CHAPTER 96 Vascular Complications in Spinal Surgery
“The surgeon who says he has no complications is either a nonoperative one or a liar.”
— The Johns Hopkins Hospital Reports 19:71, 1920
Vascular complications associated with spinal surgery are increasing in frequency, due primarily to the rise in open and endoscopic anterior procedures for the thoracolumbar spine, as well as a general increase in documentation of spine surgeries in spine periodicals.1–21 This increase is from 1997-2003, reported to be more than 400% by Ikard.22 A vascular complication may be defined as an injury to a blood vessel and its sequelae, which result directly or indirectly from a surgical approach, procedure, or operative technique. Certain conditions like neuromuscular scoliosis, Ehlers Danlos, and Marfan syndrome have increased bleeding associated with their surgeries. This is also true of patients taking aspirin, nonsteroidal anti-inflammatories, clopidogrel, and many herbals and over-the-counter medications.23 For the purposes of this chapter, a vascular complication may arise directly from vascular injury or indirectly as a consequence of the injury. Mechanisms of blood vessel injury are (1) laceration, (2) traction, (3) malpositioned instrumentation, and/or (4) compression.24 The spectrum of manifestations of vascular injuries is summarized as (1) hemorrhage from a laceration of a vessel wall25; (2) vessel wall injury resulting in an aneurysm or arteriovenous fistula26; (3) blood flow consequences at the macroscopic end organ level, or ischemia on a microscopic level13; and (4) internal vessel problems such as embolization (air, plaque, or clot); and (5) thrombosis or direct injury from instrumentation like malpositioned screws or erosions from instrumentation in contact with pulsatile major arteries (Fig. 96–1).27
Vascular complications in spinal surgery carry with them potentially dire circumstances including death. As with any complication, the best treatment is prevention. Most vessel injuries are reversible; however, prompt recognition and management are essential. Prevention of vascular complications is assisted by (1) knowledge of the vascular anatomy and common variants,28,29 (2) knowledge of the blood vessel and bone relationships,30,31 (3) gentle intraoperative techniques with appropriate illumination and magnification,17 and (4) preoperative planning.17 This chapter stresses the relations of vascular anatomy to the spine and emphasizes the spectrum of spinal vascular injuries, their prevention, and early recognition. The most common vascular complication in spinal surgery is direct laceration of the vessel resulting in acute bleeding. In reality, vessels are lacerated in every spinal surgery and are an ever-present problem affecting two of the three key preventative principles of spinal surgery (hemostasis, adequate exposure with illumination and visualization). For example, in a surgery of 5641 cases, Neo reported an incidence of vertebral artery injuries to 0.14%.32 Vascular complications are underreported and true incidences are impossible to know. A further illustrative example of this “underreporting” would be a laceration of the left common iliac vein occurring during an anterior lumbar spinal exposure at L4-L5. The vascular and spinal surgeons recognize the injury and rapidly isolate and repair it. Although intraoperative blood loss is increased, there are no other sequelae. Some prominent surgeons do not consider this a “complication” but rather a routine exposure risk of the lumbosacral spine. Thus this is neither noted nor reported. Those vascular complications that can be encountered are delineated by vessel anatomic level and injury type with mechanism of injury in parenthesis in Table 96–1.
TABLE 96–1 Reported Vascular Complications in Spinal Surgery
| Cervical Spine | Thoracic Spine | Lumbar Spine |
|---|---|---|
|
Abdominal aorta (direct injury)
|
Three primary implications of vascular complications in spinal surgery exist: (1) the consequences and sequelae of brisk, prohibitive bleeding (i.e., hemorrhagic shock)33; (2) interruption of vascular supply to vital organs such as the spinal cord or brainstem34–36; or (3) secondary injury as a result of inadequate visualization caused by bleeding.17,37 These complications vary depending on the area of the spine involved and the surgical approach used.38 These are not mutually exclusive and often occur in series or combination. The former category is self-explanatory, resulting from injury to, or disruption of, major blood vessels adjacent to the vertebral bodies. In the second category, complete neurologic dysfunction or organ failure (reperfusion syndrome—see “Anterior Lumbar Vascular Complications” later) can occur. The last category is illustrated by a spinal cord or nerve root injury resulting from inadequate hemostasis and poor visualization from inadequate control of bleeding. Each of these categories has real and theoretical sequelae that may be irreversible and permanent where time is the most important singular factor. Furthermore, this chapter discusses vascular complications by anatomic area (anterior and posterior exposures), as well as other vascular-related complications such as superior gluteal artery injury during posterior iliac crest bone graft harvest and deep vein thrombosis (DVT).
Inamasu and Guiot, neurosurgeons, have further defined and classified areas of vascular risks during spinal surgery.39 Although similar to our approach, these also consider certain procedures and their anatomic location. Clearly, vascular complications are increasing in the cervical and lumbar spine due to (1) better reporting; (2) increased numbers of cases in the upper cervical spine where lateral mass C1 screws place at risk the vertebral artery and internal carotid artery and C1-C2 transarticular screws, which risk the vertebral artery; (3) marked increased posterior cervical lateral mass fixation, which now has important details to avoid injury to the vertebral artery using techniques other than that of Magerl (1.3% incident reported by Neo)32; and (4) increased procedures and techniques requiring anterior, anterolateral, or direct anterior retroperitoneal lumbar exposures that require an ever-increasing role of all anterior surgery (e.g., anterior lumbar interbody fusion, total disc arthroplasty, a plethora of procedures for discogenic pain and complex spinal deformities).
Also, the number of vascular complications has increased with the paradigm shift to total disc replacement both in the early postimplantation period, as well as in longer follow-up (Table 96–2). These approaches are using a straight rectus-splitting anterior retroperitoneal approach exposing L3 to S1. At L5-S1 the left common iliac vein is primarily at risk, and at L4-5 and L3-4 the vena cava and aorta along with their branches of the common iliac artery and vein are at risk. The recurrent or ascending iliolumbar vein is a real source of hemorrhage coming off the common iliac vein posterior or posterolaterally for L4-5 exposures. Although venous lacerations are still most common, more arterial complications, especially occlusions and thromboses, are being reported.
Potentially devastating vascular complications in these cases involving the left common iliac artery can result in rhabdomyolysis and loss of limb or life (multiple organ dysfunction, MODs, a part of a reperfusion syndrome), and a left common iliac vein can thrombose, especially if suture repair is required, significantly altering its diameter and/or flow. The single most important identifiable reason for increased vascular complications is the increased number of anterior spinal cases from the neck to the sacrum and pelvis. This has definitely been noted in multiple studies. It probably started around 1990 and did not became visible in the literature because of publication and writing delays until about 1995.22 Current efforts include safety based on evidence-based protocols.40 This is clearly the wave of the future.
Cervical Spine
Anterior Cervical Vascular Complications
Vascular complications in the cervical spine can result from improper and excessive retraction or inadvertent laceration with a scalpel or other surgical instrument.41–66 The absolute incidence of vascular injuries from anterior cervical spinal surgery is not known, but it is less common than in anterior thoracolumbar surgery, approximated at 0.5%.67 Neo and colleague’s32 review of 5641 cases placed the incidence of vertebral artery injury at 0.14%. In a review of complications of anterior spinal surgery involving more than 500 cases, Tew and Mayfield19 reported no vascular injuries. Nor did Bertalanffy and Eggert38 in their review of 450 cases. Hohf reported four cases of carotid artery injury during anterior cervical fusion, three involving laceration and the other inadvertent laceration of the carotid artery.131 No permanent neurologic sequelae occurred from these vascular injuries, but all were repaired primarily. Although Phillips emphasized that the vessels of the carotid sheath were at “some risk” from the self-retaining retractor, he reported no cases of injury in his series.69 Careful placement of self-retaining blunt blades under the longus colli muscles medially and laterally and not against the carotid sheath is the safest method in anterior cervical surgery in prevention of carotid artery injury.
Rizzoli70 reported one case of vertebral artery laceration during anterior discectomy and fusion from a pituitary rongeur laterally in the neuroforamina. Typically, bleeding in this case was controlled by packing with oxidized regenerated cellulose. No central or peripheral neurologic complications or sequelae developed. Historically, Schweighofer and colleagues71 reported a single vertebral artery injury in 175 cases of interbody fusion. The artery was sacrificed and there were no adverse consequences for the patient. Golfinos and colleagues72 reported four cases of vertebral artery injuries in 2015 anterior cervical spine cases for a case series incidence of 0.3%. Martin and colleagues73 used a Cloward technique for anterior discectomy and fusion without any major vascular injuries in 167 degenerative cases. Microvascular issues in cervical spondylotic myelopathy were a significant factor in neurologic deterioration and/or progression.17,74,75 Multiple authors have written about the microvascular aspects of spinal cord injuries, both acute and chronic.76–80 Although classically a type of vascular disorder, this topic is more comprehensively covered in the section(s) on cervical degenerative disc disease (see Chapter 36). This type of vascular injury illustrates the consequences of ischemia on an end organ system.76–81 In reality, vertebral artery injuries occur almost exclusively compared with carotid artery injuries in anterior cervical surgery.
Exposure of the anterior cervical spine commonly uses an approach medial to the sternocleidomastoid muscle and carotid sheath (Smith-Robinson approach).29 Other approaches may dissect medial to the sternocleidomastoid muscle but lateral to the carotid sheath or lateral to both.20,82–84 These approaches risk direct injury (laceration) to the external and internal jugular veins. The external and internal jugular veins are of little clinical significance, except in regard to hemorrhage, and may increase the rate of upper extremity thrombosis.85,86 However, laceration of a large vein may be of significance if the patient is positioned in an extreme reverse Trendelenburg or sitting position because of the negative pressure created, which may result in an air embolism with disastrous sequelae.87 Zeidman and Ducker88 reviewed their experience with the posterior approach to cervical radiculopathy. In their 172 cases done in the sitting position, four patients had air embolisms without clinical sequelae.88 Lacerations of the carotid sheath vessels should be repaired if possible, although the internal jugular vein may be ligated if necessary.17 Kratimenos and Crookard89 presented 15 cases of far lateral exposure instead of a transoral approach to the base of the skull and foramen magnum. No vascular complications were reported, but the exposure required identification, protection, and retraction of the horizontal portion of the vertebral artery.89
The common carotid artery is at risk as one develops the dissection plane and during retraction for the deep anterior cervical spine exposure (Smith-Robinson approach). Identification of the carotid artery by palpation and gentle finger dissection helps to minimize injury of this major vessel. Proper placement of self-retaining retractors requires medial to lateral mobilization of the longus colli muscles along the anterolateral aspect of the vertebral bodies. Blunt-tipped blades of these self-retaining retractors must be under these muscles, and only enough tension should be applied to retract these muscles away from the vertebral and disc margins aiding in visualization of the vertebra and vertebral disc. An additional preventative measure during surgery has the anesthesiologist monitor the superficial temporal artery pulse for possible carotid artery occlusion secondary to excessive retraction.17,80,90 Pollard and Little91 documented a progressive drop in carotid blood flow as a consequence of self-retaining retractors. Ipsilateral carotid artery blood flow changed from 70% to 14% on average measured by duplex ultrasonic flow as the anterior cervical discectomy and fusion proceeded in 15 cases. The diminished blood flow remained laminar at all times and rapidly returned to baseline postoperatively. Younger patients showed a greater drop in blood flow compared with older, more atherosclerotic patients. Two cases of stroke from a presumed overzealous retraction of the right carotid artery using handheld Richardson retractors, resulting in a left hemiplegia, are known to the authors. One patient improved, but the other did not. Obviously, this complication is more likely in the older patient with atherosclerotic disease, requiring extensive exposure and dissection (e.g., multiple corpectomies).92 Unquestionably, compromise of carotid artery blood flow is highly likely to cause central nervous system ischemia (i.e., stroke).92–94
The vertebral artery and vein are at risk from both anterior and posterior exposures of the cervical spine (Fig. 96–2).2 This is a unique feature of the cervical vascular anatomy. The vertebral artery is the only artery integrated with the spinal column (intraosseous) classically passing anterior to posterior at C1-C2.95 In his detailed anatomic studies, Thomas and colleagues96 have presented the incidence of vertebral artery size, variations, and anomalies (Table 96–3). In their classic surgical treatise, Smith and colleagues61 suggested that the incidence of vertebral artery injury in anterior cervical surgery is less than 0.5%. Vertebral artery injuries result in either hemorrhage, vertebral basilar insufficiency stroke, or both.61,95,97 During anterior exposure, the vertebral arteries are at risk of injury by dissection lateral to the longus colli muscles, whereas during an anterior discectomy the lateral margins of the disc past the uncinate process are at risk (Fig. 96–3).61,98 Additionally, prevention of vertebral artery injuries laterally begins with careful dissection of the longus colli muscles. The anatomic relationship of the vertebral artery in the transverse foramina has been further studied by Ebraheim.99–102 The vertebral artery is tethered to the transverse foramina starting at C6 and proceeding to C2. This occurs by a fibroligamentous mesh connected to the adventitia of the vertebral artery, the vertebral body, and the upper edge of the transverse foraminal bony extension (Fig. 96–4). This is most likely to have an impact in cervical trauma but has implications if anterior vertebral artery laceration repair is attempted, especially in mobilizing and controlling the distal and proximal ends of the artery.
Coagulation of the medial edge of the muscles and the use of a blunt periosteal elevator to mobilize the muscles laterally are recommended. The periosteal elevator should never be directed posteriorly. More likely, the vertebral artery is injured with excess lateral dissection in the intervertebral space past the uncinate processes (C3-C6), especially in case of corpectomy and tumor (see Fig. 96–3). Dissection and/or bony resection should be medial to the uncinate process sparing this medial border of the transverse foramen unless otherwise necessary (e.g., tumor). To avoid injury to the vertebral artery injury in corpectomy, most authors recommend a midline radiograph or a computed tomography (CT) scan for any abnormalities of the vertebral artery in the transverse foramina, also knowing that the longest colli muscle margin medially is the most consistent marker for the lateral extent of bony dissection.
If foraminotomy is required, it is done so with 1 mm Kerrison punch undercutting the inferior aspect of the uncinate process, where the vertebral artery is unlikely to be injured as long as only the posterior aspect was undercut. Use of the operative microscope and microinstruments within the disc space has been advocated to help decrease the risk of vertebral artery injury at the C3-C6 levels.35,103 In the 1215 case series of Golfinos and colleagues,72 four vertebral artery injuries were caused by decompression laterally in two, screw tapping, and soft tissue retraction (one). Lu and Ebraheim have studied the vertebral artery anatomy, demonstrating that it is at risk for injury lateral to the uncinate process from C3-C6 as the vertebral artery angles increase medially by 4.3 ± 2.6 degrees from caudal to cephalad (Fig. 96–5).67,99,104 The vertebral artery in essence converges medially from its origin at the C6 transverse foramina. The vertebral veins accompanying the vertebral arteries are located medially to the artery and are the first vessels “at risk.” The use of the high-speed burr lateral to the uncinate process was implicated in a majority of reviewed cases of vertebral artery injury during anterior corpectomy and foraminotomy (Fig. 96–6).54,67
Anomalies of the vertebral artery have been reported to directly compress the cervical spinal cord and nerve roots causing myelopathy and radiculopathy (see Table 96–3).54,105 The vessel was either elongated, reduced in size, or tortuous. This type of enlargement as shown by Slover and colleagues,106 gradually erodes bone, compresses the neural elements, and risks injury if discectomy or corpectomy is demanded at the anomaly level. Surgical resection and reconstruction decompression and repairing the pathologic vertebral artery were successfully employed in these uncommon cases.106 A vertebral artery injury from a C2 compression screw used to treat a type II odontoid fracture was reported by Daentzer and colleagues.107 This may occur from the guidewire, especially during insertion, or may simply be a screw that is too long (Fig. 96–7). Type II C2 fractures are increasingly treated with cannulated 3.5- or 4.0-mm partially threaded screws. Obviously, a guidewire can be as “dangerous” as the overinserted screw relative to the vertebral artery. Dickerman and colleagues108 reported a case of anterior cervical corpectomies C6 in which a postoperative stroke occurred secondary to an injury of the left vertebral artery.
The vertebral artery and cervical spine trauma has been increasingly recognized and studied (see Chapter 82). Although not directly related to our topics, this high-energy injury provides insights into the consequences and sequelae of unilateral and/or bilateral vertebral artery injuries. They are most often associated with a cervical fracture dislocation or rotatory subluxations. These subluxations occur at about 0.05% incidence including all trauma and 70% of cervical spine trauma. The treatment is often nonoperative. Benign neglect is certainly reasonable if there are no neurologic deficits, but spinal alignment and stability should be rapidly restored. Fassett and colleagues109 found a vascular injury rate with neurologic sequelae from 0% to 24%. The diagnosis is established by cervical angiography or secondarily by magnetic resonance angiography (MRA), both possibly used as a noninvasive alternative treatment; is widely variable; and is not defined by Level I and II evidence-based research. Hoit and colleagues110 studied blunt craniovertebral trauma in 69 patients. The most common injury was a basal skull fracture with neck hyperextension. The carotid artery was also monitored and quantified. Carotid artery injuries are more likely to lead to a cerebral vascular accident and are highly associated with facial fractures. Neural sequelae and/or vascular sequelae of the vertebral artery can result in a Wallenberg or lateral medullary syndrome with ischemic defects, cerebrovascular accident (CVA), and arterial hemorrhage. This is also called the “bow hunter syndrome,” referring to a stroke produced by vertebral artery occlusion.111 Of the 69 cases observed by Fassett,109 20 had vascular blunt injuries where 3 carotid and 15 vertebral arteries were involved. The pathophysiology of the carotid artery and vertebral artery injury showed intramural dissection (8 out of 28), pseudoaneurysm (6 out of 28), and occlusion (5 out of 28). Eight injuries occurred intracranially and had the worst prognosis. There were 20 in the cervical region alone. Additionally, Taneichi and colleague’s112 review of cervical spine trauma found a 7.2% rate of vertebral artery injury. In this series, the primary cause of injury was a cervical fracture dislocation from C2 to C7. Three of the 11 injuries restored flow without treatment, and occlusion was rare, but it was much more common to see intramural dissection, especially with the fracture dislocation. All of their 11 cases, one bilaterally, were asymptomatic.
