Vaginoplasty With Perineal Reconstruction (Cosmetic Gynecologic Surgery)
The term vaginoplasty has been used to describe any reconstructive procedures performed on the vagina. This chapter specifically addresses the use of vaginoplasty with perineal reconstruction to tighten the introitus and vaginal lumen or to reconstruct the perineum for aesthetic or functional reasons.
Vaginoplasty often includes anterior and/or posterior colporrhaphy, in which portions of the mucosa are excised and the vaginal lumen and introitus are reconstructed. Unfortunately, no standardization for these types of procedures currently exists. The goal of all reconstructive procedures performed on the vagina should be to create a well-supported vagina of appropriate length and caliber. The axis of the vagina should not be deviated, with the vaginal vault having a slightly posterior direction toward the hollow of the sacrum. At the completion of any repair, the vaginal lumen should easily accept two fingers, and the posterior vaginal wall and perineum should have a perpendicular relationship. This usually is best accomplished by removing a diamond-shaped piece of tissue from the perineum and the posterior vaginal wall (Fig. 103–1). Every repair needs to be individualized to the patient’s specific anatomy.
Figs. 103–2 through 103–5 provide examples of a variety of patients undergoing vaginoplasty and perineal reconstruction. Fig. 103–2 shows a patient with a symptomatic rectocele and dyspareunia secondary to a large buildup of the skin of the labia minora at the level of the introitus. Note that the completed repair re-creates an appropriate relationship between the perineum and posterior vaginal wall while creating posterior vaginal wall support and decreasing vaginal caliber. Fig. 103–3 presents a patient with a widened genital hiatus, as well as a perineal defect. Figs. 103–4 and 103–5 both show young patients who required extensive perineal reconstruction after vaginal birth. In both cases, a xenograft (Surgisis; Cook Medical, Bloomington, Indiana) is used to fill in a perineal skin defect.
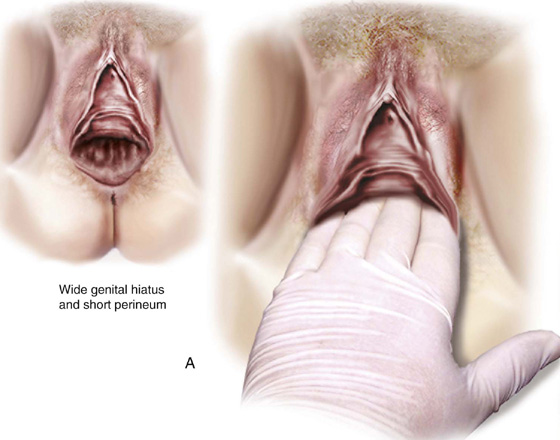
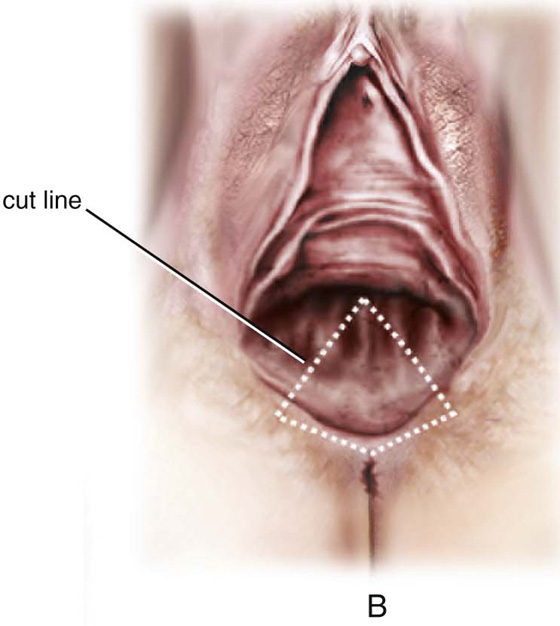
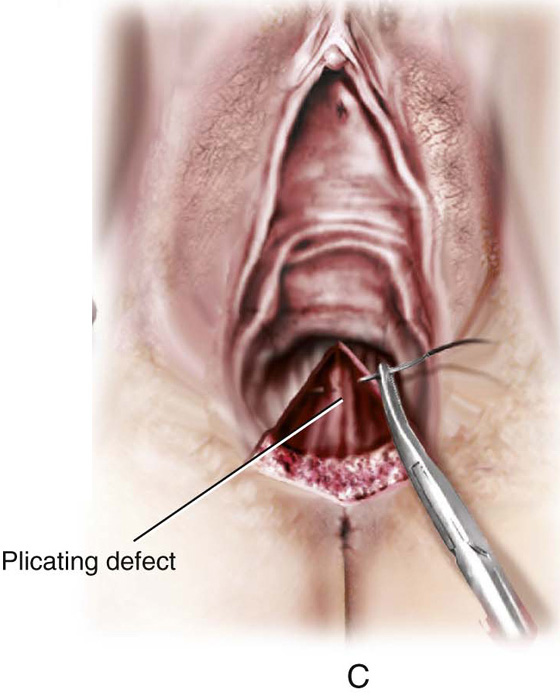
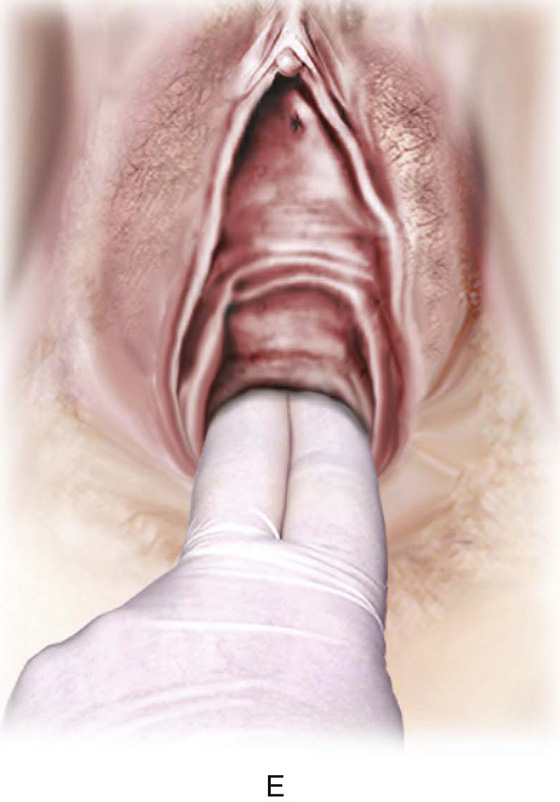
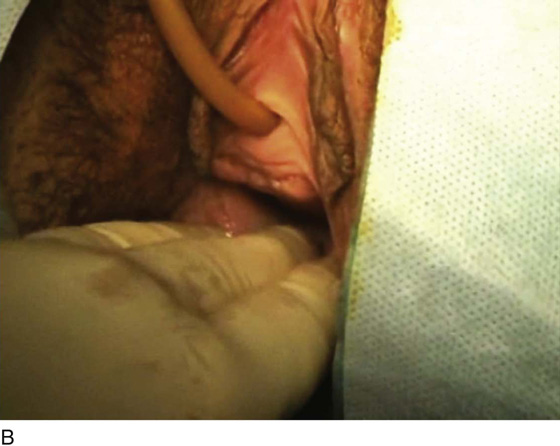
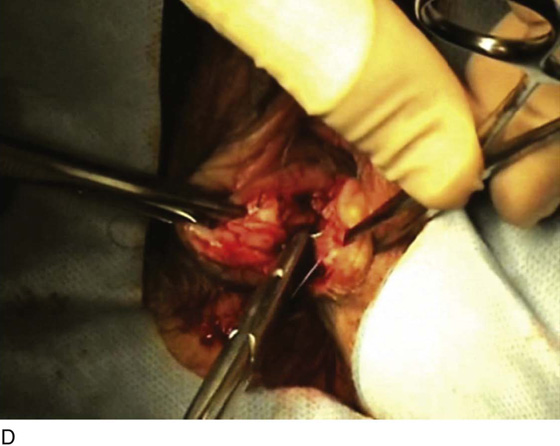
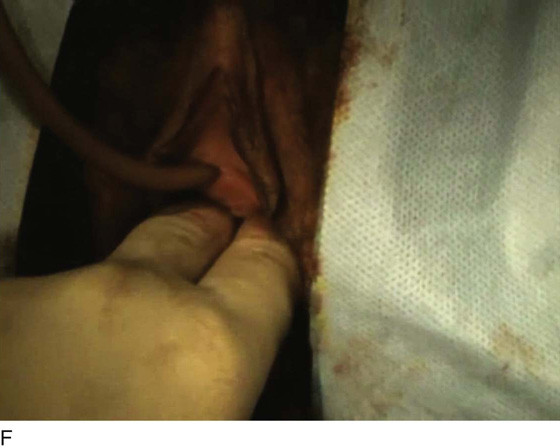
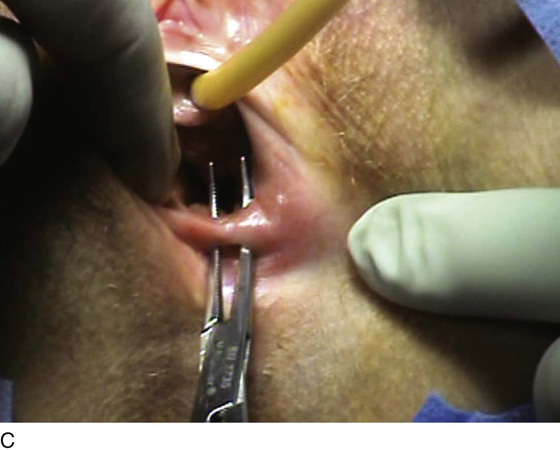
FIGURE 103–1 Technique of vaginoplasty and perineal reconstruction with the sole aim of tightening the vaginal introitus. A. Note the wide genital hiatus, which easily allows the insertion of four fingers. B. A diamond-shaped piece of tissue to be excised