eight complications of mechanical ventilation.
24. Calculate the static lung compliance if the VT is 750 mL, PIP is 46 cm H2O, PEEP is 8 cm H2O, and plateau pressure is 28 cm H2O.
25. List some conditions that result in decreased lung compliance.
26. What is indicated if peak inspiratory pressures are increasing but the plateau pressure is not increasing?
27. List the criteria that patients should meet before they can begin to be weaned from the ventilator.
28. What respiratory rates are used with HFJV?
29. List four advantages of high-frequency ventilation over conventional ventilation.
30. A ventilator patient receiving an FiO2 of 0.30 has a PaO2 of 60 mm Hg. To increase the PaO2 to 80 mm Hg, what change to the FiO2 must be made?
31. A patient using a ventilator in the control mode with a ventilator rate of 8/min has a PaCO2 of 55 mm Hg. To decrease the PaCO2 to 40 mm Hg, what change must be made to the ventilator rate?
32. A 36-year-old woman uses a ventilator in assist/control mode with the following variables: rate, 10/min; VT, 650 mL; and FiO2, 0.40. The ABG results are as follows: pH, 7.27; PaCO2, 54 mm Hg; PaO2, 75 mm Hg; and HCO3−, 26 mEq/L. What ventilator alteration should be made?
33. A ventilator patient receiving an FiO2 of 0.70 and PEEP of 8 cm H2O has a PaO2 of 147 mm Hg. What ventilator adjustment should be made to reduce the PaO2?
34. On a volume waveform, if the tracing does not return to baseline, what does this indicate?
Branson R, Hess D, Chatburn R. Respiratory care equipment. Philadelphia: Lippincott, Williams, and Wilkins; 1999.
Cairo J, Pilbeam S. Mosby’s respiratory care equipment, ed 8. St Louis: Mosby; 2009.
Eubanks D, Bone R. Comprehensive respiratory care, ed 2. St Louis: Mosby; 1990.
MacIntyre N, Branson R. Mechanical ventilation, ed 2. Philadelphia: Saunders; 2009.
Pilbeam SP. Mechanical ventilation: physiological and clinical applications, ed 4. St Louis: Mosby; 2006.
Wilkins RL, Stoller JK, Kacmarek R. Egan’s fundamentals of respiratory care, ed 9. St Louis: Mosby; 2009.

 ) Monitoring
) Monitoring is the average pressure applied to the airway over a specific time.
is the average pressure applied to the airway over a specific time. is directly affected by
is directly affected by
 levels above 12 cm H2O result in an increased risk of barotrauma.
levels above 12 cm H2O result in an increased risk of barotrauma.

 )
)

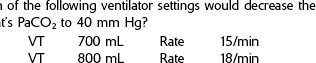
 to decrease the PaCO2 to the desired level. Then choose the answer with the appropriate
to decrease the PaCO2 to the desired level. Then choose the answer with the appropriate  that has been calculated.
that has been calculated.
 required to decrease the PaCO2 to 45 mm Hg is 8.4 L. In the example, the second choice gives a minute volume of 8.4 L (700 mL × 12/min).
required to decrease the PaCO2 to 45 mm Hg is 8.4 L. In the example, the second choice gives a minute volume of 8.4 L (700 mL × 12/min).

 .
.