Undoubtedly, blunt head and neck trauma risks the vertebral artery, especially if there is any translation or rotation of the spinal segments of C2 to C6. Vascular vessel lesions may be spasmodic, dissections, lacerations, and occlusions. However, most are prevented by rapid reduction of the cervical spine. If there is a noninvasive standard for studying the artery, the MRA is probably the best choice. Asymptomatic occlusion or other injuries are treated with observation. If the artery is occluded and symptomatic, it can be restored either through open surgery or more likely through the newer endovascular techniques for opening an occluded or damaged vessel.113 Clinical results in symptomatic patients depend on the rate at which the cervical spine can be reduced and the time of ischemia. However, endovascular repair with coated stents placed in the injured vertebral artery are superior to classical open vascular repair.
DiFabio114 performed a large inclusive series in which he reviewed 116 articles of vertebral artery injury. The most common injury was an arterial dissection followed by a basilar skull injury followed by a lateral medullary syndrome. Two percent of vertebral arteries were injured from manipulation during physical therapy. Overall morbidity was 10%. A warning or “soft” sign on physical examination is to have the patient maximally externally rotate to the right and left for 30 seconds. This is a preoperative predictive sign of spinal cord foraminal patency. If the patient does not develop symptoms, have the patient thrust the neck forward and repeat the rotation for 30 seconds. If no symptoms develop with these two maneuvers, then, in theory, the vertebral artery is patent and proximal flow is normal. A paradigm shift recently has occurred in repair of the vertebral artery from primary suture to endovascular repair. This technique used coils or covered stents and can now be inserted into the vessel to avoid complete occlusion while stopping any bleeding while occluding the vessel wall defect. This would be especially important to the left side vertebral artery, which is thought to be most frequently dominant.96
The inferior and superior thyroid arteries, between the sternocleidomastoid muscle and carotid sheath, are also at risk to injury in anterior approaches. Avoiding injury to these vessels is important not only for the sake of bleeding but also because each has a significant nerve accompanying it—the superior laryngeal nerve and recurrent laryngeal nerve, respectively. If necessary, the vessels themselves may be divided and ligated for additional exposure.35,43 Jenis and LeClair115 reported an unusual case of an inferior thyroid artery pseudoaneurysm 9 days after a routine anterior cervical discectomy and fusion. Selective endovascular embolization without revision surgery was successful in correcting this condition.115
The anterior spinal artery system is essentially an independent vascular system in the upper cervical segments and depends on contributions from radicular arteries in the middle and lower segments. The principle segmental vessel enters on the left at C6 branching from the deep cervical artery.116 The anterior spinal artery is at risk of compression in cervical spondylosis by anterior disc or osteophyte. If appropriate for the case, preservation of the posterior longitudinal ligament protects against epidural bleeding and possible injury of the anterior spinal artery. The avoidance of unipolar coagulation around the posterior longitudinal ligament or the dura is to be emphasized.38,74 Inadvertent coagulation or disruption of the anterior spinal artery will likely result in quadriplegia or quadriparesis from ischemia of the anterior and lateral cervical spinal cord.79,117,118 Regarding complications related to microvascular disease, myeloradiculopathy can cause dysfunction in the esophagus even before surgery.
Iatrogenic arteriovenous fistula between the vertebral artery and the surrounding venous plexus is a rare complication of anterior cervical discectomy.119 It may complicate anterior cervical discectomy at or above the C5-C6 level because the vertebral artery runs immediately lateral to the disc space beginning at this level. The presence of a cervical bruit following surgery may suggest a fistulous communication and necessitates angiographic investigation. Minimally invasive endovascular occlusion of the fistula with contemporary interventional techniques is the therapeutic procedure of choice.38 Cosgrove and Théron119 reported a patient who presented with an audible bruit 2 months after successful anterior cervical discectomy and fusion. Revision surgery was not necessary. The author is aware of two unreported cases of vertebral artery injury during anterior cervical disc surgery. Both resulted in no permanent injury, although one case had a pseudoaneurysm detected by postoperative magnetic resonance imaging (MRI) and MRA and ultimately was treated with microscopic reconstruction of the vertebral artery.17
Treatment of the vascular injuries during anterior cervical spine exposure involves recognition, control of bleeding, and repair, ligation, or endovascular stents when indicated. Although primary repair of the vertebral artery and common carotid artery is desirable, endovascular techniques are becoming the standard of care. If the vertebral artery is lacerated during the anterior dissection, the bleeding point must be tamponaded and the dissection carried laterally by mobilizing or dividing the longus colli muscles. The costotransverse lamellae and fibroligamentous attachments can be removed with a high-speed, diamond burr or Kerrison rongeurs to allow adequate exposure for primary vascular repair (Fig. 96–8A).120 If primary repair is chosen, the artery should first be exposed proximal to the laceration and then the loops should be used for occlusion (Fig. 96–8B).120 The nerve roots should be identified and protected. Once the artery is exposed and controlled, the laceration can be repaired, if possible, with 7-0 polypropylene interrupted sutures (Fig. 96–8C).120 The repair will require the assistance of an experienced vascular surgeon, and spinal stability should be assured after this additional required exposure. If temporary, cross clamping of the injured vertebral artery required in the repair in effect mimics a ligation and vertebrobasilar ischemia or infarct still may occur. Repair of vertebral artery injury is supported by studies by Golfinos, Pfeifer, and colleagues.72,93,120 Others have ligated the lacerated vertebral artery during an anterior approach to the cervical spine.2,38,95,104,121 This presumed a planned resection, which is rarely a realistic fact. If the vertebral artery has to be sacrificed, ideally but not practically it should first be studied by intraoperative angiography to ensure that the anatomy of the patient’s vertebral system is likely to permit such a maneuver.82,95,104 The ability of the patient to tolerate unilateral occlusion of the vertebral artery with sequelae is supported by a study of nine patients with traumatic occlusion of the vertebral artery. Only two developed neurologic deficits, both of which were transient.122 The presence or absence of neurologic deficit depends in part on the collateralization of the vertebral artery of the circle of Willis and the status of the opposite vertebral and basilar arteries (see Table 96–3).2,38,43 However, Smith and colleagues61 reported three out of seven cases of vertebral artery ligation developed symptomatic vertebrobasilar ischemic signs and symptoms. These symptoms include syncope, drop attacks, dizziness, nystagmus, and the Wallenberg syndrome. Smith and colleagues61 recommended primary repair if it could be accomplished, but repairs were not done in their retrospective series. These experienced surgeons could only (1) tamponade (30%); expose and electrocoagulate (10%); ligate transosseously (20%); or (2) open hemostatically clip (10%) in their reported 10 cases (Fig. 96–9). Further controversy as to whether to ligate or repair a vertebral artery laceration or tear is found in the cervical spine trauma literature. Thomas and colleagues96 presented a classic anatomic study that occlusion of the vertebral artery related to the incidence of brainstem ischemia or infarct was 3.1% with left-sided occlusion compared with 1.8% with right-sided disruption of flow (see Table 96–3). Conventional arteriography and, more recently, MRA demonstrate frequent vertebral artery flow abnormalities in injuries such as unilateral and bilateral facet fracture dislocations.49,77,78,123–125 In most cases, thrombosis occurs with or without recanalization.122 Despite being common sequelae, the injuries rarely cause serious irreversible vertebrobasilar ischemia or infarction of the brainstem and cerebellum.44 Reid and colleagues126 found 43 cases of vertebral artery injury from head and neck trauma. There were no cases of vertebral basilar insufficiency or stroke. However, there was a 4.7% morbidity due to hemorrhage. The minimally invasive endovascular repair is becoming the procedure of choice in symptomatic or hemorrhagic vertebral artery (see also Chapter 82).
A specific vascular complication resulting from local hemorrhage with potentially lethal consequences is a wound hematoma.127,128 This cannot be prevented by intraoperative drain placement.129 Wound hematomas in the neck represent a spectrum of clinical presentations from small local swellings to deeper collection compressing the trachea or spinal cord. These can present within hours to days following anterior cervical surgery. In cases with rapid deterioration and/or an expanding hematoma, immediate decompression of the neural elements or airway may be required to open the wound as expediently and sterilely as possible. Further discussion is given later in “Subdural and Epidural Hematoma.”
Vascular complications of cervical total disc arthroplasty are similar to those discussed for anterior cervical discectomy and fusion (see Chapter 43). Vascular complications are rarely associated with extensive discectomy because the uncinate processes are preserved. Suffice it to say, as long as disc preparation before implantation does not violate the uncovertebral joint, injury to the vertebral artery will remain rare. All of these potential vascular complications apply for the Smith-Robinson exposure. Intuitively, it is unlikely that a constrained total disc arthroplasty in the neck will fail by extrusion but more likely by bone fracture settling or polyethylene wear.130
Posterior Cervical Vascular Complications
The vertebral artery and venous plexus are the only major vessels that course posterior to the lamina in the spinal column (Fig. 96–10). These vessels are at risk of injury in the upper cervical spine or during posterior fossa surgery.35,95 Fortunately, the incidence of posterior vertebral artery injury is rare. Rizzoli70 reported three cases of posterior vertebral artery injury, all of which were secondary to laceration from the bovie device; two were ligated without neurologic deficits, and the other was repaired primarily. Hohf131 reported one case of posterior vertebral artery injury during posterior cervical spinal surgery, but the details of the injury were not given. The author is aware of two cases of posterior vertebral artery injury during exposure of C1 for an occipital cervical fusion. Both of these cases resulted in a liter of blood loss from vigorous subperiosteal dissection with a periosteal elevator. Both were managed by packing to control bleeding with absorbable gelatin sponge or oxidized regenerated cellulose. Fortunately, no neurologic sequelae developed in either case.17 Cranial base surgery continues to offer significant challenges and limitations owing to the variations of this region’s cerebrovascular anatomy and physiology (see Table 96–3).132
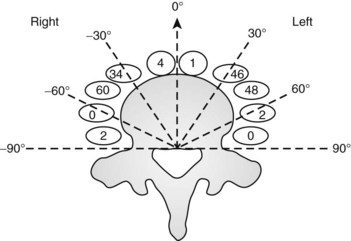
Prevention of vertebral vascular injuries during posterior exposure of the upper cervical spine starts with identifying the posterior tubercle of the atlas and limiting lateral dissection to less than 1 cm (8 to 12 mm) along the cephalad edge of C1 and less than 1.5 cm (12 to 23 mm) along the caudal C1 border (Fig. 96–11).17,95,104 These limits may need to be adjusted to take into account smaller individuals or pediatric patients. The vertebral artery is vulnerable because it passes between the C1 and C2 transverse foramina laterally. Here, lateral dissection along the caudal border of C1 should stop when one encounters the dorsal ramus of C2. Injury to the vertebral vessel should be controlled initially by packing and administering local antithrombotic agents. If possible and technically feasible, a posterior vertebral artery injury should be repaired for similar reason for repair in the transverse foramina (i.e., to preserve brainstem and cerebellar blood flow).132
Similar to anterior lumbar surgeries, instrumentation of the upper posterior cervical spine has seen an exponential increase. Consequently, operating from the occiput to C2 increases the risk of injury to the vertebral artery, carotid artery (CA), and hypoglossal or cranial nerve XI depending on the technique. Malpositioning of the lateral mass screws may injure the vertebral artery within the transverse foramen (Fig. 96–12).2,20,102,133 As this technology is becoming established as a standard of care, complication rates of C1-C2 transarticular screws and C1 lateral mass and C2 pars screws are increasingly reported (see Fig. 96–12). C1-C2 transarticular screws risk the vertebral artery, carotid artery, and hypoglossal (CNX11th) nerve anteriorly in the C2 transverse foramina, making preoperative CT scanning mandatory to prevent inadvertent injury as screw insertion progresses across the C1-C2 facet (Fig. 96–13).97,134 Anomalies and anatomic variations are common (10%) among all cases in the geometry of the foramen, as well as its position with the vertebral artery in the C1 vertebral body (CV6). C1 lateral mass screws risk the vertebral artery posteriorly and laterally, requiring meticulous technique for mobilization and protection.18,135 Prevention includes knowledge of the bony landmarks, choosing appropriate screw lengths, and reviewing angles of insertion (Fig. 96–14). Wellman and colleagues,138 in a consecutive series of 43 patients, reported no vertebral artery injuries from lateral mass plating using AME Hard Universal instrumentation (UBP; American Medical Electronics, Richardson, Texas). It is noteworthy that the females average a 14- × 3.5-mm screw compared with a 16- × 3.5-size for males.83 The vertebral artery and veins are directly anterior or slightly lateral (about 6 degrees at C6) at the middle one third of the lateral mass. A lateral mass screw insertion technique, starting near the center of the mass and directed about 10 to 15 degrees lateral and 30 to 35 degrees cephalad, is best to avoid the vertebral artery.
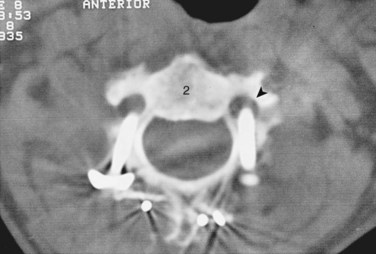
FIGURE 96–12 Malpositioned C2 screw violating the vertebral artery, fortunately without ill effects or vascular sequelae.
The Magerl technique, which goes more or less straight down from a central lateral mass, is more likely to impale a nerve or the vertebral artery. Thus this technique should be avoided. Cervical pedicle screws may be placed more safely at C6 or C7 in reference to the vertebral artery. The screws are started about 2 to 3 mm inferior to the superior articular facet and just lateral to the midline of the lateral mass angling medially 35 degrees (C6) and 30 degrees (C7). These projections pass anterior to the vertebral artery at C6 (see Fig. 96–14). The C1-C2 technique, which is least likely to risk injury to the anterior VA, is the modified technique of C1 lateral mass screws and C2 intralaminar crossed screw fixation described by Harms and others.136 In about 15.5% of patients, a false bony bridge called the ponticulus ponticus covers the vertebral artery as it passes onto the posterior C1 ring. This is easily noted on lateral cervical plain films (Fig. 96–15). Young and colleagues137 emphasized the importance of recognizing this common anomaly to avoid injury to the VA by dissection or if C1 transosseous screw fixation is considered.
Placement of anterior C2 screws is routinely used to stabilize type II or high type III odontoid fractures. Remember that C1 and C2 injuries anteriorly or posteriorly should be reduced before attempting fixation or there will be a much higher risk of injury to the cord or vertebral or interior carotid artery. Vascular risks are derived from either the guidewire or screw tip, which may impale the internal carotid artery or the vertebral artery (Fig. 96–16). To avoid this, radiologic control is used to minimize penetration of the tip of the odontoid at initial positioning, whether you use one or two screws and guidewires. C2 anterior screw placement should be done with live fluoroscopy by hand and without power reaming and tapping. Once positioned, make sure the reamer or screw cannula is free of bone so that inadvertent advancement of the guidewire does not occur. This procedure increases fluoroscopy time, but it is essential to carefully monitor the tapping position, as well as the insertion over the guidewire, to make sure that proximal migration does not occur. Some surgeons employ three-dimensional (3D) fluoroscopy or CT image guidance in such cases to minimize radiation while maintaining safety by imaging guidance (see Fig. 96–7).
Vertebral artery injury posteriorly is often injured by lateral mass screws either from the drill, screw, or probe penetration. All the techniques that start near or just inferior to the midline and angle laterally and cephalad 15 to 30 degrees and use screws that are 14 to 16 mm are unlikely to injure the vein (vertebral artery or veins).102,138 As with anterior C2 screw placement, drilling should be done by hand and not power. Also, caution should be used with the depth gauge taking care not to plunge and possibly grab the vertebral artery with the curved end of the depth gauge. Neo and colleagues32 clearly identified the Magerl technique as most likely to injure the vertebral artery in the lateral mass technique with an incidence of 1.4% in his survey series of 5,641 cases. The relationship of the vertebral artery to C1-C2 and its location to the triangular window of the pedicle of C1 is emphasized by Ebraheim and colleagues99,100–102 (Figs. 96-16 to 96-18; see Fig. 96–11A). Primary clinical challenges are to identify the C2 root, identify the vertebral artery, and identify and control the venous plexus, which sometimes covers and projects inferiorly between the vertebral artery and the posterior C2 dorsal ramus.
C1 fixation was complicated in one series by high-riding vertebral artery, thinning, or abnormality of the C2 pedicle, where anomalies of the artery are common in the vertebral artery (see Figs. 96-11A and 96-17). Typically 8 mm from the C1 tubercle, the vertebral artery penetrates the ligamentum flavum passing over the cephalad margin of the C1, posterior ring. The level of the C1 lateral mass screw insertion at the inferior border of the C1 arch is typically 12 to 14 mm from the midline. The ponticulus ponticus is a harbinger for injury to the vertebral artery along the cephalad margin, especially for C1 lateral mass screws, if unrecognized (see Fig. 96–15).
C1 lateral mass fixation has proven safe, stable, and effective on the basis of the window of the lateral mass with the C1 arch and the vertebral artery superior and the C2 dorsal root ganglion inferior. This “window” is covered by a plexus of veins (differentiated from vertebral artery), which needs to be coagulated and controlled. Removal of the inferior edge of the C1 arch often assists the placement of the C1 lateral mass or pedicle screw. The medial-most extension of the vertebral artery cephalad to the C1 ring is usually about 8 mm from the C1 tubercle but about 4 more mm lateral and caudal to the C1 ring, which is the optimal starting point for a C1 lateral mass screw. Image guidance systems like 30 fluoroscopic or CT-based guidance systems are becoming vital and increase safety in this point of the C1 lateral mass screw positioning.139 The vertebral artery anomalies are high in relation to the vertebral artery to transverse foramina and bone and to the anastomosis at the bone and skull. Thomas and colleagues96 found an absence of the vertebral artery on the right in 3.1% and 1.8% on the left. They reported several cases of narrowing of the vertebral artery (5.7% on the left and 9.7% on the right). Additionally, the left vertebral artery is most often dominant. Also, Thomas and colleagues96 found two cases of vertebral artery proceeding directly to the posterior internal cerebellar artery, one on the right and one on the left. These anomalies can and do affect C1 lateral mass screw fixation along with the ponticulus ponticus (see Fig. 96–15). A preoperative CT with reconstruct is mandatory, as is the upper cervical case, where screws are placed so as to identify the vertebral artery and its foramen. Numerous minor and major variation occur, some of which preclude screw placement on one side. If injury of a vertebral artery occurs, it is treated by reinsertion of the screw or in some cases packing the hole with collagen cellulose strips and covering the hole with sterile bone wax.