is marked. C. The tissue has been removed, and deep stitches are taken through the perirectal fascia and levator muscles to build up the posterior vaginal wall. Great care is taken to avoid the creation of a posterior vaginal wall ridge. D. The upper portion of the posterior vaginal wall is closed in preparation for perineal reconstruction. E. After perineal reconstruction, the introitus allows the insertion of only two fingers. F. Completed repair; note the perpendicular relationship between the posterior vaginal wall and the perineum.
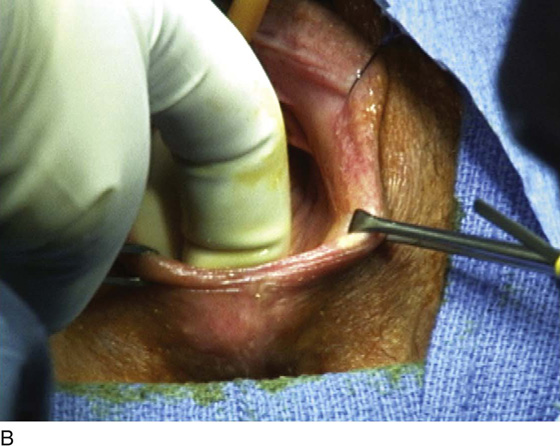
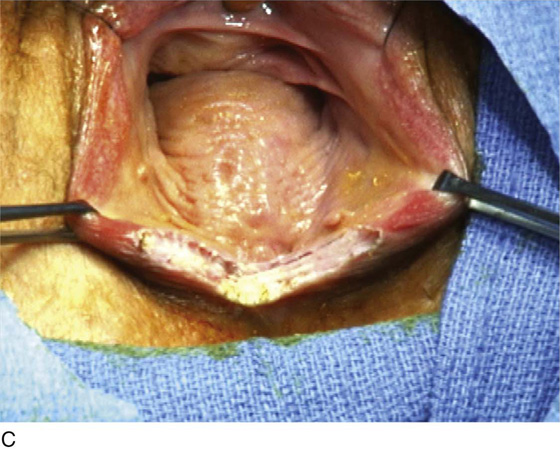
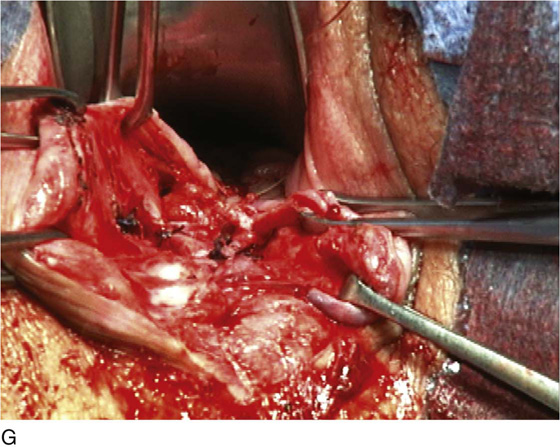
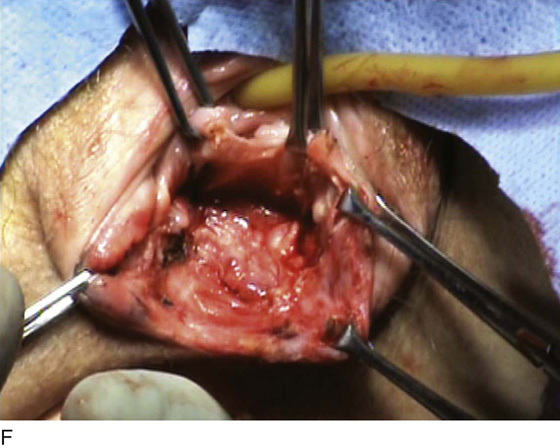
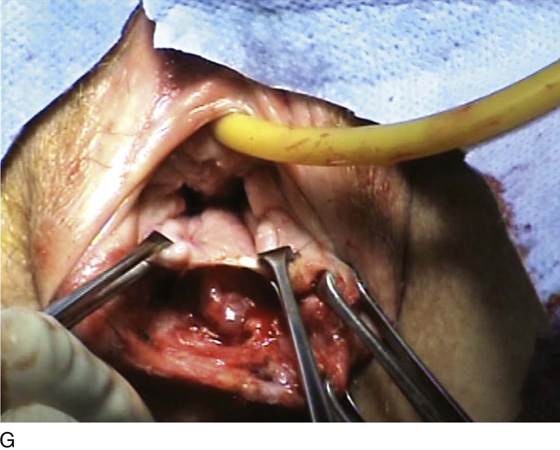
FIGURE 103–2 A. A patient with a large symptomatic posterior vaginal wall defect who also complains of dyspareunia secondary to an aggressive buildup of perineal skin. B. The skin of the labia minora has been previously sewn across the midline, most likely at the time of repair of a midline episiotomy. C. A longitudinal incision is made in the midline, taking down the built-up perineal skin. D. Sharp dissection is used to separate the distal posterior vaginal wall from the perineal muscles. E. The dissection is extended cephalad with removal of a midline tongue of vaginal mucosa. F. The