9 Venous Anomalies
Background
Overview of Echocardiographic Approach
TABLE 9-1 RECOMMENDED VIEWS TO EVALUATE PULMONARY VEIN ANATOMY
| View | Best-Viewed Pulmonary Veins |
|---|---|
| High parasternal short axis (crab view) | RLPV, LUPV, LLPVMore challenging: RUPV |
| Apical 4 chamber | RLPVMore challenging: Left lower pulmonary vein origin is adjacent to the left atrial appendage ostium |
| Apical 5 chamber / LVOT | RUPV, LLPV |
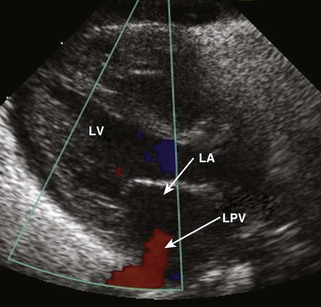
| Parasternal long axis | Left pulmonary veins (upper and lower can be difficult to distinguish) |
| Subcostal long axis | RUPV, RLPV, LUPV, LLPV |
| Subcostal short axis | RUPV |
Postoperative Evaluation of Patients with Repaired TAPVC/PAPVC
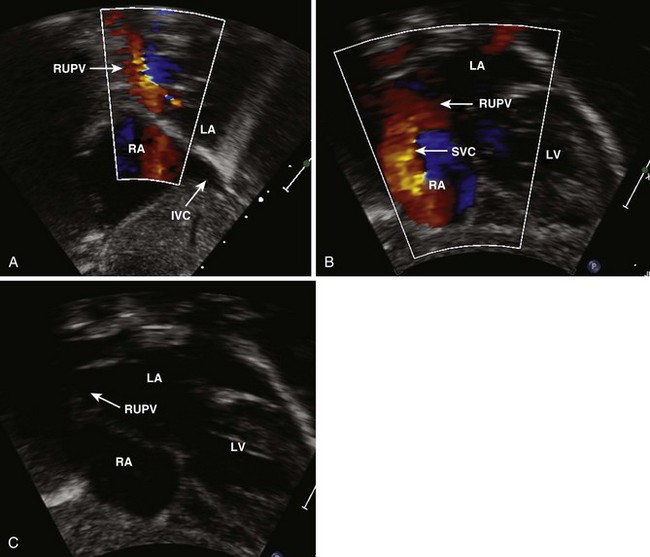
Anatomic Imaging
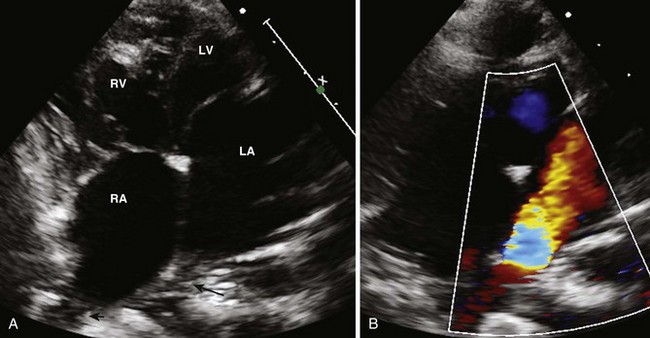
Pulmonary Veins
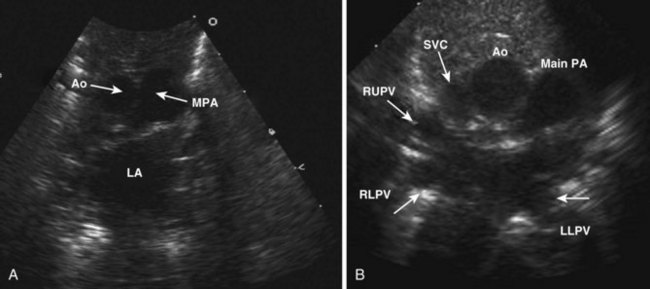
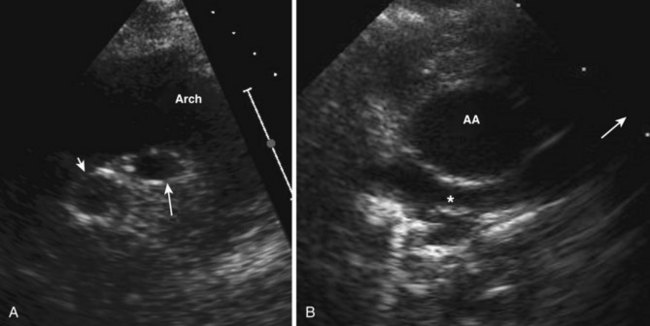
Figure 9-3 Crab view of the left atrium (LA) (A) and views of the individual venous connections (B).
Systemic Veins
TABLE 9-2 ECHOCARDIOGRAPHIC CUES FOR CONGENITAL SYSTEMIC VEIN ANOMALIES
| Anatomic Imaging Problem* | Possible Congenital Diagnosis | To Confirm, Look for |
|---|---|---|
| No inferior vena cava present in subcostal views. Only hepatic veins are seen. | Interrupted inferior vena cava with azygos vein continuation. |
. |
* Acquired venous anomalies such as deep vein thrombosis should always be considered if these anomalies are present.
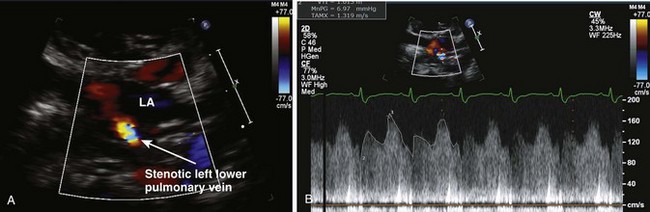
Physiologic Data
Alternate Approaches
Key Points
1 Fulton DR. Partial anomalous pulmonary venous connection. In: Basow Ds, eds. UpToDate. Waltham, MA, 2010.
More detailed review of this condition.
2 Vida VL, Padalino MA, Boccuzzo G, et al. Scimitar syndrome: a European Congenital Heart Surgeons Association (ECHSA) multicentric study. Circulation. 2010;122:1159.
3 Alsoufi B, Cai S, Van Arsdell GS, et al. Outcomes after surgical treatment of children with partial anomalous pulmonary venous connection. Ann Thorac Surg. 2007;84:2020.
4 Seale AN, Uemura H, Webber SA, et al. Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Circulation. 2010;122:2718-2726.
Perhaps the largest cohort of patients, which was gathered across 19 centers in Europe.
5 Saxena A, Fong L, Lamb R, et al. Cardiac arrhythmias after surgical correction of total anomalous pulmonary venous connection: late follow-up. Pediatr Cardiol. 1991;12:89.
6 Soriano BD. Total anomalous pulmonary venous connection. In: Basow, Ds, eds. UpToDate. Waltham, MA, 2010.
7 Tanel R, Kirshbom P, Paridon S, et al. Long-term noninvasive arrhythmia assessment after total anomalous pulmonary venous connection repair. Am Heart J. 2007;153:267.
Important series that documents that a high proportion of these patients have arrhythmias.