Thoracic Spine
Anterior Thoracic Vascular Complications
Anterior exposure to the thoracic spine is well established with ever-increasing applications.4,17,45,88,140–161 Thoracoscopy is now routine for the treatment of a variety of disorders, primarily scoliosis release, fusion, or instrumentation. Oskouian and Johnson11 retrospectively reported a 5.8% incidence of vascular complications in 207 open anterior thoracolumbar surgeries with mortality rate of 1%. They reported a 3.4% incidence of direct vascular injuries of the segmental or intercostal vessels. Most had a delayed onset of sequelae, and one death occurred as a result. Potential vascular-related complications involve injury to the major vessels and their branches and the consequences of the interruption of the blood supply to the thoracic spinal cord (Fig. 96–19). The incidence of paraplegia secondary to unilateral vascular interruption of the thoracic segmental vessels is essentially nil, in primary or unoperated cases. Bilateral disruption of the segmental blood supply, as in aortic surgery or dissecting aortic aneurysms, is not as forgiving.21,81,162–168 The thoracic and vascular literature is replete with reports of the difficulties with bilateral disruption of the blood flow to the thoracic cord during complex thoracic and thoracolumbar aneurysm reconstructive surgery. Recently, the risk of paraplegia and paraparesis in cardiothoracic surgeon has been reduced by (1) limiting cross clamping times,21,162 (2) avoiding hypotension (i.e., mean arterial blood pressure [MABP] < 60 mm Hg),21,162 (3) cerebrospinal fluid (CSF) drainage,163,165 and (4) distal aortic perfusion by cardiopulmonary bypass.21,163 CSF drainage or cooling is proven to decompress the intradural space and improve blood flow to the cord via the artery of Adamkiewicz and other segmentals.163,165 Parke and colleagues12 have shown that smooth muscle of the tunica media of the lower anterior spinal artery may further risk blood flow to the cord if constricted by autoregulation after aortic cross clamping. Other procedures associated with spinal cord infarction include bilateral sympathectomies16; open thoracoscopy with lobectomy169; open anterior surgery for tuberculosis in which bilateral vascular ligation or disruption occurs166; revision anterior scoliosis surgery, especially if approaching the previously undissected side (i.e., right side) of the anterolateral spine or having a significant kyphotic component167,170; and rarely a routine spinal test today, angiography, and MRA using the thoracic or abdominal aorta.44,72,164 Theoretically, the thoracolumbar spinal cord tolerates transient and permanent unilateral segmental blood flow disruption. However, bilateral segmental disruption, transient or permanent, is much more likely to cause spinal cord ischemia and thus paraparesis or paraplegia.
The exact incidence of spinal cord infarction and paraplegia due to vascular occlusion is not known. Morbidity and mortality statistics from the Scoliosis Research Society (1975) described an incidence of 1% paraplegia due to indirect vascular compromise (distraction instrumentation) in more than 10,000 deformity cases.95,171,172 Paraplegia rates are higher in adult patients and those treated with posterior instrumentation and fusion for severe scoliosis, kyphosis, kyphoscoliosis, or congenital scoliosis and kyphosis.173,174 Open, single-stage, same-day vascular disruptions leading to paraplegia have been reported in 6% of one-stage circumferential spinal osteotomies.36 Of the five reported cases, four were permanent and one recovered completely. In this series of circumferential osteotomies, there were 55 adults with scoliosis and all cases resulting in paraplegia were at the T5-T9 level. Hodgson reported one case of vascular-induced paraplegia in more than 400 cases of anterior spinal surgery for tuberculosis.166 Riseborough,148 Micheli and Hall,174 Dwyer and Schafer,142 and Winter and colleagues151 reported a cumulative total of more than 3000 extensive open anterior discectomies or partial corpectomies with unilateral ligation of thoracic segmental arteries without any cases of paraplegia. It is important to understand that unilateral ligation of thoracolumbar segmental arteries applies to primary cases and occurs over the convexity of the deformity. Certain complex revision surgeries, however, may mimic bilateral ligation.151 Cases in which there is significant kyphosis or kyphoscoliosis, especially with multiple posterior procedures or prior surgery, may have paraplegia with unilateral ligation of “key” segmental arteries. Winter and colleagues151 discuss a so-called “cord at risk” advocating spinal cord monitoring up to 20 minutes after ligation or clamping of a key segmental (Artery of Adamkiewicz). These authors describe a case of revision anterior scoliosis surgery in which the convexity was approached after prior anterior surgery from the concavity.151 The authors clamped a segmental and observed loss of somatosensory evoked potentials (SSEPs). The spinal cord monitoring changes were reversible and mandated that the anterior discectomy be performed between the segmental vessel, thereby sparing spinal cord blood flow. This circumstance illustrates that bilateral thoracolumbar segmental vessels are associated with a small but definite risk of spinal cord infarction and permanent neurologic deficits. Avoiding actual or indirect bilateral segmental vessel injuries should be avoided from T9-L2 on the left.
The transthoracic approach to the anterior thoracic spine usually requires mobilization of segmental arteries and veins over several vertebral levels.98,142,148,151,174,175 A right-sided approach is recommended to avoid the pericardial structures and theoretically avoid the artery of Adamkiewicz. Spinal cord monitoring is now considered routine, especially motor evoked potentials (MEPs). MEPs are the most precise method to monitor the spinal cord (anterior spinal cord) compared with SSEPs, which test primarily the dorsal columns of the spinal cord.176 In cases of deformity, however, it is most advantageous to approach the convexity of the deformity, regardless of the side involved. To gain access to the thoracic segmental and intercostal arteries, the parietal pleura must be divided.177 This dissection begins over the disc space, where there are no vessels. The individual vessels are identified and isolated with a right-angle hemostat and ligated; occlude with vascular clamps, or spared.178 About 1 centimeter of segmental vessel is maintained from the thoracic aorta or vena cava to avoid cutting this vessel too close to the aorta or vena cava, thereby creating a hole in the side of the vessel. Lazorthes and colleagues179 have shown that better collateralization and anastomotic substitution can occur as these vessels are ligated or disrupted closer to the major vessels. Inadvertent laceration or avulsion of the segmental vessels from the aorta or cava can result in rapid voluminous bleeding.17 Should this occur, bleeding should be controlled by direct pressure proximal and distal to the defect. Repair of the aorta or vena cava should be assisted by a surgeon experienced in vascular surgery. Mack and colleagues143,149,180,181 reported 100 cases of video-assisted thoracoscopy (VAT) for a variety of thoracic spine conditions. A recent European meta-analysis found no vascular complications or paralyses associated with VAT.182 A singular case of profound epidural bleeding occurred, but no incident of segmental artery, aorta, or azygos vein injury was noted.104 Other studies of thoracoscopy have validated the usefulness and safety, especially relative to the vascular structures.68,146,149,183,184
Faro and colleagues in a thoracic spine calf model monitored thoracic vertebral body screws after placement in relation to the aorta at T6 to T11. This was an anterior thoracic instrumentation model. There were a number of penetrations of the vertebrae into the aorta. These penetrations at T6 to T11 were followed at 3, 6, and 12 months. Postmortem histology showed thinning of the aorta in 52%. Sixty percent had scarring with impregnation with a trend of greater impregnation causing larger amounts of scarring. In 96% of all the cases in which there was some screw contact, the aorta showed some cicatrix. The authors concluded that this histopathology was worrisome for late development of complications if the screw tip approached or entered the thoracic aorta in calves.185
The relative importance of individual blood vessels that supply the spinal cord is debated.94 In 1939 Suh and Alexander noted that “much of what has been written in the past 40 years about the circulation of the spinal cord is either inaccurate or incomplete.”81 In the same year, Bolton determined that the segmental vessels that supply the spinal cord are indeed end arteries and there are no anastomoses between the capillary beds.43 Individually, vessels that travel with the spinal nerve into the spinal canal do not seem to be important, as evidenced by Dwyer’s ligation of 3 to 16 ipsilateral segmental arteries in a single patient without neurologic loss.142 Great attention was given in the past to the artery of Adamkiewicz (arterial radiculitis or arterial magna),which is the largest of the feeders to the thoracolumbar spinal cord (Fig. 96–20).48,123,186,187 It occurs on the left side in 80% of patients between T7 and L4 with the greatest incidence (92%) between T8 and L1.80,117,187,188 It usually enters the spinal canal with at least one additional feeder. The location of the artery of Adamkiewicz has further been confirmed on the left from T8-L1 by helical CT scans and MRA, as well as more contemporary spinal cord angiographic techniques.167,187 In 1970 DiChiro and colleagues123 noted that this artery could be tied in Rhesus monkeys without complications, but paraplegia would follow when the anterior spinal artery (arterial median longitudinal artery) was simultaneously ligated. Further evidence of the importance of bilateral disruption of this segmental vessel is indicated by the high incidence of paraplegia in thoracic aortic surgery involving cross clamping of the thoracic aorta or in cases where dissecting aneurysms occlude the segmental vessels bilaterally.21,81,162,164–167,189,190 However, paraparesis or paraplegia as a result of unilateral ligation of thoracic, thoracolumbar, or lumbar segmental vessel (left or right) is rare.155 Bridwell and colleagues173 reported two cases in which there was unilateral ligation from T10 to T2 on the left, but these cases were complicated. One was a 34-year-old patient who had had kyphotic corrective surgery 6 years ago with an anterior and posterior treatment for kyphoscoliosis. Subsequently, he underwent another two-stage posterior repair of nonunion followed by an anterior left-sided T10 to T5 ligation of vessels with spinal cord monitoring a week later. During the second-stage surgery, the MEPs disappeared and the patient had a permanent anterior cord syndrome postoperatively. The other case was an 85-year-old male who had four prior lumbar decompressions and fusions, and 3 years before his presentation he had an L1 to L2 fusion. His diagnosis was flat back syndrome, and thus he underwent a posterior pedicle subtraction osteotomy at L1. Four months afterwards, he returned and underwent a revision anterior T10 to L2 left-sided fusion. On the second postoperative day he became a paraplegic. This delayed-onset paraplegia was attributed to slow occlusion of the artery of Adamkiewicz.155 Dr. Winter has always recommended that to avoid injury to the artery of Adamkiewicz to ligate the vessel unilaterally, it should be done in the midbody position and on the convexity of the curve. He also recommends, along with Leung, intraoperative monitoring, especially MEP or a Stagnora wake-up test if no monitoring is available or the spinal cord monitoring is felt to be inconsistent.191
Even the artery of Adamkiewicz, which is substantially larger than the others, can be occluded under most circumstances. It is not uncommon in some scoliosis procedures such as anterior instrumentation to have an extensive ipsilateral sacrifice of these feeding arteries without significant sequelae.142 Winter and colleagues151,191 reported more than 1200 consecutive anterior spinal cases with no cases of paraparesis or paraplegia related to the ligation of segmental vessels unilaterally. These authors recommend (1) vessel ligation unilaterally, (2) ligation on the convexity of the deformity, (3) ligation at the mid body level, and (4) avoidance of hypotensive anesthesia. The later point needs emphasis in that the spinal cord is best protected by MAP of 70 mm Hg or more. This may also have implications to visual loss in the prone position due to posterior ischemic optic neuropathy (PION) if this means blood pressure is not maintained. Kostuik reported no vascular or neurologic complication due to vascular injury in 278 cases involving unilateral segmental ligation anterior kyphotic deformity reconstructive surgeries with anterior Kostuik-Harrington instrumentation.192
Dommisse and Enslin noted four cases of permanent paraplegia in their series of 68 circumferential spinal osteotomy procedures, three of which occurred between T5 and T9 and the other occurred with surgery below T10.36 These authors confirmed the “critical vascular zone of the spinal cord” from T4 to T9. In the study by Lozorthes, the artery of Adamkiewicz appeared between T9 and T12 in 75% of cases, at the L1-2 level in 10% of cases, and at the T5 to T8 level in 15% of cases.179 When the artery of Adamkiewicz appeared in the midthoracic level, there was a supplemental artery he referred to as “the arteria conus medullaris supplying the thoracolumbar cord” (see Figs. 96-19 and 96-20). The thoracolumbar spinal cord has a rich anastomotic blood supply formed by both the anterior and posterior spinal arteries. The anterior spinal artery in the region of T4 to T9, however, is quite small and can be incomplete, as demonstrated by Lazorthes.179 Dommisse’s studies eloquently demonstrated that the spinal canal was also the most narrow in the T4 -T9 region, and this could predispose to surgical complications, particularly in the face of a chronic low-reserve state of spinal fluid circulation.35
Hempfing and colleagues did an elaborate study on the unilateral and bilateral aspects of paraplegia using a high-powered laser Doppler source with a Doppler flow meter placed in the vertebral body. This researcher ligated the segmental vessels on the left side and then measured the change in the vertebral body flow.193 The problem is the vertebral body flow may or may not correlate with the segmental vessel flow, and it is at best an indirect measurement. Ten cases were done intraoperatively. They ligated segmented vessels on one side as part of the spinal procedure and then occluded or tamponaded the others from T7 to L3. They had a small decrease in blood flow of about 13% with ligation, but there was a 75% loss of blood flow with bilateral blood flow disruption by the compression on the opposite side. Curiously, in the four levels they noted there was no change that they attributed to a significant collateral circulation. These were at T8, T10, T11, and L3. However, all occlusions returned to baseline almost immediately after the patency of the vessels was restored.
Cambria and colleagues194 looked at the aorta relative to the artery of Adamkiewicz and found that 80% of the time it was T9 to T12 and 100% of the time it was T8 to L2. The key, in regard to aortic surgery, is to not cross clamp the aorta more than 30 minutes, reattach key intercostals, and cool the CSF. A great deal of debate as to how best to prevent paraplegia has occurred. The cardiovascular literature suggests that these are several keys: (1) have a short cross clamping time and (2) identify the artery of Adamkiewicz preoperatively. The artery of Adamkiewicz can be identified by spinal angiography or MRA, which can guide the reattachment of those key segments, especially to the left.
In their study, Alpagut and colleagues195 reminded the spinal surgeon that 12% of the artery of Adamkiewicz is at L1-L2. Although a known potential location of the artery of Adamkiewicz, the issue of ligation on the left is reemphasized, especially if there has been prior surgery or some injury on the opposite side. Oskouian reinforced that intercostals can at times be inadvertently avulsed or stretched, which may cause problems with the key left segmental or intercostal vessels (i.e., artery of Adamkiewicz).11 One author identified 30 cases of traumatic chest compression in which 1 involved the artery of Adamkiewicz without paralysis or paraparesis.196
Kato and colleagues studied dogs by ligating the segmental vessels bilaterally. When he ligated them from L3 to L6, paraplegia developed 100% of the time. When he ligated them from L4 to L6 bilaterally, he would get some with paraplegia and some with paraparesis. He equated the dog levels of T9 to L2 to be equivalent to our T4 to T9 or watershed area, and the lower area would have been the area of the “artery of Adamkiewicz.”197 This type of study re-emphasizes the need for bilateral segmental or intercostals disruption to result in paraplegia.
Most acute major vascular injuries during anterior thoracic or thoracolumbar surgery are direct injuries with immediate and profound blood loss that demands immediate attention. If the case is minimally invasive, an open procedure will be necessary. Delayed injury such as that of a segmental or intercostal vessel (artery or vein) may result in a hemothorax.54 In Zeilke’s series of 103 anterior thoracolumbar procedures, he reported 4 hemothoraxes requiring chest tube placement.54 Following the theme of delayed vascular complications, Ohnishi and colleagues198 reported a delayed aortic rupture due to erosion of the aorta from a T12-L1 smooth rod Kaneda anterior implant (AcroMed; Raynham, Mass.). This occurred 20 months following a T11 burst fracture and repair in a middle-aged man presenting with nonspecific gastrointestinal symptoms. Anterior instrumentation or thoracic scoliosis also risk major vessel injury because these vessels closely approximate in the concavity of the curve of the spine to the screw tips.150 This bleeding complication is due to excess length or depth gauging of the vertebral body hole. Vanichkachorn and colleagues198a reported a potential vascular injury from broken pedicle screw migration on attempt to remove the screw with a trephine extractor system at T12. Anterior exposure was necessary, and the screw at T12 had pushed out from the vertebra and become seated between the aorta and vena cava. The authors are aware of one another’s case in which a thoracic pedicle screw was inserted to 40 mm (4.5-mm diameter) and lacerated a T10 segmental vessel resulting in hypotensive, hemothorax, and death. As pedicle fixation indications expand in the thoracic spine, the position of the screws relative to the canal and anterior vascular structure must be carefully considered.199 The safety of pedicle screw placement, especially in the cervicothoracic spine, may be enhanced by multiplanar plain images or CT-based image guidance systems.139 Been and colleagues200 also noted a 20-year-old patient who had undergone a transpedicular instrumented thoracolumbar fusion for scoliosis and developed a saccular aneurysm with dissection of the thoracic aorta. Recognition and repair of this unusual aneurysm required successful endovascular grafting through a transfemoral approach.200
Posterior Thoracic Vascular Complications
Direct posterior midline thoracic surgery typically endangers no major vessels.173,201 However, if the anatomy is distorted such as in idiopathic right thoracic scoliosis, the intercostals can be injured either with rib resection (posterior convex thoracoplasty) or overly vigorous posterolateral exposure. The author is aware of one case of hemothorax from the inadvertent injury of an intercostal vessel at T7 on the convexity of the deformity. This rigid deformity measured 50 degrees, and the bleeding was due to the periosteal exposure lacerating the vessel with retraction. A right hemothorax developed over the next day with clinical dyspnea and hypoxia. Thoracoscopy to coagulate and ligate the vessel, as well as drain the right chest cavity, was required.17 Deviation too anterior even in the routine midline posterior cervical or thoracolumbar exposures can potentially injure segmental vessel(s) anterior to the transverse processes, which may or may not be associated with deformity.
