19
Venous leg ulcers
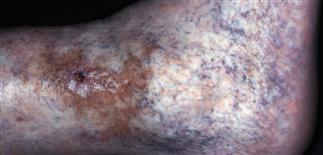
Venous stasis ulceration with surrounding atrophy blanche (white, scarred plaque surrounding the small ulcer). Some cayenne pepper-like dermatitis surrounding the ulcer, typical of venous stasis.

Medial lower leg with stasis ulceration that is clean with base of healthy granulation tissue. Note hyperpigmentation of surrounding skin and its tight appearance, indicating chronicity.

Chronic stasis dermatitis with ulceration. Medial malleolus shows a small clean ulcer, surrounding scar from prior healing, lower leg dermatitis, and some varicosities on the foot.

Stasis ulcer with small surrounding hyperpigmentation and small superficial varicosities, typical of lower leg venous stasis. Support stockings are of value.
DESCRIPTION
A chronic, non-healing ulcer typically located on medial aspect of lower leg in association with chronic venous insufficiency.
HISTORY
• Occur in middle-aged and elderly. • Ulcer formation often sudden. • Preceding leg injury, slight trauma, phlebitis, obesity, and deep vein thrombosis are also important risk factors. • Slow healing over weeks or months. • Venous leg ulcers can be a chronic, recurrent, lifelong problem. • Ulcers may be asymptomatic or mildly tender; do not typically cause severe pain.
PHYSICAL FINDINGS
• Ulcer location: most often medial malleolus. Flat, sharp, or slightly sloping borders, and shallow with granulation tissue. • Edema, usually pitting, is common; improves at night with leg elevation. • Chronic edema, trauma, infection, and inflammation lead to fibrosis; skin has firm, non-pitting, ‘woody’ quality. • Ultimately, decrease in lower leg circumference from fibrosis. • Legs swollen and ache; pain worse with standing, better in morning. • Vein varicosities often prominent. • Secondary eczematous dermatitis (stasis dermatitis) often present. • Often hyperpigmentation. • Ulcer remains small; may enlarge rapidly without trauma. • Color duplex ultrasonography identifies presence and source of significant venous reflux. • Chronic lesions are biopsied to rule out cancer (basal cell or squamous cell carcinomas), and for tissue culture. Biopsy should be performed if wound persists > 3 months. • Cultures not usually helpful. • Differential diagnosis: arterial, neuropathic, infectious, neoplastic, metabolic ulcers. Pyoderma gangrenosum, anti-phospholipid or other coagulation disorder.
TREATMENT
• Leg compression, elevation above heart level for 30 min three or four times daily and at night. • Compression with Ace wraps, graded compression stockings (30–40 mmHg), or external pneumatic compression. • Unna boots helpful; apply and replace weekly. • Use group III–V topical steroids (for 7–14 days) for stasis dermatitis. • Heavy moisturizers (e.g. Aquaphor, petrolatum, Aveeno cream) protect skin, help resolve dermatitis. • Pentoxifylline (Trental) 400 mg t.i.d. can help lipodermatosclerosis. • Debride ulcer crust and exudates. • A variety of synthetic dressings are available. • Hydrocolloid dressings (e.g. DuoDERM CGF) are effective, easy to use as initial treatment. • Change dressing type if healing is slow. • Treat exudative and draining ulcers with absorbent dressing such as calcium alginate. • Signs of malnutrition (e.g. low serum albumin level) should be noted and corrected. • Aspirin 300 mg q.d. may improve healing. • Consider ascorbic acid (1–2 g q.d.), zinc sulfate (220 mg t.i.d.), and vitamin E (200 mg b.i.d.). • Consider skin grafting for difficult cases.