dissection is extended to the pre-peritoneal space of the posterior cul-de-sac. G. A vaginal rectocele and enterocele have been performed, and the upper portion of the vaginal wall incision has been closed. H. The perineal body has been reconstructed and the vaginal introitus tightened. Note the perpendicular relationship between the perineum and the posterior vaginal wall.
FIGURE 103–3 A. Patient with a widened genital hiatus and a small perineal defect. B. Note that the vaginal opening easily allows three fingers. C. A diamond-shaped piece of tissue is removed from the perineum and the posterior vaginal wall. D. Deep 2-0 absorbable sutures are placed to close off the defect, thus decreasing the vaginal caliber. E. The vaginal and perineal incisions have been closed using a fine delayed absorbable suture. F. Note after completion of the repair that the introitus allows only two fingers. G. Completed repair 6 weeks postoperatively.
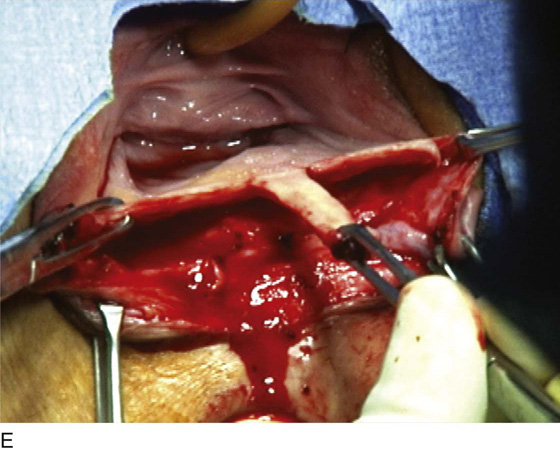
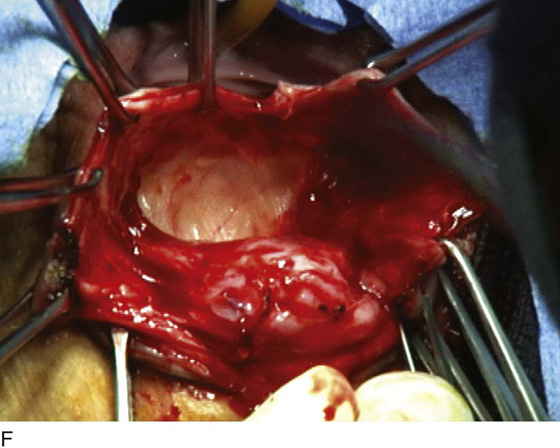
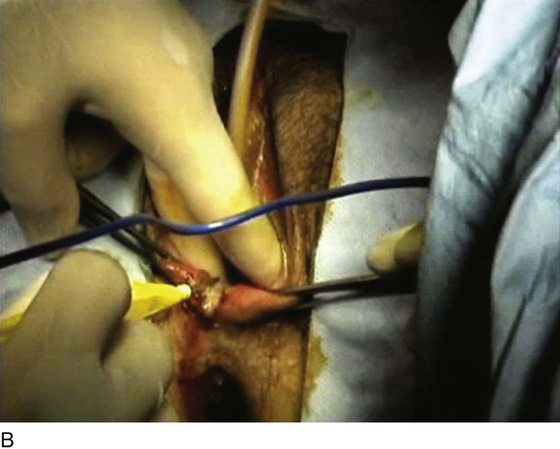
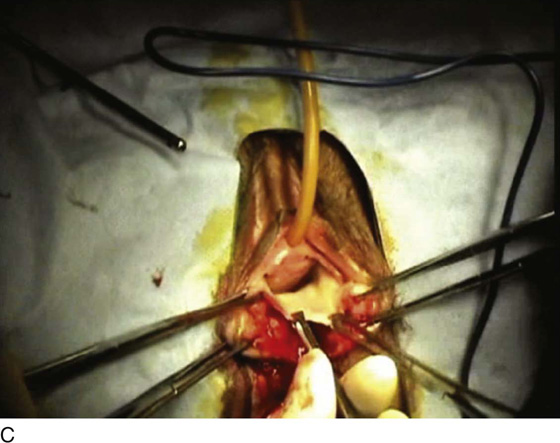
FIGURE 103–4 A. A young patient with a nonfunctional vagina secondary to a very tight introitus after an overaggressive repair of a midline episiotomy. B. Monopolar cautery is used to take down perineal construction at the midline. C. Sharp