Chapter 4 Valvular heart disease
Introduction
Cine imaging using SSFP and velocity mapping sequences are the cornerstone of CMR valvular assessment. Breath-hold high-resolution FSE can be useful for valve morphology and developments such as moving slice velocity mapping and real-time imaging will improve evaluation in the near future. CMR reporting in valvular heart disease generally includes:
Aortic stenosis
AS has a long asymptomatic period after which clinical symptoms such as angina, exertional dyspnoea and effort syncope may result. Since symptoms develop late in the pathophysiology of AS, clinical deterioration soon follows if valve replacement is not undertaken. Obstruction to the LVOT leads to elevated LV pressures and compensatory LVH which initially maintains cardiac output and reduces LV wall stress, but ultimately decreases LV compliance and increases end-diastolic pressure. Increased myocardial oxygen demand causes myocardial ischaemia and later LV failure.
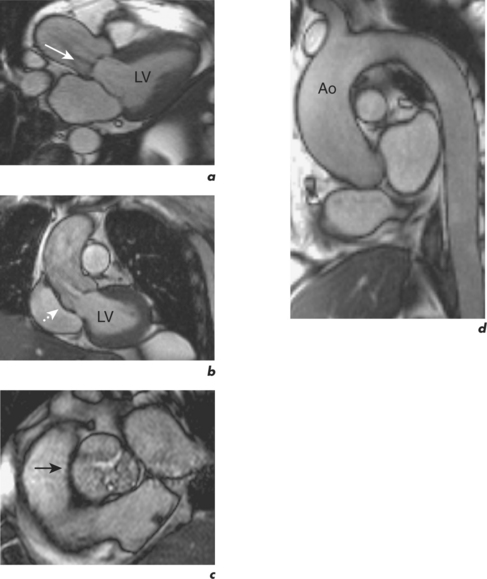
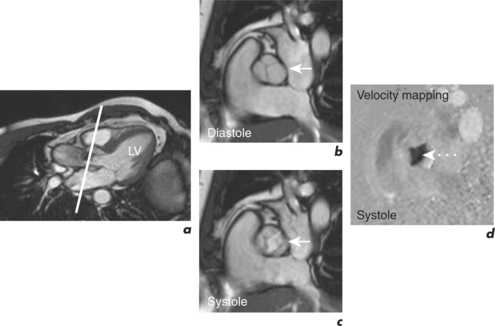
CMR is a robust method of calculating the severity of AS and correlates well with continuous wave Doppler echocardiography. However, it is far superior to echocardiography in identifying the cardiovascular functional and morphological sequelae of AS, such as post-stenotic dilatation of the ascending aorta, degree of LVH, and myocardial viability (Figures 4.1 and 4.2). These are important factors in the assessment of patients prior to valve replacement surgery, which often includes CABG and aortic root replacement. CMR also provides an excellent modality for serial surveillance of parameters such as LV function, volumes and mass in patients under follow-up and post operatively. This is done using the pre-contrast part of the protocol outlined in Chapter 1. Cines can demonstrate thickening and bulging of the aortic cusps and turbulent flow in the aorta. Imaging in an oblique sagittal plane parallel to the valve may demonstrate restricted opening and closure of the valve, and is frequently satisfactory for direct planimetry of the valve orifice and evaluation of bicuspid valve morphology. Direct planimetry can be performed using cine imaging or velocity mapping sequences (Figure 4.3).
Velocity mapping is primarily used, however, to calculate the pressure gradient across the AV using the modified Bernoulli equation;
where ΔP (mmHg) is the pressure drop across the stenosis, and Vmax is the peak velocity (m/s) determined by velocity mapping 1 to 1.5 cm above and parallel to the valve plane (Figure 4.3d). The typical Venc setting for the LVOT is 2 m/s, and 2.5 to 4 m/s for the aorta. An initial Venc of 2.5 m/s is often used and adjusted upwards if there is velocity aliasing (Figure 1.3). The velocity of blood flow through the AV is greater than that through the MV.
Severity of AS is graded as: mild >1.5 cm2, moderate 1.0–1.5 cm2, severe <1.0 cm2, and critical <0.8 cm2. In severe AS, the peak transvalvular gradient is usually >50 mmHg.