Posterolateral Thoracic Vascular Complications
In contrast, the posterolateral approach (also known as costotransversectomy or lateral rachitomy of Menard) has definite potential vascular complications, although major vascular injury is quite rare.202 This approach requires mobilization of the neurovascular structures that serve as a guide to the spinal canal. Injury to the intercostal vessels can result in profuse bleeding; however, these vessels can be ligated without problems. Retrograde thrombosis of the left eleventh intercostal vessels from a left rib transthoracoabdominal approach during sympathectomy has been reported to cause paraplegia in one case.16 In this regard; a right-sided approach is used, unless the pathologic process dictates a preference to a side. The author is aware of a case in the early postoperative period presenting with a hemothorax from uncontrolled intercostal artery bleeding during a costotransversectomy. Chan has warned of potential aortic perforation during a costotransversectomy for tuberculosis owing to the weakening of the vessel from the tuberculous inflammatory process, which is also true of any chronic infection or tumor.46 Injury to the major vessels using the costotransversectomy approach requires packing off the bleeder in the depths of the wound, covering the wound, starting volume expanders, and preparing for immediate thoracotomy and repair of the thoracic vessels because retraction is likely to occur.177 Microembolism or endovascular repair techniques may be useful depending on the magnitude and location of the injury. Prevention of injury to the major vessels anteriorly during the costotransversectomy procedure is assisted by careful blunt dissection of the pleura off the lateral border of the vertebral bodies.201 No instrument should be placed in the depths of the wound unless visual identification of the position and tip of the instrument can be verified. Once the parietal pleura has been mobilized, the segmentals can be further bluntly dissected from the vertebral body or ligated, thereby allowing access to the disc and posterolateral vertebral body.177
Lumbar Spine
Anterior Lumbar Vascular Complications
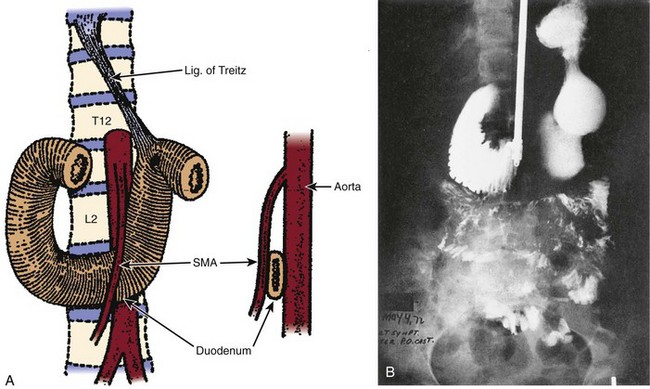
Inamasu and Guiot39 have documented a definite increase in vascular complications since 1995 from anterior lumbar interbody fusion (ALIF) (see Table 96–2). This is in part due to increased reporting of complications but also due to the absolute increase in the number of cases. Anterior exposure of the lumbar and lumbosacral spine can be accomplished by a lateral retroperitoneal approach,45,190,203–205 a transperitoneal approach,174,206,207 or a paramedian hypogastric “mini open” (rectus-splitting or minimally invasive anterior lumbar) retroperitoneal approach.190,204,205,208 Monitoring of the left great toe pulse oximetry is necessary to identify early and reversible left iliac artery occlusion during the surgical procedure. The lateral retroperitoneal approach was initially described by Fey as a modified sympathectomy approach.190 All approaches directly address the vascular structures of the anterior lumbar spine best used for L1-L3 exposure.203,209–211 Although the rectus-splitting anterior or paramedian exposure is specifically limited to L3 to S1 due in large part to the renal arteries branching from the abdominal aorta (Fig. 96–21). There is a high degree of anatomic variability in these structures, especially for the iliocava bifurcation and the segmental vessels (Fig. 96–22). The incidence of the vascular injuries from anterior lumbar spinal surgery varies and is still believed underreported (see Table 96–2). For example, Cohen and colleagues204 reported no vascular complications in 66 cases involving lumbar exposure, whereas Baker and colleagues41 in 102 consecutive cases performed by fellowship-trained vascular surgeons reported a 15.6% incidence. Baker and colleagues41 reported complications such as tearing of the recurrent iliolumbar vein, and they found a 7.7% incidence with the lateral or flank exposure compared with 18.4% with a rectus-splitting retroperitoneal exposure. However, there was no significant morbidity or mortality in Baker’s series. Depending on the spine surgeon’s level of expertise and hospital credentialing, a collaborative effort with a surgeon experienced in vascular surgical techniques is often required or necessary, especially in the increasing number of anterior lumbar revision cases.41,212,213 Vascular injuries and complications during anterior lumbar exposures rarely result in serious sequelae unless the injury results in total disruption of the vascular channels to the lower extremity or other important viscera.131 Prompt recognition and repair remain the standard of care. Blood conservation techniques such as cell saver and/or autologous blood donation are recommended to address the effects of anterior thoracolumbar vascular complications.214
As anterior lumbar interbody fusion and arthroplasty techniques have gained wide acceptance, laparoscopic or “mini-open” rectus-splitting approaches have fallen into disfavor, especially for lateral exposure at L4-5 and below.* Vraney and colleagues221 noted that laparoscopic exposure of L3-L4 required significant aorta retraction in more than 9 out of 10 angiographically studied patients. Dewald and colleagues208 easily gained access to L3-4 and above using a mini-open rectus-splitting exposure, as did Brau.222 Exposure of the anterior lumbar spine may be performed with open or laparoscopic techniques. Open techniques can be done with a small versus large incision, retroperitoneal versus transperitoneal, and in cases requiring exposure and treatment of higher lumbar segments for example (L3-4) can be approached through an anterolateral retroperitoneal exposure (Fig. 96–23). Advantages and disadvantages with all of these alternatives exist. Choices will be dictated by (1) the surgical pathology, (2) the vascular and spine surgeon’s preference and experience, (3) prior abdominal surgery, (4) size and weight of the patient, (5) the risks of retrograde ejaculation in males, and (6) any special patient preferences and/or requests. Kaiser and colleagues48 performed a comparative study between the limited or mini-open retroperitoneal anterior lumbar exposure and that of the laparoscopic approach. The laparoscopic approach was used in 47 patients, and the mini-open technique was used in 51 patients forming the basis for comparison. Operative time and preparation was increased in the laparoscopic group. The length of hospital stay was slightly longer in the mini-open anterior lumbar interbody fusion technique procedures. More importantly, the rate of retrograde ejaculation (injury to the superior hypogastric plexus) was markedly higher in the laparoscopic group at 45% versus 6% in the other group. In their series there were no vascular complications reported, and no distinct advantage between the two techniques was noted.
The lateral or anterolateral exposure of the lumbar spine is most appropriate for pathology at or above L3-L4.190 The left side is chosen if all else is equal owing to the resiliency of the aorta compared with the vena cava. However, the side of exposure is most often dictated by the pathology. Considering the lateral or flank exposure of the retroperitoneum, the psoas major can be relaxed by flexing the hip and knee, rendering vascular dissection safer and easier. Incisions are placed according to the vertebral level of interest, and the approach is carried to the retroperitoneal space. The psoas major is the key landmark to guiding the deep dissection. Each segmental vessel is independently isolated over the concave vertebral body with a right angle hemostat and clipped or ligated. Double ligation or clipping is preferred toward the great vessels, leaving at least 1 cm of lumbar segmental vessel to prevent making a hole in the aorta or vena cava. The use of clips versus suture ties is largely dependent on surgeon preference. Ligation of the segmental vessels should be over the middle of the vertebral body. By staying away from posterior ligation of the segmental vessels, the risk of interference with foraminal or collateral blood flow is reduced. In addition, it is technically easier to control the vessels in this anatomic location. If the ligature, suture, or clip should tear or dislodge, the major vessel can develop a large perforation in its sidewall. Regardless of the type of anterior exposure, access to the vertebral bodies and intervertebral discs will require identification, mobilization, control, ligation, and/or protection of the arteries and veins that cover the anterior lumbar spine.*
In most cases the vascular surgeon will provide this for the spine surgeon, but it is important for the spine surgeon to be knowledgeable about the nuances of this component of the anterior procedure.41 This is especially important in identifying the left recurrent iliolumbar vein off the left common iliac vein. This vessel is of variable size and anatomic origin of the common iliac vein. It may branch from the left common iliac vein posteriorly or from the superior lateral margin of the left common vein. In a review article, Watkins emphasized four key vascular components and considerations for anterior lumbar exposure that must be addressed: (1) the iliolumbar vein, (2) the left iliac vein, (3) the middle sacral vessels, and (4) the type of arterial retraction so as to optimize exposure but minimize the risk of altered blood flow or displaced plaque.220 Exposure of L5-S1 is probably the easiest vascular window. Capellades and colleagues,209 in an MRA-based study, found that 18% of their cases showed the iliocava bifurcation occurred at or below the L5-S1 intervertebral disc space. Tribus and Belanger,240 in a recent gross anatomy study of the L5-S1 level, demonstrated the relationship of the vena cava, aorta, and right and left common iliac arteries and veins (Fig. 96–24). In almost all cases, the left common iliac artery and vein will require mobilization from the midline to the left to visualize the entirety of the L5-S1 intervertebral disc. The left common iliac vein averaged a distance of only 12 millimeters from the midline. The middle sacral artery and veins were constant vessels over the L5-S1 intervertebral space but varied as to the exact position and size. Sacrifice of the middle sacral artery and vein is a routine component of any L5-S1 exposure, but this artery does not in reality mark the true midline at the L5-S1 disc space.
Exposure of the L4-5 level and above will require mobilization of the vena cava and aorta by sacrificing and ligating segmental vessels and the recurrent left iliolumbar vein. Kleeman and colleagues213 demonstrated three general anatomic patterns on the basis of MRI and clinical experience as the “best window” to the L4-5 interspace. Kleeman showed that the aorta and vena cava, as well as the left common iliac vein and artery, can be taken together or independently from side to side or from a caudal to cephalad direction, depending on the level of the iliocava bifurcation (Fig. 96–25A-C).213 In cases where there is a low iliocava bifurcation, the left common iliac vein is taken from left to right and the window to the L4-5 disc is obtained by mobilizing the left common iliac artery to the left. There is no case in which the aorta, vena cava, or common iliac vessels are mobilized from right to left given in large part due to relative frailty of the vena cava and potential for tearing, laceration, or avulsion. This may be an exposure of revision anterior surgery such as revision or removal of a total disc arthroplasty. As one extends the exposure to levels above L4-5, the aorta and vena cava are almost always mobilized together from left to right. There may be times in which a window needs to be created between the aorta and vena cava. Kleeman and colleagues,213 in their 139 cases, warned that transperitoneal laparoscopic release and mobilization of the left segmentals of the aorta at L4-5 were associated with a 16% rate of retrograde ejaculation. This caused the authors to recommend an alternative exposure for the L4-5 interspace between the aorta and vena cava in low iliocava bifurcations (Fig. 96–25D). By contrast, Brau241 reported one case of retrograde ejaculation in 684 patients using a mini-open rectus-splitting anterior approach from L2 to S1. Cases in which there are multilevel anterior lumbar interbody fusions that extend from L5-S1 to L3-L4 will require that an anterior exposure be provided by multiple approaches. However, retroperitoneal exposures that mobilize the sympathetics with the peritoneum have the least risk of retrograde ejaculation. In comparison, transperitoneal exposures have a 7 times increased risk of retrograde ejaculation.242 At the end of the case, once all retractors are removed, the vessels can be inspected for any obvious bleeding that may have been tamponaded by the retraction process and directly palpated to exclude occlusion or thrombosis from retractor positioning. A retractor system (hand-held and/or self-retaining) (Fig. 96–26) should be chosen with the vascular surgeon to protect overstretching the vessels but allow for adequate exposure.243 It is probably best to use these retractors to retract the peritoneum and its contents. Vascular retraction is usually done safely on the hand-held retractors (e.g., Wiley retractors; see Fig. 96–26). Continuous monitoring of the left great toe pulse oximetry is key and has become the standard operating procedure for anterior lumbar surgeons when the aortic or the left common iliac artery is involved.244,245
Rapid and large quantities of blood loss can occur if the segmental lumbar vessels, aorta, or vena cava are lacerated or torn (see Figs. 96-21, 96-23, and 96-25). The left common iliac vein and iliolumbar vein are the vessels most at risk in lower left-sided retroperitoneal spinal dissections. Bleeding is always initially controlled by direct pressure. Ligation of the segmental vessels is assisted by carefully compressing the aorta and vena cava medially to identify the bleeding source. Repair of the abdominal aorta, especially the vena cava, requires expertise in vascular surgery. While waiting for the vascular surgeon, bleeding should be controlled by direct pressure with a sponge on a clamp or even a well-placed finger. Exposure of the lumbar spine anteriorly requires dissection and mobilization of the segmental vessels.213 Cases of life-threatening vascular injury from anterior lumbar spinal surgery are uncommon. Illustratively, Dwyer and Schafer142 averaged 1800 mL blood loss in their 51 cases, but no irreparable arterial or venous injuries were reported in using this Dwyer cable fixation.
Baker and colleagues41 reviewed 102 consecutive cases of anterior lumbar spinal surgery performed for a wide variety of lumbar spinal conditions (L3-S1), all assisted by fellowship-trained vascular surgeons. The overall incidence of vascular injury was 15.6%. All injuries involved the more fragile, thin-walled venous structures: 11 common iliac vein injuries, 4 inferior vena cava injuries, and 1 iliolumbar vein injury. All injuries were identified and repaired primarily (5-0 or 6-0 polypropylene [Prolene] sutures) without any reported clinical significance. The incidence of venous injury differed by the extent of surgical approach. The hypogastric “mini-incision” rectus muscle–splitting approach was associated with an 18.4% of vascular complication rate versus a 7.7% incidence with an anterolateral muscle dividing retroperitoneal exposure. This type of study emphasizes the relatively common association of vascular problems with anterior lumbar spinal cases, even in expert hands. Primary repair is the standard of care except for segmental vessels, which can usually be sacrificed at the first surgery unilaterally. Successful repair did not cause any sequelae other than one case of DVT requiring vena cava filter placement. More recently, Brau reported a 1% incidence of arterial and venous injuries each using a “mini-open” technique in 686 exposures.222 There were minimal serious morbidity issues or mortality in Brau’s cases (see Table 96–3).222 Hohf found three cases of major arterial injuries from anterior lumbar spinal surgery, two from disc excision and the other from an anterior vertebral body exploration.131 Louis reported a series of 440 cases involving anterior lumbar surgery over a 10-year period that only resulted in two vascular complications: one common iliac vein laceration and one inferior vena cava thrombosis.97 The repair of the lacerated common iliac vein was done primarily and did not have any serious sequelae despite severe hemorrhage. Kozak and colleagues206 reported two venous injuries in a recent series of 45 open anterior lumbosacral spinal reconstructions. One involved the iliolumbar vein with 1500 mL of blood loss, and the other involved 2000 mL of blood loss due to a 3-mL vena cava tear. Both were recognized primarily and either ligated (Iliolumbar vein) or repaired (vena cava) without sequelae. These authors also reported a rare vascular complication in which a rectus sheath hematoma developed from an inferior epigastric artery tear due to forceful coughing in a patient 3 days postoperative that had to be drained and ligated. Paresis of the abdominal wall in lateral retroperitoneal exposures is almost universal and a source of complaints by many patients. Other authors have reported large series or anterior interbody fusions of the lumbar spine for degenerative disc disease and spondylolisthesis without major vascular injuries (see Table 96–2).24,126,186,208,212,215,246–251
The transperitoneal approach, described by Lane and Moore, offers direct extensive access to the lumbosacral area but has been supplanted by retroperitoneal techniques in most primary open cases.207 The transperitoneal exposure appears to be one of the key revision approaches to the lower lumbosacral spine. In order to minimize vascular-related complications, Brau recommends the mini-open or rectus-splitting exposure using transverse skin incisions with exposures for L2-3 and L3-4 above the umbilicus and for L4-5 and L5-S1 below the umbilicus.222 He emphasizes that the keys to safe exposure to the hypogastric rectus-splitting anterior retroperitoneal exposure are for the surgeon to (1) stand on the patient’s left side; (2) make a transverse or longitudinal incision depending on the number of levels; (3) identify the lateral edge of rectus muscle on the left and mobilize it; (4) incise the posterior rectus sheath or tranversalis fascia by 4 to 5 mm to visualize the peritoneal sac with or without its retroperitoneal fat; (5) use the finger and hand dissection to release the peritoneum up and down and sweep laterally to the left to the retroperitoneal space; (6) identify the iliopsoas with the genitofemoral nerve and the ureter; (7) place the self-retaining (Balfour, Hayden Medical, Inc., Santa Clarita, Calif., or Bookwalter, Codman, Johnson & Johnson, Raynham, Mass.) retractor relatively anterior, retracting the retroperitoneum handling the vessel with hand-held retractors to the right; and (8) isolate, ligate, and mobilize the vessels as needed depending on the level and extent of surgery planned.222 Whether or not the surgeon exposes retroperitoneal or transperitoneal, the potential vascular complications are similar, but the retrograde ejaculation rate is higher in the transperitoneal group. The surgeon must work at the bifurcation of the abdominal aorta and at the formation of the common iliac veins from the vena cava (see Figs. 96-24 and 96-25). The middle sacral vessels have to be sacrificed for exposure of L5-S1. The left common iliac vein, as it passes dorsal to the aortic bifurcation, becoming ventral and inferior to the left common iliac artery, is vulnerable to laceration and tearing. Should the bifurcation of the major vessels be more caudal (10% to 20% in some series) at the L5-S1 disc level or exposure above the L4-L5 disc level be desired, mobilization of the vessels will be necessary. If this approach is chosen, it may be helpful to perform preoperative digital subtraction angiography or abdominal ultrasonography to confirm the level of the bifurcation of the aorta and vena cava. This is particularly applicable to the newer techniques like total disc replacements (Fig. 96–27). Bleeding may be profuse and difficult to localize in this region of the retroperitoneum. It is recommended that the use of electrocautery in this area be limited due to the risk of injury to the sympathetic nervous system (superior hypogastric plexus). Some authors have suggested infiltrating the retroperitoneal space with normal saline and/or using bipolar electrocautery to aid in preserving the parasympathetic and sympathetic nerves.252 Clearly, transperitoneal exposure has a higher risk of retrograde ejaculation because the inferior sympathetic plexus must be exposed transperitoneally rather than lifted and swept right to left with the peritoneum as in the retroperitoneal exposure.