dissection is used to mobilize the posterior vaginal wall off the anterior wall of the rectum to allow for a vaginal advancement procedure. D. The incision has been closed transversely with interrupted delayed absorbable sutures. A defect in the perineal skin has been covered with a piece of Surgisis (Cook Medical).
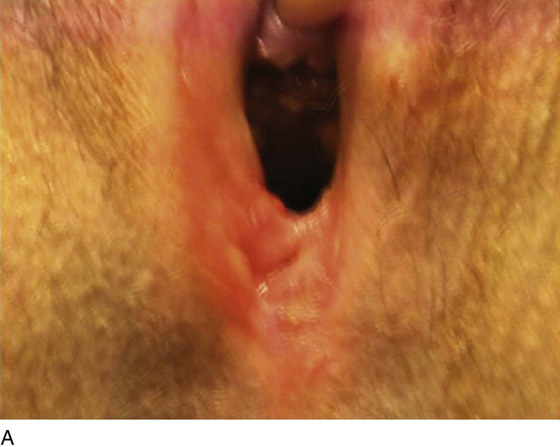
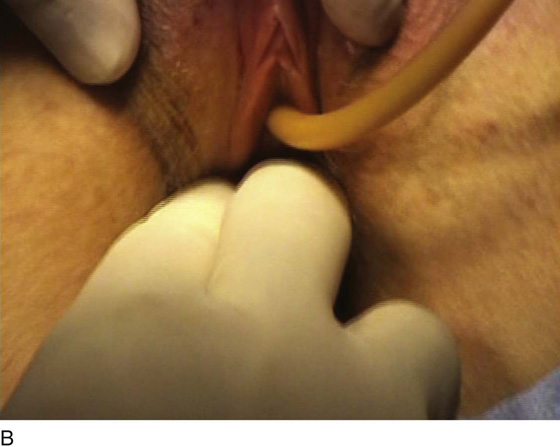
FIGURE 103–5 A. A young patient with excessive perineal scarring after repair of a perineal laceration. B. The introitus is noted to be very tight, allowing the insertion of only one finger. C. Band of perineal scar tissue. D. The area of perineal skin to be excised is marked. E. Perineal skin has been excised; note the extent of scar tissue. F. Scar tissue has been removed, and the posterior vaginal wall has been dissected off the anterior wall of the rectum. G. The posterior vaginal wall has been mobilized in preparation for vaginal advancement. H. The lateral edges of the vagina are successfully advanced, leaving a large defect in the perineal skin. I. A patch of Surgisis (Cook Medical) is sutured to the edges of the defect. J. The completed repair easily allows the insertion of two fingers. K. Completed repair 3 months postoperatively. Note successful conversion of the Surgisis to what appears to be normal perineal skin.