Aortic regurgitation
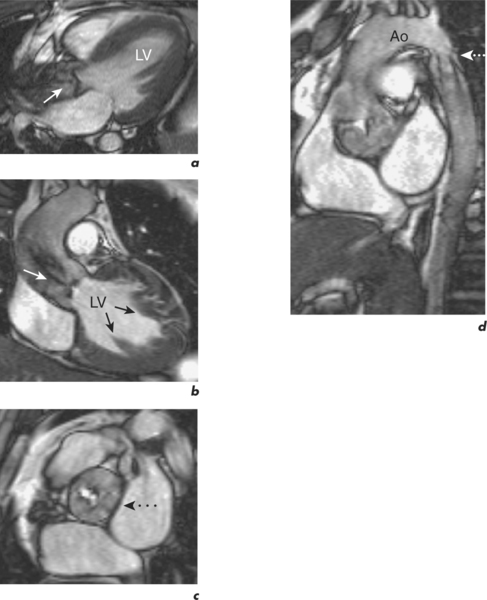
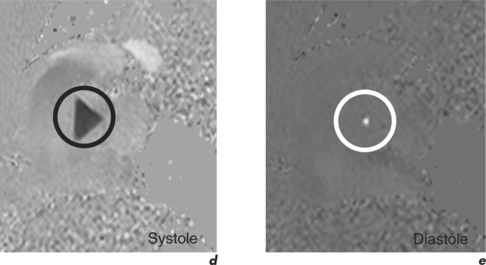
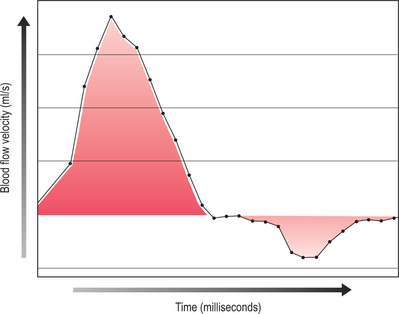
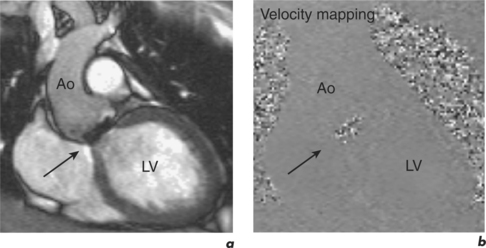
Cines in the LVOT plane demonstrate the flow void due to the regurgitant jet which can be qualitatively assessed by the size of the jet, after taking into account the effects of echo time (Figure 4.4a). Velocity mapping is performed in a plane perpendicular to the AV positioned just above the valve but below the coronary ostia (Figures 4.4b–c). This plane optimally demonstrates forward and regurgitant flow and can further characterize the morphology of the valve. The regurgitant fraction is then calculated by graphing the flow volume curve using dedicated software (Figures 4.4d–e). The area under the curve below zero in diastole represents the regurgitant volume and the regurgitant fraction is calculated by dividing this into the forward SV in systole (Figure 4.5). An alternative method is to calculate the aortic flow and pulmonary flow at a level just above the respective valve planes. The difference in forward flow provides an estimate of the degree of AR in single-valve disease, as does the quantitative difference between RV and LVSV. The degree of ventricular dilatation also helps to qualitatively assess the severity of regurgitation. In the presence of dilatation, LGE imaging is performed to look for myocardial fibrosis, and this is especially useful in the preoperative setting.
Specific CMR reporting points for AR include:
Mitral stenosis
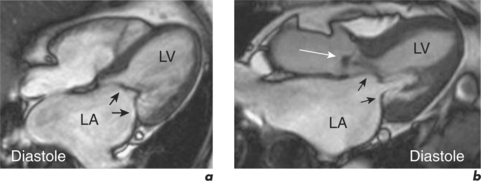
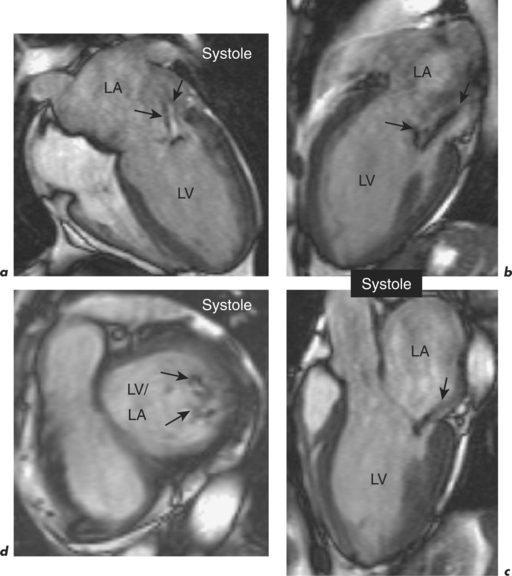
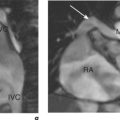
CMR complements echocardiographic evaluation of MS, especially in patients with poor acoustic windows. Cines taken in the four-chamber, two-chamber and LVOT views demonstrate the thickened, hypokinetic and domed MV leaflets and a signal void arising from the MV in diastole extending into the LV (Figure 4.6). The LA is usually enlarged in moderate to severe stenosis and this is easily visualized. Additionally, the pulmonary trunk may be enlarged and tricuspid regurgitation (TR) may be present in cases with pulmonary arterial hypertension. This can be assessed in more detail by reviewing the four-chamber cine and acquiring an RVOT cine view, while a preliminary appraisal of the pulmonary arteries is readily made with the transaxial FSE acquisition. SSFP cines or velocity mapping performed in a plane parallel to the MV can be performed for direct planimetry of the stenotic valve orifice, although these can be limited by motion of the valve through the fixed imaging plane (Figure 4.7). Calculation of the valve area by direct planimetry correlates well with echocardiographic and cardiac catheterization data, but may slightly overestimate measurements obtained by these modalities.