Laparoscopic anterior lumbar procedures continue to be alternatives to open procedures in some centers. As with any anterior lumbar approach, there are potential but not unique vascular complications. Because laparoscopic anterior spinal surgery requires a pneumoperitoneum to adequately visualize the lumbar spine, intervertebral disc, and vascular anatomy, the approach is actually a limited transperitoneal exposure. As such, the rate of postoperative ileus and retrograde ejaculation are reportedly higher than those of open retroperitoneal techniques.213 Vascular injuries associated with laparoscopic-assisted anterior lumbar procedures include (1) segmental vein lacerations, (2) excessive bleeding from bone at the intervertebral disc space in discectomy cases, (3) iliac vein tears and lacerations, (4) presacral vein lacerations, and (5) iliolumbar vein lacerations and tears. Bowel and bladder injuries have also been reported by Kleeman and colleagues213 at a rate of 1.4%. Regardless of the surgical series, most laparoscopic exposure-related vascular injuries occur early in the reported series and also exclusively involve veins, not arteries. Nordestguard and colleagues253 reported several major vascular injuries during laparoscopy reporting 5 new cases and about 20 more from a literature review. These injuries characteristically involve the distal aorta, distal vena cava, and iliac or iliac veins. Interestingly, four of the injuries were not recognized immediately and three of these led to death from exsanguination. At laporotomy, the field of vision and the open exposure was severely compromised because of the massive blood loss. McAfee and colleagues254 reported a single common iliac vein laceration during the first 100 endoscopically assisted anterior thoracolumbar spinal reconstructive procedures. This singular case required an open conversion from a laparoscopic procedure to an open one for repair. The authors wisely suggest routinely setting up for such an occurrence, emphasizing the need for preparation and early treatment of large vessel injuries, especially those involving the vena cava or common iliac veins. Regan and colleagues218 and Zdeblick255 converted 2.4% and 3%, respectively, of their initial series of laparoscopically associated anterior lumbar interbody fusions as a result of inability to see or control venous injuries. Recently, contemporary techniques of limited transperitoneal laparoscopic exposure have significantly lessened the risk of morbidity and mortality but the technique has fallen into disfavor primarily due to the increased rates of retrograde ejaculation.216,256
When vascular injuries occur during laparoscopically assisted anterior lumbar spinal surgery, the treatment is either (1) laparoscopic control ligation or repair or (2) conversion to an open transperitoneal case, followed by ligation and repair of the source of bleeding as appropriate. Heniford and colleagues217 warned that the left iliac vein, which commonly must be mobilized for access to L5-S1, is susceptible to compression with as little as 15 torr of pressure from the pneumoperitoneum. This may make differentiation of the left iliac vein from the peridiscal tissue difficult. Laparoscopic repair of venous injuries requires patience, experience, proper equipment (specialized Kitner forceps), and technical skill as outlined by Heniford and colleagues217 and others.218,253,256,257
Delayed aortic erosion, laceration, and retroperitoneal hemorrhage have been reported in three cases in which the Dunn device (now off the market) was used anteriorly for thoracolumbar spine burst fractures.258 Although this device is no longer in use, it illustrates potential delayed vascular complications with anterior implants with sharp edges. In 1985 Brown and colleagues258 reported 3 cases out of 22 instrumented procedures. Blood loss varied from 8000 to 15,000 mL and manifested itself 21 days to 9 months postoperatively. All these devices were placed on the left side, and a sharp edge on the device was implicated as the cause of the delayed aortic rupture. A similar experience with the Dwyer cables, Zielke instrumentation, and other anterior systems has not been encountered.54,142,181,192,218,222 However, Ohnishi198 recently reported that a grossly loose Kaneda device with a smooth margin migrated in a 53-year-old male at T11. This caused compression of the aorta, and a pseudoaneurysm developed on the left 24 months after surgery. The device was ultimately removed, and the pseudoaneurysm was repaired without lasting sequelae.176
Marsicano and colleagues75 reported a rare case of thrombotic occlusion of the left common iliac artery in a 59-year-old male with peripheral vascular occlusive disease following anterior spinal surgery (see Table 96–4). Iliac-iliac open revision bypass grafting was required with resolution of the patient’s postoperative neurologic complaints. Vascular insufficiency of the patient’s left leg followed the left lateral retroperitoneal exposure and was noted on a delayed basis postoperatively. Common iliac artery occlusion or thrombosis is rare and is a true spinal vascular emergency. Raskas and Delamarter13 also reported a case of left iliac artery occlusion presenting immediately on awakening in a 67-year-old woman after a four-level anterior lumbar discectomy and fusion. She presented with left leg paralysis, loss of pulses, and loss of sensation hours after her surgery, detected in the postanesthetic care unit (PACU). After arteriography, the patient returned to surgery, where a bypass graft was necessary after thrombectomy was unsuccessful. The authors stress prompt diagnosis to decrease muscle ischemia time to less than 6 to 8 hours and monitoring the compartment pressures should this routine complication occur. If an iliac artery occlusion is suspected, immediate or emergent exploration of the vessel is preferred rather than losing warm ischemia time with diagnostic angiography. Intraoperative angiography can be done if the level or degree of occlusion is not apparent. This author is aware of a case of iliac artery occlusion occurring 6 to 8 hours after the anterior stage of a two-stage anterior posterior procedure. The clot was evacuated within 8 hours of the left iliac thromboses, but ultimately the patient died of MOD. Once flow was reestablished, a reperfusion syndrome occurred.
In aortic or common iliac artery surgically corrected occlusion, a reperfusion syndrome may occur in which the physical findings are early lower extremity sensory and motor deficits below the knee. Also in the initial phase, weakness, especially in the L5 and S1 distributions, predominates. Ultimately, there is a pale, mottled, cool extremity, and this can develop late and or slowly after surgery. These symptoms can occur variably after surgery. This complication is life and limb threatening. Endarterectomy is a treatment of choice. Rhabdomyolysis with reperfusion is a potentially fatal late complication. Reperfusion syndrome is likely fatal, and lower leg compartment syndromes are to be expected with warm ischemia over 6 to 8 hours. Brau restated that the standard of care for the early diagnosis and prevention of arterial thrombosis is a pulse oximetry monitor on the left toe.241 In more modern protocols the introduction of adverse events remains relatively common in spinal surgery, estimated at one in six cases; however, only one out of four (25%) of these complications are thought to be reduced by evidence-based clinical practice protocols.
A reperfusion syndrome is defined as an altered blood flow or ischemia that can further cause tissue and organ damage.259 In its most severe presentation, MOD occurs with about a 1 in 2 mortality rate in the intensive care unit (ICU). Cellular effects of the reperfusion syndrome are summarized in Table 96–5. The effects of the ischemia predetermine how treatment can control reperfusion and provide antioxidants, complement, and serologic factors. Optimal treatment limits these effects or at least seeks to control and minimize some of these effects. For example, in an anterior left common iliac artery thrombosis, early treatment is important because as reperfusion starts, the effects of ischemia are set in motion in the underperfused tissues. Ideally, this reperfusion is done in a controlled fashion if at all possible. In one of Brau’s cases, he had to tie off the vena cava to control bleeding.260 This led to chronic irreversible bilateral lower extremity edema. Further, clinical effects of MODs include myocardial stunning, reperfusion, arrhythmias, central nervous system–effect-like strokes, gastrointestinal-effect-like bleeds or infarction, and renal failure. If all of these occur in a combination, this is called MOD. Risk factors for MOD have been identified as sepsis, major trauma, septic shock, aortic cross clamping, lower extremity ischemia, burns, circulatory shock and collapse, pancreatitis, and immunologic disorders. The theoretical treatment principle includes a timely reperfusion with antioxidants, complement, and leucocytes. The author is also aware of three cases of left common iliac vein thrombosis; one occurred postoperatively without risk factors, and the other two occurred after extensive repair of the left common iliac with occlusion of the vein diameter by greater than 50%. Adding fractionated heparin or warfarin should be considered if the risk of neurologic deterioration from an acute epidural hematoma is considered low.
Cellular aspects of ischemia and hypoxia in the early stages of a reperfusion syndrome. These are fairly well understood, but not all of these can be controlled directly. This is best addressed by a relatively slow, controlled reperfusion of the extremity when possible.
The vascular complications in disc arthroplasty can be divided into three groups: (1) exposure related, (2) retraction related, and (3) late complications related to the implant stability and/or need for revision and for total disc arthroplasty failure with anterior extrusion (early). Numerous authors have elucidated the close proximity and vascular anatomy of the anterior lumbar spine related to the aorta vena cava, segmental vessels, and recurrent lumbar vein, as well as the common iliac artery and vein. Implantation with total disc arthroplasty is essentially identical to an anterior lumbar interbody fusion except that the exposure is more extensive—the entire anterior surface or margin of the intervertebral disc needs to be seen for a total of 120 degrees of the anterior annulus fibrosis. At L5-S1, this is relatively easily accomplished, but L4-5 and L3-4 are much more difficult while preserving arterial and venous blood flow.261 Retraction is always necessary after ligation and control of the left segmental vessels, as well as the recurrent or ascending lumbar vein. Most access surgeons use some type of retractor that attaches to the operating room table. It is important that this retractor be able to move with the patient and that the retractor concentrates on retracting the ureters and peritoneum and not the vessels.262 Multiple factors such as peripheral vascular occlusive disease, age, weight, and vessel pliability determine if the great vessels are incorporated into a fixed retractor setup. By and large, this should be avoided because it can produce variable constant pressure and may lead to venous or arterial occlusions. The concern is occlusion of the aorta, vena cava, or common iliac arteries and veins. Laceration, embolization, delayed DVT, and vasospasm are all possible adverse events, which may also lead to significant complications (0.6%). Kulkarni also showed increased incidence of thrombosis with Steinman pin retraction, which was initially recommended in Charite TDA.263 With this technique, the incidence almost doubled if the pins were used for more than 30 minutes (see Fig. 96–27). Retractors (see Fig. 96–26) are blunt tipped and have concave edges, so they can be placed under the vessel and retraction can be variable, adjusted, and gentle. At times this requires working in steps, minimizing the time of arterial retraction (or occlusion) often working side to side at the disc avoiding constant retraction from right to left at that particular disc level (see Fig. 96–27).
Multiple reviews of lumbar total disc replacement have identified the most common vascular adverse events as left common iliac vein laceration (5%), vena cava laceration (2%), and thrombosis of the left common iliac vein or left common iliac artery (<1%).264 The latter is most common in two-level cases, as reported by Hannibal.265 This is directly due to the relative immobility of the aorta and vena cava branching into the common iliac artery and vein at or near the L4-5 disc space in the majority of cases.100 Thrombosis of the left common iliac artery and/or left common iliac vein is a surgical emergency. Unfortunately, thrombosis is not always present at the time of closure or noted on the pulse oximetry. Evaluating pulses before closure and after retraction should be routine and recommended. The left leg neurovascular assessment should continue in the PACU.262,266 Unfortunately, most reported cases of left common iliac artery thrombosis are diagnosed on a delayed basis. Restoring circulation is the priority and requires a thrombectomy and arterioplasty. These may not be able to adequately restore flow, depending on multiple factors including the presence or absence of emboli, delay in diagnosis, and with warm ischemia times of 6 to 8 hours or longer. If this occurs, there are likely to be varying degrees of rhabdomyolysis and elevated compartment pressures requiring a prophylactic fasciotomy. A rapid reperfusion syndrome is likely to occur as previously reviewed. Left leg amputation and/or death may be the final sequelae. Thus most vascular complications in anterior lumbar surgery and/or total disc replacements are exposure related, Most of the lacerations of venous structures are usually easily identified and repaired with 4-0 or 5-0 Prolene sutures. The major life and limb risk is the secondary formation of an arterial thrombosis. Hackenberg has reported left common iliac artery thromboses from hours to 13 days.266 Initially, this type of occlusion is easily and often confused with vasospasm. On the other hand, Kulkarni263 showed that all either occurred intraoperatively or within 2 hours of surgery. Arterial occlusions are more common in smokers in whom there is an 80% increased risk of thrombosis.263
Revision anterior lumbar surgery is a new and evolving frontier with limited data compared with primary anterior lumbar surgery (Table 96–6). Principles noted here are applicable to any failed anterior spinal surgery with or without instrumentation. These principles will vary by the exposure, time to revision, levels involved, experience of the access surgeon, and nature of the failure. Bertagnoli divides anterior lumbar revisions into three categories: (1) those that can be handled posteriorly only, (2) those that require partial anterior exposure and treatment followed by posterior stabilization, and (3) those requiring full access anteriorly and treatment both anteriorly and posteriorly.267 Approaches include (1) reusing the initial left rectus-splitting retroperitoneal exposure (most often used in early cases of failure), (2) right rectus-splitting retroperitoneal exposure, (3) transperitoneal exposure, or (4) an anterior lateral retroperitoneal exposure either right or left depending on the pathology. Preoperative preparation and planning for revision are crucial and include (1) venous balloon catheter placement for emergency bleeding, (2) setup and use of the cell saver, (3) a left lower extremity pulse oximetry, (4) urethral catheterization, (5) varying the approach to address the pathology at this point (≈90% to 95% of cases can be redone through the same incision according to Bertagnoli), and (6) preoperative arteriography or some other equivalent noninvasive study such as a CTA (see Table 96–6).267 The technical aspects are further expounded elsewhere (see Chapters 51, 97, and 99), but suffice it to say that the vascular complications, especially venous, are more likely; a greater blood loss is expected; and there is a possibility that the case may have to be abandoned anteriorly in some excessive cases.267 To illustrate, revision cases in which venous lacerations and/or bleeding has gotten out of control with the vessel becoming irreparable have been reported. Unfortunately, this massive hemorrhage could not be stopped and led to death. As experience grows, alternatives to anterior or anterolateral exposure will improve and reflect the current state of knowledge and experience.
TABLE 96–6 General Recommendations for Revision Anterior Lumbar Surgery
From Brau SA, Delamarter RB, Kropf MA, et al: Access strategies for revision in anterior lumbar surgery. Spine 33:1662-1667, 2008.
Posterior Lumbar Vascular Injuries
Vascular complications in posterior lumbar spinal surgery are almost always associated with lumbar discectomy.268 By contrast, Smith and Lawrence reported a vascular complication associated with a lumbar laminectomy without discectomy for acquired spinal stenosis.52 A 62-year-old man developed high-output cardiac failure and hypovolemic shock with an expanding right retroperitoneal hematoma due to laceration of a segmental vessel caused by neuroforaminal probing. A blunt-tip gallbladder probe was used at L3-4, tearing the right fourth segmental artery. Similarly, an 84-year-old patient with kyphoplasty had an L4 segmental bleed requiring segmental angiographic embolization.269 The exact incidence of lumbar vascular complications associated with lumbar discectomy is not known, but estimates of less than 0.05% have been offered (Fig. 96–28).89 More than 300 cases of vascular complications associated with discectomy have been published, usually as case reports, or in small retrospective series.* These appear in periodicals of vascular and cardiovascular surgery, general surgery, orthopaedic surgery, neurosurgery, urology, and internal medicine, thus emphasizing the complexity and vast spectrum of vascular and/or visceral injury complicating lumbar discectomy. Even, prone positioning a morbid obese patient can cause a vascular complication (external iliac artery occlusion) just by pressure exerted in positioning on a 4-poster frame.282
In 1945, about a decade after the first discectomy, Linton and White26 reported a case of arteriovenous fistula formation between the right common iliac artery and the inferior vena cava after a L4-L5 discectomy. Three years later, Horschler275 reported another case of arteriovenous fistula formation after an L4-L5 discectomy and stated he knew of five more cases that had occurred over the previous 5 years. Hohf131 surveyed more than 3500 orthopedists with a 33% response rate as to the arterial injuries from orthopedic surgery. He found 58 well-documented cases of major vascular injury secondary to disc surgery, 17 of which resulted in death. Disc surgery clearly was the most common procedure resulting in major vascular injury and death. DeSaussure284 surveyed 739 neurosurgeons and 2228 orthopedic surgeons and discovered 106 cases of major vascular injury secondary to disc surgery. Mortality rates varied from 16% to 100% depending on the timing of surgery and the type of vascular injuries. Arteriovenous fistula formation was the most common vascular sequela secondary to disc surgery. In 1976 Jarster and Rich276 reviewed 68 cases of arteriovenous fistula formation and added 5 more cases. Tsai and colleagues285 reported the first case of a superior rectal artery laceration following lumbar discectomy. The patient presented subacutely with hypotension, tachycardia, and signs of hypovolemia in the postoperative period. Because this was a smaller-caliber vessel, percutaneous elective endovascular embolization could be successfully employed. Sporadic case reports and small retrospective series continued to appear, but this serious vascular complication secondary to lumbar discectomy (most commonly at L4-5) disc surgery does not appear to be decreasing.268 Despite being recognized as a known risk of lumbar disc surgery, major vascular injury tends to result in legal action. In a review of 21 cases from 1985-1997, Goodkin and Laska25 noted that all such complications went to litigation and a settlement or verdict was rendered in all cases. According to these authors, this potential disastrous complication does not represent negligence per se because the complication may occur without the surgeon being aware of the injury at the time of surgery. It behooves the spine surgeon to understand methods to avoid such complications, provide informed consent, and understand how to recognize the signs and symptoms of this rare complication.25 In regard to informed consent, Goodkin and Laska25 found that failing to specifically discuss vascular injury is not below the standard of care because death as a complication is usually mentioned, but the authors recommend that this specific complication be specifically mentioned in the informed consent process.
Vascular injury during lumbar discectomy occurs most commonly at the L4-L5 level, followed by L5-S1 (Fig. 96–29; see Fig. 96–28). To some extent, this incidence reflects the frequency of symptomatic disc herniations in the lower two disc levels; however, the vascular proximity at the anterior L4-L5 interspace directly contributes to this higher incidence. Szolar and colleagues238 reported that the left common iliac artery is the most common vessel injured, complicating lumbar discectomy. Bass and colleagues noted that vascular complications associated with lumbar discectomy occurred in six categories: (1) laceration of the aorta or vena cava with immediate hypovolemic shock, (2) lacerations of the iliac vessels with or without immediate hypovolemic shock, (3) partial avulsion of a vessel wall with delayed hemorrhage or thrombosis, (4) injury incident to preexisting vascular disease such as an abdominal aortic aneurysm or atherosclerotic vessel walls, (5) false aneurysm and infected hematoma, and (6) arteriovenous fistula.34 The most common instrument implicated in these injuries are the pituitary rongeur and curette,191 of which “the pituitary rongeur is by far the primary instrument of destruction” (Fig. 96–30).7,279 Partial or total discectomy in DeSausssure’s series did not affect the incidence of vascular complications.284 Another contributing factor to vascular injury in discectomy is the failure to appreciate disruption of the anterior annulus fibrosis.286–288 Annular tear can commonly occur anteriorly or laterally as part of the degenerative process.287 Szolar and colleagues238 summarized risk factors for vascular injury during lumbar discectomy to include (1) preexisting degenerative disc disease, (2) retroperitoneal inflammatory processes leading to adhesions between the vessels and the disc, (3) aggressive “total” discectomy, (4) increased intraabdominal pressure that may force vessel or viscera against or close to the disc (especially if anterior annular tears exist), and (5) revision discectomy when annular tears are common. Adhesions can and do occur in anterior disc herniations and degenerative disc disease without prior anterior surgery, especially at L4-5 and L3-4 disc levels. Despite these multiple reports, injuries to the retroperitoneal vessels or viscera still occur. Injuries to the anterior vessel are still being reported with left L5-S1 discectomy. One study reported injury to the left recurrent iliolumbar vein, which is the first such venous injury ever reported.289 Another case report noted injury to the superior rectal artery during posterior lumbar discectomy.285
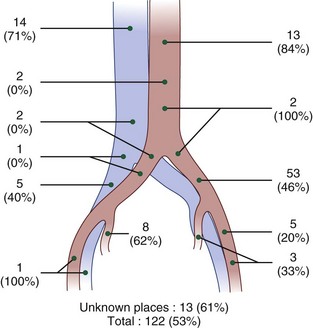
FIGURE 96–29 Cases of arterial venous fistulas reported by Morisi and Terragni, as modified by Montorsi and Ghiringhelli.
(From Montorsi W, Ghiringhelli C: Genesis: Diagnosis and treatment of vascular complications after intervertebral disc surgery. Int Surg 58:233-235, 1973.)
As anterior lumbar surgery rates have increased, as mentioned earlier, it is not uncommon to find adhesion or inflammation changes around an unoperated intervertebral disc (IVD) with degenerative disc disease. It is common to observe some peridiscal inflammation, especially at L4-5 with anterior disc herniations. Bolesta has reported an injury to the left common iliac vein in an obese male with prior surgery.42 The significance of peridiscal fibrosis was emphasized as a risk factor, as well as excess weight in this case. These risk factors are further illustrated by the fact that reports before 1990 of vascular injuries associated with lumbar discectomy ranged from 20 to 58 years of age compared with more contemporary reports where the patients are in the fifth and sixth decades of life.* Curiously, the majority of transforaminal and posterior lumbar interbody fusion techniques do not report vascular complications despite the extensive discectomy and endplate preparation required.67,186,246–248,290 One transforaminal interbody fusion technique incurred a rare injury and hemorrhage from the ipsilateral segmental vessel at L5-S1. Packing and coagulation with bipolar electrocautery stopped the bleeding.
*References 7, 10, 25, 33, 34, 42, 131, 162, 180, 187, 270–281.
Because of the incidence, severity of bleeding sequelae in lumbar discectomy, recognition, and prompt treatment of lumbar vascular injuries is essential.25,271 Definitive intraoperative findings include (1) brisk bleeding or blood welling up in the disc space, (2) hypotension with associated tachycardia, and/or (3) abdominal rigidity or a palpable mass. Other suspicious findings include fat or mucosa in the pituitary during discectomy, and this suggests retroperitoneal adipose, vessel, or visceral wall.25 Notwithstanding brisk arterial or venous bleeding from the disc space, there are no pathognomonic findings.271 Less than 50% of reported cases have bleeding from the disc space.25 Furthermore, less than 50% in DeSaussure’s series was recognized early.284 Intraoperative hypotension unexplained by anesthetic effects is the most sensitive and early diagnostic finding. Should bleeding occur intraoperatively from the disc space in association with hypotension, the interspace should be packed, the wound covered with a sterile dressing, volume expanders or blood started immediately, a vascular or general surgeon called emergently, the patient turned to the supine position, and the abdomen prepped and draped for an extensive transperitoneal laparotomy. Bass and colleagues34 suggest a generous longitudinal extensile abdominal incision. Options to surgically address the vascular injury include (1) suture repair of a tear, (2) resection of a damaged segment and graft or side-to-side repair, or (3) bypass graft or anastomosis when the injured segment of the vessel is ligated. If ligation of a major vein such as the internal or external iliac is required, thrombosis, lower extremity swelling, venous congestion, and thromboembolism (DVT or PE) are possible or even probable sequelae.273 It is not uncommon for these injuries to go undetected during the procedure, only to be discovered in the recovery room. During this perioperative period, unexplained hypotension, tachycardia, or abdominal signs and symptoms should alert one to the possibility of this complication.271 The clinical picture may mimic an ileus; however, the signs of shock are not expected in a paralytic ileus.
Arteriovenous fistula formation is the most common late or delayed vascular injury from lumbar disc surgery and has been recognized from 24 hours to more than 12 months postoperatively (see Fig. 96–29).26,271 After discectomy, arteriovenous fistula formation in one series most commonly occurred between the right common iliac artery and the right common iliac vein (29.1%), followed by the left common iliac artery to the left common iliac vein (25.5%), the right common iliac artery to the inferior vena cava (21.8%), the right common iliac artery to the left common iliac vein (12.7%), and others (10.7%)26. An extensive review by Quigley and colleagues268 found that the most common arteriovenous fistula was between the right common iliac artery and left common iliac vein. High-output cardiac failure with cardiomegaly is the most common presenting problem, found in 27 of 73 arteriovenous fistula cases reported by Jarster and Rich.276 Cardiomegaly and/or bruits over the abdomen after disc surgery should raise the level of suspicion, especially in a patient younger than 45 years. Various other presenting symptoms have been described including lower extremity pulse abnormalities (two), thrombophlebitis (five), abdominal pain (five), disc space hemorrhage (three), leg pain (two), lower extremity edema, (two) lower extremity varicosities (one), inguinal pain (one), and pulmonary embolus (one).270 Most often open surgical techniques for correction and repair are necessary. Recently, Tsai and colleagues285 and Lee and colleagues277 have been successful in the treatment of acute vascular complications, as well as arteriovenous fistula with percutaneous endovascular covered stent placement. These include stent placement, excision and grafting, selective embolization, and detachable balloons and microcoils. CT scanning is the preferred test to contrast the vascular injury, hematoma, vital organs, and osseous structures, especially in the subacute or delayed presentation (Fig. 96–31). Three-dimensional readings and spiral acquisition of the CT image can provide even more detail and definition.21 Radiographs of the abdomen may show free air if visceral injury occurs in association with a vascular injury.274 Obviously, angiography is mandatory in more chronic cases or if endovascular therapies are planned.21
To minimize the risk of a major vessel injury during lumbar discectomy, careful positioning and meticulous surgical technique is recommended.3,176,189,268,291,292 Operations are performed with adequate illumination and magnifications (2.5 to 3.5× loupes or operative microscope). A limited or subtotal discectomy is recommended in most cases because the results of partial lumpectomy or discectomy are equivalent to a more aggressive and complete discectomy.3,176 Experience confirms that this gives satisfactory long-term results with a success rate of about 90%. In contrast, DeSaussure commented on a series reported by Semmes involving radial discectomy with vascular injuries occurring in 1 out of 6000 cases284 that recommended only loose disc fragments should be removed. If not torn already, the posterolateral annulus is incised with a scalpel blade that is inserted no more than 4 to 5 mm in depth following a cruciate pattern. The pituitary rongeur is only inserted under direct vision and limited to less than 2.5 cm depth in most cases. More important than a depth measurement is the feel of the instrument against the endplates before opening and closing the jaws of the pituitary.25,33,274 There is no clear consensus, however, as to the “safe” depth of penetration by a pituitary rongeur with recommendations ranging from 2.5 to 4.5 cm. As shown by Gower and colleagues274 and Anda and colleagues,33 the angle or direction of insertion into the disc space also affects this distance due to the oval geometry of the intervertebral disc (Fig. 96–32). Judging these distances is absolutely more accurate on MRI or CT compared with plain films because discs vary by size, the sex and build of the patient, and intradiscal pathology.274 For example, Holschler summarized several important considerations for disc surgery.275 He emphasized that the surgery should only be performed for precise indications with hypotensive anesthesia, adequate exposure, and meticulous hemostasis. He suggested that the instruments not be inserted more than 2.5 to 3.75 cm below the posterior margin of the vertebral body at L2-L3 through L4-L5 and not more than 4 cm below the posterior vertebral margin at L5-S1. Marking scales on instruments by centimeters may improve the precision of this maneuver. Some have further suggested taking an intraoperative radiograph during the surgery for determination of depth, as well as for documentation reasons.25,274 Finally, he warned to remove the disc slowly, avoiding any forceful maneuvers. Routinely, the pituitary rongeur should touch the vertebral endplates to assure that the instrument is contained in the intervertebral disc space. Typically, the distance from the hinge jaw and the tip of the pituitary is about a centimeter. Probing of the interspace is not precise.274 Always remember, the goal of surgery is to relieve tension and/or compression of the nerve root, not to perform a total or subtotal discectomy per se. A 5% recurrence rate is preferable to even a single vascular injury during posterior limited discectomy.
Shevlin’s test is an intraoperative test for a potential large anterior annular defect, especially in the face of unexplained hypotension during posterior lumbar discectomy. The test is performed by filing the wound with saline, and if it escapes rapidly anteriorly, then an anterior disc defect is highly likely and may indicate a retroperitoneal vascular or visceral injury.293 The test is not pathognomic but highly suggests an anterior annular defect allowing the flow of fluids into the retroperitoneal space if the defect is present. Periodic education of recovery room staff has been recommended to help identify cases not apparent until after surgical lumbar discectomy, as well as other vascular complications such as iliac artery thrombosis and a pulseless or cold extremity. Unexplained hypotension, unusual abdominal symptoms, lower extremity pulse changes, leg swelling or engorgement, unexplained tachycardia, or a person who appears in shock without a good explanation should represent warning signs of possible significant vascular injury. Using these principles, vascular complications from routine and revision discectomy can be kept to a minimum but are unlikely to be completely eliminated.
Vascular injuries from lumbar disc surgery are serious complications. Mortality rates are variable (15% to 100%) and depend on the type of vascular injury.272,273,281 Death from a vascular injury during lumbar discectomy is called by some the “Jeff Chandler” syndrome, after a Hollywood actor who died from the complication.176 Early recognition and repair is not a guarantee of survival, especially in acute lumbar vascular injuries. Birkeland and Taylor270 give mortality rates from arterial and venous injuries of 78% and 89%, respectively. These complications tend to manifest early and require emergency attention. Even if patients survive, long-term morbidity may occur from ischemic consequences to sensitive organs like the brain and kidney, not to mention persistent low pain with or without radiculopathy.33,176,274 On the other hand, AV fistula formation ranges from 9% to 11%.284 DeSaussure reported mortality rates from 16% to 100% depending on the nature of the vascular injury and the temporal relationship between recognition and treatment.284 Newer technologies like percutaneous nucleotomy or laser discectomy can cause vascular injury. For example, a laser discectomy was done at L5-S1, indirectly injuring the left common iliac artery and requiring an emergency laparotomy.227
Visceral injuries are also reported independent of or more commonly in association with vascular injuries to the aorta, vena cava, and their branches.142,294,286 Incidences of associated visceral trauma are about half that reported for vascular injuries alone.275 Visceral injuries reported include (1) urethral damage, (2) small and large bowel perforations, (3) damage of the lumbar sympathetic nerve chain, and (4) pancreas.25,278,286 Al-Binali and colleagues294 reported a rare vascular and visceral complication presenting clinically 6 years after an elective posterior thoracolumbar instrumentation and arthrodesis for idiopathic scoliosis. This patient presented with an acute massive lower gastrointestinal bleed due to an internal iliac arterial fistula with the colon after bowel perforation. Surgical correction was required. The spine surgeon should be aware of the association of visceral injury in the unlikely event of a vascular complication following lumbar disc surgery. Finally, Hodge and Dewald294a reported two cases of splenic rupture and blood loss associated with anterior thoracoabdominal exposure for scoliosis. This occurred in one case during the exposure due to capsular adhesions from prior surgery. The other case presented on a delayed basis 1 week postoperatively, presumed due to the corrective forces applied to a three-staged rigid thoracolumbar scoliosis curve correction. Abumi and colleagues295 reported a 0.06% pedicle screw vascular injury complication rate. Smythe and colleagues296 published a unique case in which a sharp K-wire penetrated the aorta on the left at the level of the superior mesenteric artery, causing a major bleed that had to be opened.
Miscellaneous Vascular Complications
Thromboembolic Disease and Complications of Treatment
†References 6, 11, 41, 95, 204, 213, 243, 297–301.
* Patients with thromboembolic disease or DVT may present asymptomatically or with local lower extremity signs of calf pain, swelling, tenderness, a positive Homan sign, or redness and induration along the vein. Recent studies have established a variable incidence in patients undergoing elective spinal surgery.† Pulmonary embolism (PE) can occur as well and may be seen with a negative venous Doppler ultrasound of the lower extremity. Odu and colleagues300 found an incidence of thromboembolic disease of 5.6% in their 134 cervical cases compared with 26.5% in their thoracolumbar cases. Risk factors for DVT and PE are linked to the type and length of surgery. Patients undergoing complex spinal reconstructive surgery, often two staged, have a higher incidence of lower extremity thromboembolism, as well as PE. West and Anderson established a 14% incidence of thromboembolic disease as it relates to the length of surgery in their retrospective review.301 Prothero and colleagues279 identified several factors that heighten the risk of thromboembolism and/or PE. These include inactivity, recumbency, increasing age, obesity, cigarette smoking, anterior spinal procedures, and iliac crest bone harvest. Without explanation, the authors found that two thirds of the lower extremity DVTs occurred on the same side as the bone graft.279 Brau222 reported his experience with 686 anterior lumbosacral exposures, finding only a 1% incidence of thromboembolic disease comparing similarly to an incidence of 2% reported by Rajaraman and colleagues308 in 60 anterior lumbar interbody fusion cases. The diagnosis of DVT may be established definitely by invasive venography or secondarily by Doppler ultrasound. A spiral CT scan of the chest has replaced the ventilation perfusion scan with a high specificity and sensitivity and is the diagnostic test of choice for PE.300,309
The prevention of thromboembolic disease in patients undergoing spinal surgery is a double-edged sword. Traditional antithrombotic agents like heparin, antiplatelet drugs, fractionated heparins, and warfarin are relatively contraindicated owing to the high risk of epidural bleeding with or without epidural hematoma, whereas aspirin (acetylsalicylic acid) (81 mg) use is still debated.6,116,299,309,310 This risk extends well into the postoperative period, up to 4 weeks following the initial surgery.6,116,299,310 Universally it is recommend that intermittent pneumatic compression sleeves with elastic stockings be a primary mode of prophylaxis in patients undergoing all types of spinal surgery applied preoperatively.6,116,297,299,311 Bostrom and colleagues297 compared low-dose heparin with mechanical compression and alternating-day Dextran and found both reduced the incidence of thromboembolic disease by about a factor of four. Patients with proven lower extremity thromboembolic disease or patients with symptomatic pulmonary emboli are best managed by insertion of a vena cava filter.301,311 Patients undergoing complex anterior spinal reconstruction and who have two or more of the routine risk factors such as obesity, sedentary lifestyle, and history of prior DVT or pulmonary embolus are candidates for a prophylactic preoperative removable vena cava filter. More and more elderly patients presenting with surgical spinal disease are on warfarin for atrial fibrillation or other prophylactic reasons (e.g., transient ischemic attacks). Clearly, this should be stopped about 5 to 7 days before surgery, allowing the prothrombin time and international normalized ratio (INR) to normalize. Interval coverage with low-molecular-weight heparin is usually recommended to within 12 hours of surgery (dosing is usually mg/kg). This should be done in consultation with the patient’s medical and/or cardiac physician. When to reinstate the warfarin is controversial, and opinions vary from a few days to a few weeks after surgery. Spanier and Stambough312 report a case of epidural hematoma 2 weeks after a lumbar laminectomy and fusion in an elderly female with acute thromboembolism and concomitant heparin-induced thrombocytopenia started on intravenous therapeutic dosing of heparin and oral warfarin. Logically, anticoagulation can be given more safely in cases that do not involved laminectomy or corpectomy.
Heck showed that 21% have recurrent DVTs and 2.6% have fatal PEs after the first DVT. He summarized preexisting hypercoagulable states summarized in Table 96–7. Furthermore, he stated that the incidence of DVT with laminectomy or laminectomy and fusion is somewhere between 2.2% and 2.8%. In a review of 1954 patients, the DVT overall rate in the spine surgeries was 0.05% with no PEs. Prophylaxis was with low-molecular-weight heparin, but the downside was a 0.4% epidural hematoma incidence, and 40% or about half of those epidural hematomas went on to permanent paralysis. Thromboembolism incidence was 16% with stated anterior and posterior surgery.312 Factors such as age older than 60 or a body mass index (BMI) of greater than 30 kg/m2 highly correlated with DVT. Lumbar cases demonstrated a 5 times greater rate of DVT than cervical cases, but thoracic and lumbar cases were the same. As in extremity thromboembolism evaluation, there is a poor correlation between DVT and PE. Key factors in controlling thromboembolism include early mobilization, elastic stockings, and sequential compressive sleeves with risk of thromboembolism of less than 1%. In one study, low-molecular-weight heparin (nadroparin) at 2850 IU per day was successful in further reducing this rate. Rokito and colleagues in 1996 looked at mechanical devices versus warfarin monitored by noninvasive duplex scans. Invasive venography is still the gold standard in thromboembolism diagnosis. He reported an overall incidence of 0.03% with a case mix that included major spinal reconstruction of the thoracolumbar and cervical spine anterior and posterior. There was a 4 : 1 thromboembolism rate in lumbar versus scoliosis cases totaling 119 cases. No complications related to low-dose warfarin sodium (Coumadin) were directly due to the institution of the drug after surgery.305
In a survey, Glotzbecker and colleagues polled 94 spine surgeons with a 49% response rate. Of those that gave any prophylaxis, 12% would do it within 24 hours, 15% would do it after 24 hours, 22% after 48 hours, 13% after 27 hours, and 10% after 96 hours. Answers were based on the perceived “risk-to-benefit ratio.” There was a 5% to 10% rate of “late starters” of low-molecular-weight heparin, administered several days after surgery but rarely preoperatively. Glotzbecker identified a trend of placing inferior vena cava (IVC) filters before surgery. Among the responders, 77% would do that in a high-risk case in lieu of low-molecular-weight heparin.303 Clearly, no consensus exists and level I-II evidence-based studies are necessary.