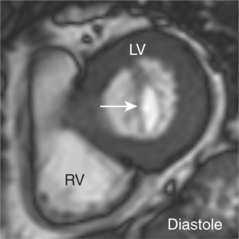
Figure 4.7 SSFP cine image performed in a plane parallel to the MV (white arrow) from the case illustrated in Figure 4.6. Direct planimetry revealed a valve area of 1.8 cm3.
Severity of MS is graded as: mild ≥1.5 cm2, moderate 1.0–1.5 cm2, and severe <1.0 cm2.
Mitral regurgitation
MR can be caused by abnormalities of the MV leaflets (myxomatous degeneration (Figure 4.8), rheumatic disease, endocarditis, parachute MV), chordae tendineae (myxomatous or traumatic chordal rupture, endocarditis), papillary muscle (acute infarction) or annulus (annular dilatation, periannular calcification). Chronic MR produces LA and LV dilatation due to increased SV. Pulmonary venous hypertension may be present but is usually less severe than with MS, and pulmonary arterial hypertension is also less common. Acute MR causes pulmonary venous hypertension which may be asymmetrical (right upper lobe) without atrial or ventricular enlargement.
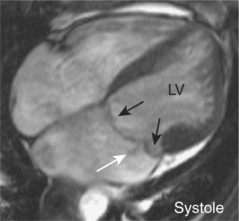
Cines in the four-chamber, two-chamber and LVOT views demonstrate the signal void from the regurgitant jet. The jet may be central in annular dilatation or eccentric in valve leaflet, chordae tendineae or papillary muscle dysfunction. Multiple or complex jets may be present (Figure 4.9). Qualitative assessment of the severity of regurgitation can be performed by the size of the jet (accounting for the echo time) and the degree of LA dilatation. Quantification of regurgitant fraction can be performed in several ways along lines similar to that already described with AR. MR secondary to central, uncomplicated jets can be quantified by prescribing a region of interest with velocity mapping CMR using a plane placed en-face and just distal to the valve. This plane can also be used to measure effective regurgitant orifice area. A method in single regurgitant lesions is via determination of the difference in LVSV with either flow in the proximal ascending aorta or MPA, or the RVSV if no right-sided regurgitation is present.
Other valve lesions
Mixed valvular disease is often present, particular in rheumatic heart disease which principally involves the MV and less commonly the AV. In late disease with pulmonary arterial hypertension, TR is also present. CMR quantification of regurgitant fractions can become complicated in this setting but is possible using velocity mapping at the individual valve planes and generating several flow velocity time curves for evaluation in comparison with LVSV and RVSV. Valve planimetry of the mitral and aortic valves can also be undertaken to yield values for an effective regurgitant orifice (Table 4.1). As with echocardiography, all available indicators of severity must be assessed collectively prior to documenting final conclusions on the clinical report.
Table 4.1 Grading of severity by effective regurgitant orifice (mm2)
| Severity | MR | AR |
|---|---|---|
| Mild | <20 | <10 |
| Mild to moderate | 20–29 | 10–19 |
| Moderate to severe | 30–39 | 20–29 |
| Severe | >40 | >30 |
CMR is also useful in quantifying the degree of TR, pulmonary regurgitation (PR) and pulmonary stenosis (PS). Its multiplanar capability is useful in the assessment of global RV function which may be limited using echocardiography.
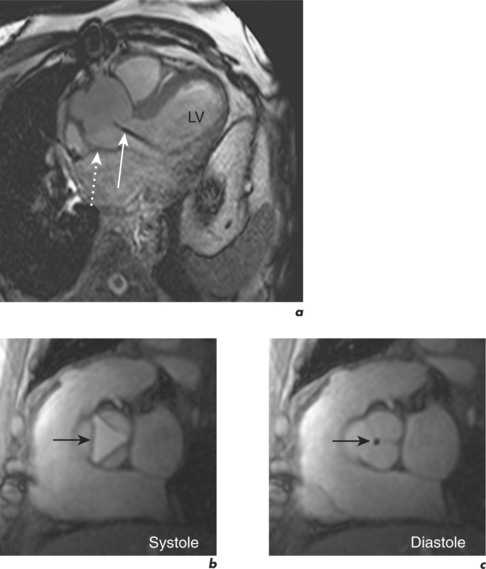
Metallic prosthetic valves are safely imaged with CMR. Although assessment of paravalvular abscesses or quantification of regurgitant lesions can be performed, results may be markedly hindered by metal artefact and conclusions should therefore be interpreted within this context (Figure 4.10). FSE sequences are less affected in the presence of metal than SSFP cine or velocity mapping CMR.