Another retrospective study for DVT screening using ultrasound duplex found a 1.3% incidence of DVT where 0.3% were symptomatic of 313 patients. Cases involved major reconstructive surgery series with anterior and posterior decompressions with instrumented fusions. Despite a relatively high DVT rate, IVC filters prevented fatal PEs and were documented by Leon and colleagues313 in high-risk multiple surgical populations. They included all types of surgeries including spinal surgery. IVC filters were implanted in patients (1) with a history of DVT, (2) with thrombocytophilia, (3) with malignancy, (4) bedridden for more than 2 weeks, (5) having a two- to three-staged multiple-day procedure, (6) having anterior and posterior same-day surgery, (7) experiencing significant intraoperative blood loss, and (8) undergoing procedures lasting more than 8 hours. Twenty-two of 24 cases prophylactically used IVC filters. Twenty-five of 74 had isolated calf veins, and 1 out of 74 had a nonfatal PE. These data support the efficacy of IVC filters in that only 1 out of 74 patients developed a nonfatal PE in this high-risk group.313
Dearborn and colleagues314 showed the DVT rate in their high-risk reconstruction patients to be 0.3% with a PE rate of 2.2%; one PE was fatal. This study was a combination of 116 patients treated prospectively and 318 treated retrospectively. There were no IVC filter mechanical complications. Contemporary IVC filters are easier to apply and are removable. Duplex scanning poorly correlated with PE, and all PEs were after anterior and posterior surgery except for one occurring after an extensive, long, high blood loss, posterior spinal fusion, and reconstruction. These data among other anterior and posterior surgeries imply that anterior procedures alone or in combination when the major vessels are manipulated to some extent are more likely to develop thromboembolic disease.
Epstein315 studied perioperative thromboembolism in 100 circumferential cervical cases treated only with mechanical compression. She compared these data with her historic controls of heparin or miniheparin. These 100 cases had 1% PE and 1% DVT rates. Corpectomy cases had a slightly high DVT rate at 2% DVT with a 7% PE rate. All thromboembolisms and PEs were nonfatal. In high-risk cases, Epstein favored IVC filters before treatment and intermittent stockings or sequential compression boots during treatment.315
Fedullo reinforced the efficacy of IVC filters in high-risk patients regardless of the type of surgery (spine included) and discovered that IVC filters have a lower complication rate relative to bleeding than any other form of anticoagulation.316 Rosner and colleagues validated the use of IVC filters in high-risk major stage complex spinal reconstruction. In a follow-up, 74 patients had one or more of the following: a history of thromboembolism, thrombocytopenia, history of malignancy, bed rest for more than 2 weeks, staged reconstruction, two to three stages or with significant iliocaval manipulation, and operation time longer than 8 hours. Preoperative IVC filters in this group resulted in one nonfatal PE and 22 DVTs, most inferior to the IVC filter. No details were reported in the 22-patient pilot study and 74-patient additional follow-up study.317 Heppner and colleagues reported four cases of thromboembolism with a variety low-molecular-weight heparin, like aspirin, Coumadin, and heparin. No vascular complications occurred in this small series. Heppner reported four epidural hematomas in patients on low-molecular-weight heparin.318 Wong and Luk reported a rare case of an epidural hematoma under a spinal, well-formed thick fusion 30 years before a minor fall.319
Subdural and Epidural Hematoma
Epidural hematoma can be a catastrophic postoperative complication presenting with acute paraparesis or acute paraplegia.4,127,319,320 (See also Chapters 91 and 92.) Subdural hematomas are similar except they can occur without surgery, and the location of the bleed is different (subarachnoid versus outside the epidural space). Also, epidural hematomas involve vein bleeds compared with subdural hematomas, which involve arteries. Subdural hematomas are more likely to be expansile and cause neurologic deficits because they involve arterial tears and injuries. Risk factors for both include coagulopathy, thrombocytopenia, anticoagulation, the length of surgery, ankylosing spondylitis, poor hemostasis, and number of levels treated, especially if corpectomy is used.95,97,127,321 Immediate evacuation of the hematoma and decompression of the neural elements are the gold standards of treatment.
Diagnosis is primarily made on clinical presentation and may be confirmed with ultrasound, MRI, or CT myelography in a nonurgent clinical setting.128 The diagnosis of subdural hematomas and epidural hematomas on MRI classically shows an isointense T1 image and an iso-high intensity early in T2. Then it becomes low intensity as the blood clots and loses water. Back pain is the most common presentation. MRI is the diagnostic test of choice with or without gadolinium reported by the authors, whereas among the seven subarachnoid hematomas, three were continuous and four were skipped. Minor neurologic deficits developed in two of these seven and these were managed nonoperatively. The spontaneous epidural hematoma not associated with progressive or significant neurologic deficit can be managed nonoperatively, with reversal of any anticoagulation and serial monitoring being key factors. Most symptomatic subarachnoid hematomas can be surgically decompressed within 12 hours. Of all the epidural hematomas cases, 12 cases developed perioperatively, 7 from epidural catheters, 4 from vascular abnormalities in the epidural space, 4 from anticoagulation, 2 from trauma, and finally 2 spontaneous. All patients improved, but those treated after 12 hours had inconsistent improvements. The neurologic deficits were not further quantified in this retrospective review.
Coagulation studies should be ordered and corrected as needed with vitamin K and fresh frozen plasma. Patients receiving warfarin, aspirin, heparin, and/or its derivatives can experience this complication, especially if a laminectomy has been performed. Thrombocytopenia (especially heparin-induced) and other coagulopathies are well-documented risk factors for epidural hematoma.127 Due to the risk of epidural hematoma, routine administration of warfarin, heparin, or low-molecular-rate heparin is not routine prophylaxis, but low-dose aspirin (81 mg) may be used with low risk of epidural hematoma.127 Prevention of life-threatening consequences of pulmonary embolus is the most crucial issue of management of thromboembolic disease. Removable inferior vena cava (IVC) filters should be given preoperatively in high-risk cases or perioperative patients who develops venous thrombosis above the popliteal fossa area.116,311 Mechanical devices are unlikely to cause bleeding problems and are the current baseline prophylaxis for thromboembolic prevention in spinal surgery, as is early mobilization of the patient.300 These patients may present within hours or days with deteriorating neurologic symptoms with or without respiratory failure.
Treatment of an acute thromboembolic process, DVT, or pulmonary embolus must be done on a case-by-case basis weighing the risks and benefits of anticoagulation therapy and/or temporary vena cava filter placement. No absolute standard of care exists. Anecdotes suggest that restarting preoperative anticoagulation is probably safe within hours of surgery not involving exposure of neural elements, but no level I or II data exist as to resumption of warfarin or low-molecular-weight heparin in the postoperative period in cases requiring laminectomy or corpectomy. Epidural hematomas are associated with venous clot or hematoma formation, especially after anterior corpectomy, and are most likely to be seen in anterior cervical discectomy or corpectomy where anticoagulation medications or effects can exert neurologic pressure. Lee and colleagues reviewed two cases of epidural hematoma that developed immediately after corpectomy. Both were monitored with MEPs, which identified the neurologic change and allowed for early decompression, and no lasting neurologic deficit occurred. One was a 74-year-old male and the other, a 37-year-old female. A perioperative epidural hematoma was diagnosed by deterioration of the MEPs but not the SSEPs, which were both run after the closure was completed.322 The authors emphasize the use of MEPs as the more sensitive test to follow the normal or even slightly abnormal cord during anterior cervical surgery. This requires corpectomy because, as the authors noted, the degree of paralysis was severe and immediate early evacuation was crucial in returning cord function.
Spontaneous spinal epidural hematomas were reviewed in 330 cases, and their prognosis depends on the degree of deficit, level of the cord or cauda, and time to surgical decompression occurring within 36 hours.320,321,323 Incomplete neurologic deficits may be delayed in treatment up to 48 hours.130 Spinal epidural hematoma typically presents as severe back pain with or without radicular pain, and the thoracolumbar area is more involved than the cervical area. Except in cases of vascular malformations, the degree of pressure and compression were most important. In vascular cases, the extent of the arteriovenous malformations (AVMs) determined the volume of the bleed and subsequent amount of pressure induced (see Chapter 91).
Iliac Bone Graft Harvest
Iliac crest bone graft harvest is commonly required for arthrodesis of the cervical, thoracic, and lumbosacral spine.* Vascular injuries associated with this concurrent surgery most commonly involve the superior gluteal artery and vein in the sciatic notch.100 The incidence is low and underreported.325 Injury to these vessels is usually direct and bleeding can be profuse. This often occurs from aggressive deep subperiosteal exposure of the gluteus maximus muscle from the posterior third of the iliac crest at the sciatic notch. Lim et al. have reported on injury to the superior gluteal artery during harvest of a posterior iliac crest graft with a literature review.326 Management options include packing, direct repair, ligation, or preferably selective angiography and embolization. When possible, ligation is performed which requires further exposure of the vessels by resection of the bone around the sciatic notch or rarely by exposure within the pelvis.17 An unrecognized or irreparable superior gluteal vessel or irreparable vessel damage injury can best be managed by selective endovascular embolization techniques postoperatively.277,326 Partial injury of a vessel wall may result in an aneurysm described by Neo and associates in an elderly osteoporotic male following anterior tricortical iliac crest bone graft harvest involving the deep circumflex iliac artery.327 Selective endovascular embolization of the artery was required after direct repair and hematoma evacuation were unsuccessful. Understanding the vascular anatomic relationships associated with the iliac crest bone graft harvest technique and prevention of the vessel injury is clearly optimal to all other treatment options.
Indirect Vascular Injury
*References 120, 173, 192, 206, 212, 219, 222, 246, 248, 250, 324, 325.
Indirect vascular complications from positioning during spinal surgery are infrequent compared with those of peripheral nerves such as the ulnar nerve at the cubital tunnel or stretch of the brachial plexus (best prevented with upper extremity SSEPs).5,170,220 Vascular complications regarding the eye and retina have been reported with prone positioning in posterior spinal surgery.5,328,329 These include embolic disorders to the retina, as well as central retinal artery (CRA) occlusion and retinal vein thrombosis.328 Embolism of clot, plaque, or air is rarely reported.252 The clinical consequence of these vascular complications to the retina is blindness, which is both catastrophic and, most often, irreversible. Risk factors include (1) length of surgery; (2) elevated intraoperative blood loss; (3) hypotension, both from blood loss or planned especially using nitroprusside; and (4) direct ocular or periorbital pressure.328,329 Two types of ophthalmologic vascular events can occur. CRA occlusion is directly related to pressure on the eye, whereas PION is multifactorial with increased blood loss, prone position, and sustained hypotension being key risk factors. Preventative measures include eye protection, soft foam facial padding, managing interoperative hypotension, and a 20-degree reverse Trendelenburg positioning. If these complications occur, ophthalmologic evaluation and treatment are recommended. However, the prognosis for restoration of sight is dismal. Friedman and colleagues330 presented another rare vascular complication remote from the site of surgery—cerebellar hemorrhage (cortical blindness). One cases was associated with an intradural T9-T10 disc herniation, and the other had an L3-S1 laminectomy for spinal stenosis. Although the cause of this extremely rare complication is not known, the authors suggested that durotomy and CSF loss may have been factors. This should be kept in mind if unexplained, delayed neurologic deterioration occurs postoperatively. This condition has been reported in supine, prone, and seated positions. Also, there are several reports of concurrent lumbar and cervical stenosis in which paraparesis to paraplegia has occurred from extension of the neck while treating the lumbar stenosis in a prone position. Unfortunately, these complications are not limited to spinal surgery.331
Superior Mesenteric Artery Syndrome
Superior mesenteric artery syndrome (SMAS) still occurs with more than 1000 cases reported worldwide, estimating an incidence of 0.2% of deformity cases.332 There are two variants of SMAS: nutcracker syndrome and Wilkie syndrome. Nutcracker syndrome is a rare condition characterized by the entrapment of the left renal vein (LRV) between the superior mesenteric artery (SMA) and the aorta. Wilkie syndrome occurs in patients with extreme malnutrition and weight loss leading to SMAS. The exact cause of the SMAS is unknown, but this syndrome may occur with external compression in this emaciated patient group.333
SMAS or “cast syndrome” is a type of vascular complication in which the distal one third of the duodenum is compressed.334 The superior mesenteric artery classically branches directly anterior from the aorta at about the L1 level at an acute angle. This artery then crosses the distal third of the duodenum. Corrective deformity surgery as is commonly seen in scoliosis reduces the angle of the superior mesenteric artery directly compressing the duodenum (Fig. 96–33A).335 These patients present with an upper gastrointestinal bowel obstruction (Fig. 96–33B).335 This syndrome also has been described in adult paraplegics on a delayed basis or in adult hyperkyphotic corrections.336
A high index of suspicion is required to recognize this complication because most anterior spinal procedure has pain and at least some degree of ileus. Evaluation and diagnosis is usually established with abdominal films, CT scanning, or MRI. Differential diagnoses include (1) postoperative ileus, (2) a large bowel obstruction, and (3) Ogilvies syndrome (spastic or pseudo obstruction).337 Initial treatment should include a nasogastric tube (NG), restriction of oral intake, intravenous fluids, and electrolyte balance. These patients may benefit from positioning left side down with a slight Trendelenburg posture. Although the vast majority of cases resolve in 2 to 3 days with supportive measures, if the obstruction persists intravenous hyperalimentation should be provided to prevent malnutrition with its attendant risk of wound problems. In rare unresolving cases, a direct surgical decompression is necessary. If any external compressive device is present (i.e., cast or brace), this should be removed first. Surgical care would include a duodenojejunostomy and/or release of the ligament of Treitz as the treatment of choice, with gastrojejunostomy as an alternative.35
SMAS can affect adults with kyphosis but is primarily seen in pediatric deformity cases. Recently, a low BMI accompanied by the typical risk factor of a high degree of correction has been implicated as a key risk factor in the development of SMA. Those who developed an SMAS had a 17.5 BMI compared with those who did not at 21.7, and the percent correction was increased to 75.5% from 64.5%, respectively.336 Adult cases occur with significant corrections of kyphosis and have been reported as late as 24 days after the surgery.338 The treatment remains the same, including NG tube (an average of 10.2 days), no oral intake (NPO) status, and intravenous hyperalimentation.337,339
Peripheral Vascular Disease
End organ effects of vascular complications can be acute, as discussed previously. In reality, nerve and vascular structures are often paired anatomically and the effects of vascular disease are much more chronic (e.g., vascular disease associated with diabetes mellitus. Peripheral vascular disease, lumbar spinal stenosis, and cervical myeloradiculopathy are often seen in the same patient because they are degenerative conditions related to age (sixth decade on). It is well established that neurogenic claudication in the lumbar spine and cervical spondylotic myelopathy of the neck have a microvascular ischemic etiology.* The anterior spinal artery, supplying about 75% of the cord, is the chief vascular supply to the spinal cord.80 Chronic microvascular ischemia causes demyelination, nerve cell damage, and impaired axoplasmic flow.76 Sequelae are more likely to be evident in patients with underlying canal stenosis.340,341 Because atherosclerotic vascular disease and acquired spinal stenosis occur in the same age ranges, coexistence of the two disease processes is common.17 Rupture, leakage, or dissection of an aortic aneurysm may present with sensory and motor symptoms and signs on the basis of spinal cord or nerve root ischemia.340–342 It is beyond the scope of this chapter to discuss these in detail, but it seems appropriate and comprehensive to note these here. The same is true of vascular neoplasia such as vascular anomalies or arteriovenous malformations (see Chapters 41, 42, 62, 75, and 91).
Major Traumatic Vascular Injury (Polytrauma)
Vascular injury and complications can result from high-energy blunt trauma or penetrating objects.343 (See Chapter 82 for more information.) Reports include vertebral artery injury from cervical spine fractures, fracture dislocations, and penetrating trauma such as gunshot wounds. Vertebral artery occlusion occurs at a relatively high rate in cervical bilateral facet deformity and rarely recannulates. This is important in two scenarios: (1) If further cervical surgery is planned, all effects should be given to avoid the uninjured side and (2) there is an increased risk of late vascular sequelae such as aneurysm or fistula. Thoracic aortic lacerations can also result from fractures and fracture dislocations, as well as blunt trauma to the chest. For example, shear type fracture dislocations associated with diffuse idiopathic skeletal hyperostosis or ankylosing spondylolysis have been reported to directly shear or lacerate the tethered aorta.176 It is noteworthy that a fracture in ankylosing spondylitis has a high rate of epidural hematoma, which is the primary way that neurologic deterioration occurs in fragile and brittle spines. The lumbar aorta and vena cava are less likely to be involved in this mechanism because they are relatively more mobile.210 Mozingo and Denton343 present a case of abdominal aortic occlusion from blunt trauma in which the patient had acute peripheral nerve ischemia and paraparesis mimicking spinal cord trauma or a “transverse” spinal cord lesion.
Spinal cord ischemia is less likely in such lesions if they occur below the level of the renal arteries.201 Detail in the examination will help identify the lack of distal pulses but may be confused with spasm, specifically if the patient is hypovolemic. The injuries to these types are due to the close proximity to the vertebral artery to the cervical spine as it passes in the transverse foramen and the thoracic aorta as it is anteriorly tethered to the thoracic spine. Further review and discussion of these types of vascular injuries is beyond the scope of this chapter and is further pursued in the spinal trauma section (see Chapter 78). Choi and colleagues113 managed vertebral artery lesions with an endovascular covered stent. A myriad of adverse events occurred including three deaths, seven pericardial tamponades, one aortoduodenal fistula, seven pseudoaneurysms with secondary ischemia, two DVTs, and one carpal tunnel.
The vertebral artery in cervical spine trauma has been increasingly recognized and studied. This is most often associated with a fracture dislocation or rotatory subluxations. These occur at about 0.05% incidence including all trauma and 70% of cervical spine trauma. The treatment is often nonoperative with benign neglect and is certainly a reasonable way to go if there is no neurologic deficit, but spinal alignment and stability should be restored. Fassett and colleagues109 found a vascular injury rate with neurologic sequelae from 0% to 24%. The diagnosis is by cervical angiography or secondarily by MRA or magnetic resonance venogram (MRV). Both can be used as a noninvasive alternative treatment, are widely variable, and not defined by level I and II evidence-based medicine. Hoit and colleagues110 showed what they called blunt craniovertebral trauma in 69 patients. The most common injury was a basal skull fracture with neck hyperextension. The carotid artery was also monitored and quantified. Carotid artery injuries are more likely to lead to a cerebral vascular accident and are highly associated with facial fractures. Neural sequelae and/or vascular sequelae can result in a Wallenberg or lateral medullary syndrome with ischemic defects, CVA, and arterial hemorrhage. As discussed earlier, this is called “bow hunter syndrome” (a stroke produced by vertebral artery occlusion). Of the 69 cases observed by Fassett, 20 had vascular blunt injuries in which 3 carotid and 15 vertebral arteries were involved. The pathophysiology of the carotid artery and vertebral artery injury showed intimal dissections in 8 out of 28, pseudoaneurysm in 6 out of 28, and occlusion in 5 out of 28. Eight injuries occurred intracranially and had the worst prognosis, and 20 injuries occurred in the cervical region alone.
In contrast, Taneichi and colleagues’112 review of C1 trauma found a 7.2% rate of vertebral artery injury. In this series the primary cause of injury was a cervical fracture dislocation from C2 to C7. Three of the 11 injuries restored flow without treatment. Occlusion was rare, but it was much more common to see intimal dissection, especially with the fracture dislocation. All 11 cases, one bilaterally, were asymptomatic. Blunt head and neck trauma risks the vertebral artery, especially if there is any translation or rotation of the vertebral artery containing segments C2 to C6. Lesions may be spasmodic, and they may be dissections, lacerations, and occlusions. These are best controlled by rapid reduction of the cervical spine. If there is a noninvasive standard for studying the artery, MRA is probably the best choice. Clearly, if asymptomatic, one would do nothing. If the artery is occluded and symptomatic, it can be restored either through open surgery or more likely through the newer endovascular techniques for opening an occluded or damaged vessel. Clinical results in symptomatic patients depend on the rate at which the cervical spine can be reduced and the time of ischemia.
DiFabio did a large inclusive review of 116 articles regarding vertebral artery injury. The most common injury was an arterial dissection followed by a basilar skull injury followed by a lateral medullary syndrome. Two percent of vertebral arteries were injured from physical therapy manipulation. Overall morbidity in the literature is 10%.114 There is some question about preoperative testing and whether there are any physical warning signs. One such warning sign or preoperative possible predictive physical examination test is to have the patient maximally externally rotate to the right and left for 30 seconds. If the patient does not develop symptoms, then a forward thrust of the neck with repeat of the rotation for 30 seconds is recommended. If no symptoms develop with these two maneuvers, then, in theory, the vertebral artery is patent and proximal flow is normal.
Conclusions
As Inamasu and Guiot stated, anterior lumbar arterial and venous injury is under-reported and, given the usual publication lag of 1 to 3 years, the vascular complications of lumbar spinal surgery from reconstruction, deformity, and arthroplasty or fusion have correlated with increased adverse events and complications.39 This probably started to occur about 1990 but just got into the literature around 1995 because of that publication lag. Occlusion of the left common iliac artery is probably one of the worst complications to develop from anterior lumbar spinal surgery because it is difficult to diagnose. It presents initially with neurologic deficits, and slowly vascular manifestations are clearer. It can be mimicked by spasm, and if the ischemia is due to a complete block, rhabdomyolysis can occur and loss of limb and/or life will follow (reperfusion syndrome) (see Table 96–5). Uncontrolled bleeding from any large venous vessel such as the vena cava, common iliac vein, or recurrent iliolumbar vein can be fatal if uncontrolled. As shown by Brau, if bleeding is uncontrollable, ligation of the vena cava is an option but leaves the patient with difficult-to-control chronic lower extremity edema.260
Pearls
Pitfalls
Key Points
1 Baker JE, Reardon PR, Reardon MJ, Heggeness MJ. Vascular Injury in Anterior Lumbar Surgery. Spine. 1993;18:2227-2230.
2 DeSaussure RL. Vascular Injury Coincidence to Disc Surgery. J Neuro. 1959;16:222-229.
3 Goodkin LL, Laska LL. Vascular and visceral injuries associated with lumbar disc surgery: medicolegal implications. Surg Neurol. 1998;49:358-372.
4 Pfeifer BA, Friedberg SR, Jewell ER. Repair of Injured Vertebral Artery in Anterior Cervical Procedures. Spine. 1994;19:1471-1474.
5 Smith MD, Emery SE, Dudley A, et al. Vertebral artery injury during anterior decompression of the cervical spine. J Bone Joint Surg. 1993;75-BM:410-415.

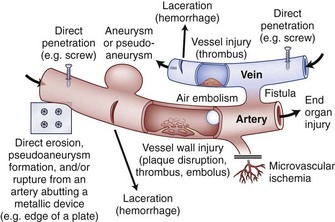
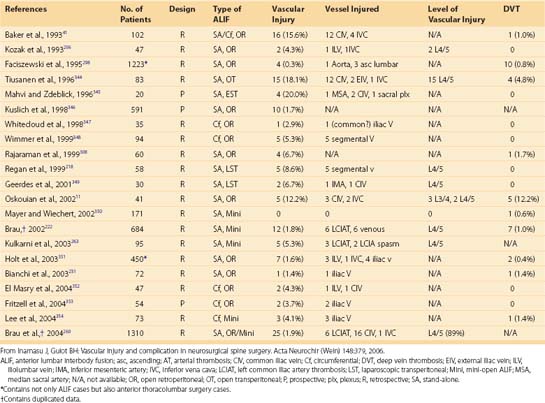
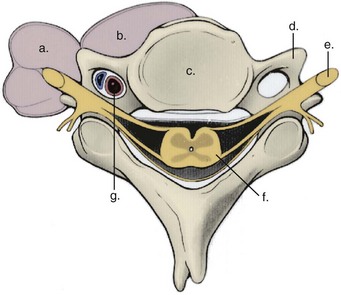
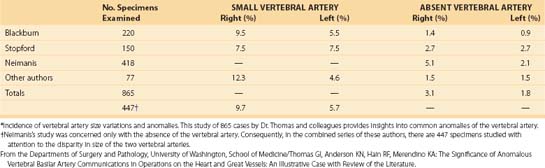
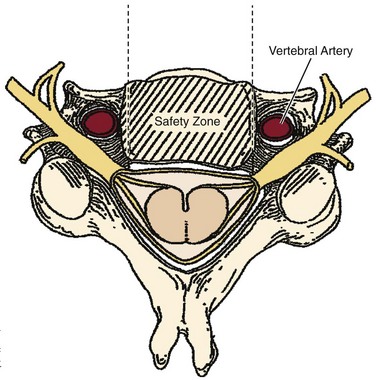
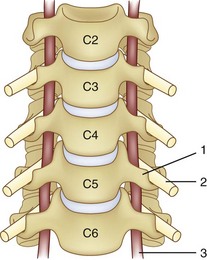
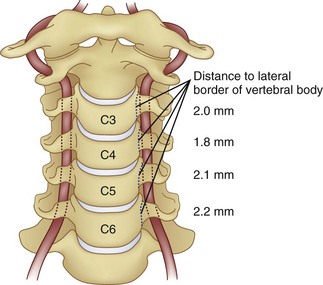
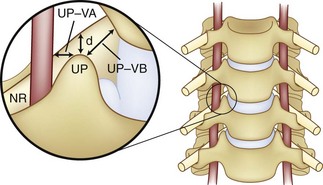

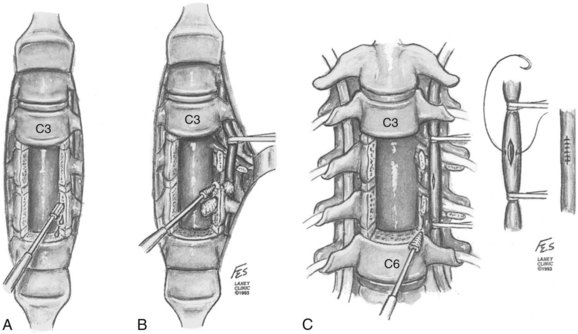
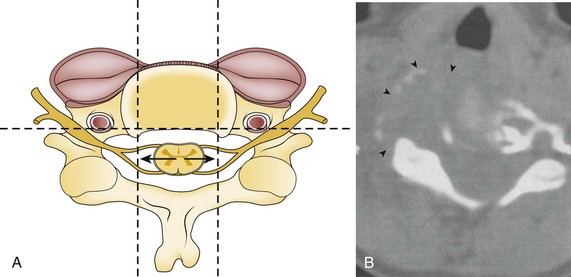
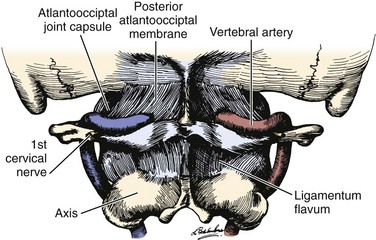
 to 2 cm from the midline.
to 2 cm from the midline.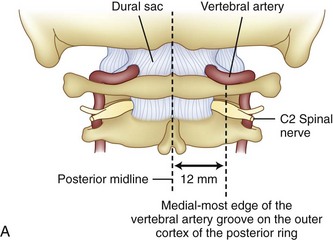
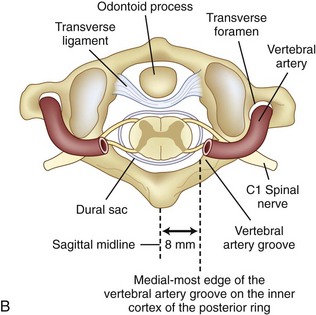

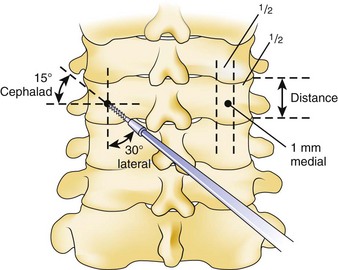

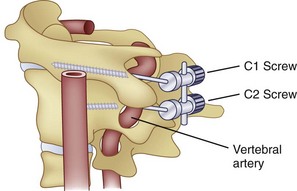
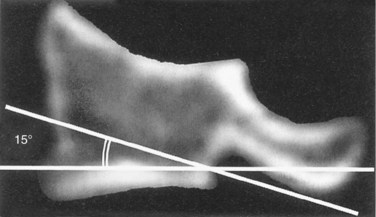
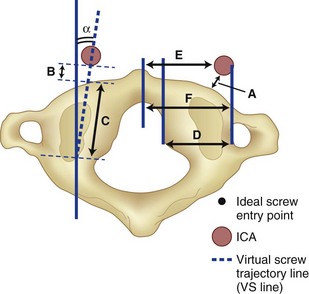
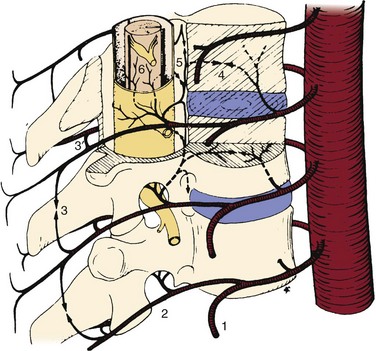
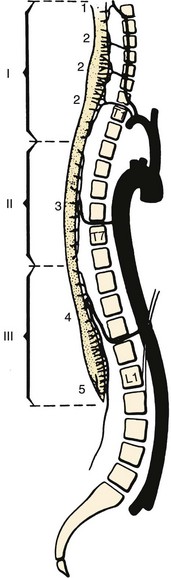
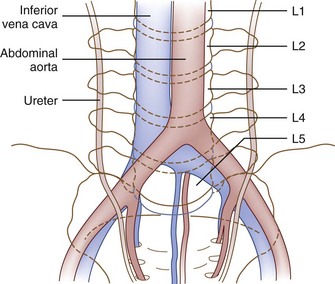
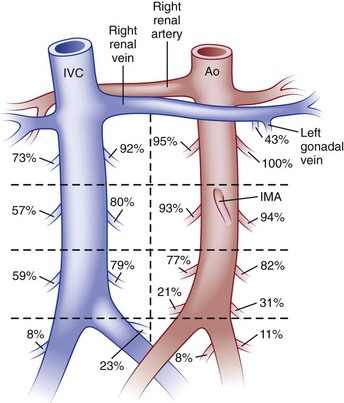
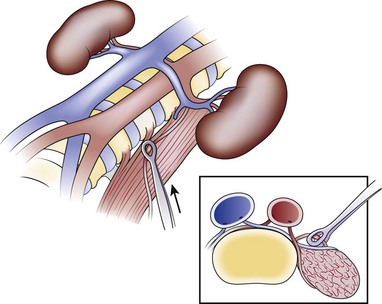
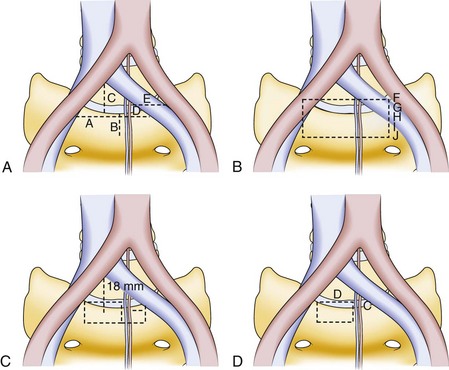
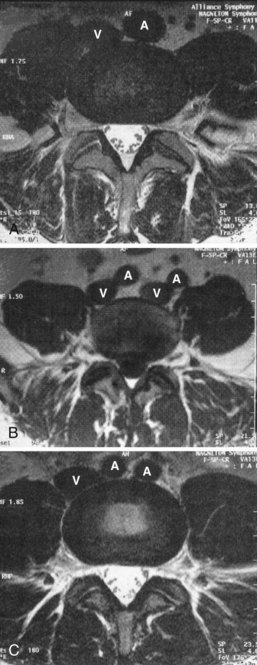
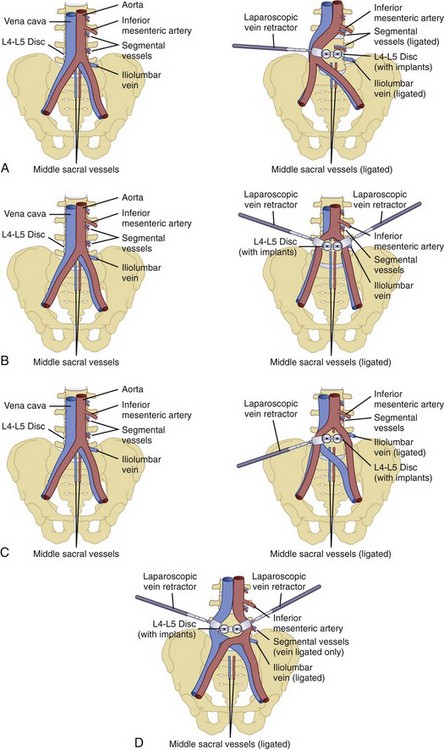
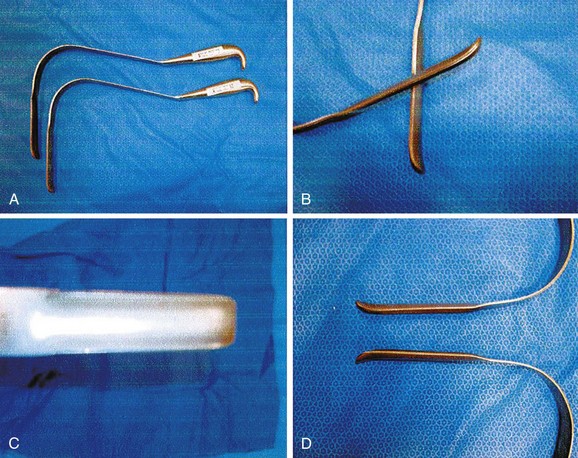
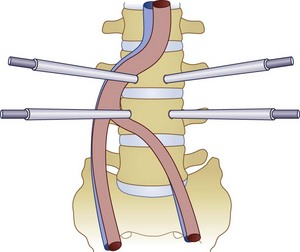
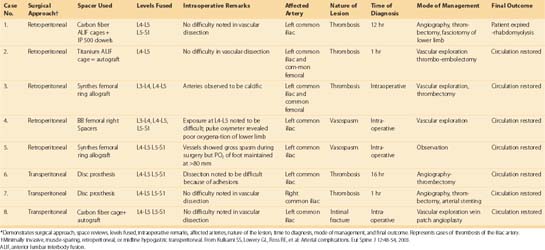
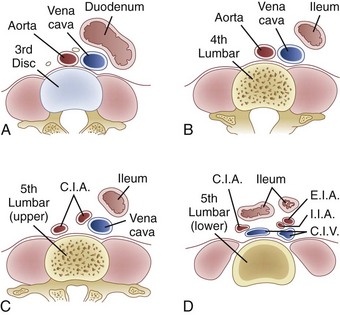
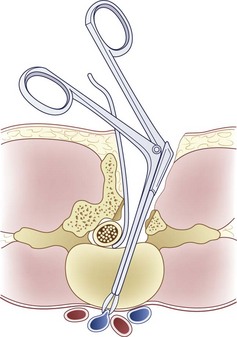
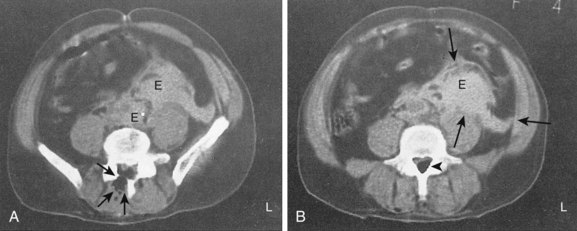
 ) between cava and aorta (E). Hematoma is infiltrating the caudal part of the pararenal space.→, air in the muscular tissue;
) between cava and aorta (E). Hematoma is infiltrating the caudal part of the pararenal space.→, air in the muscular tissue;  , air in the spinal canal at the hemilaminectomy site, as a result of the recent surgical treatment (30 minutes).
, air in the spinal canal at the hemilaminectomy site, as a result of the recent surgical treatment (30 minutes).