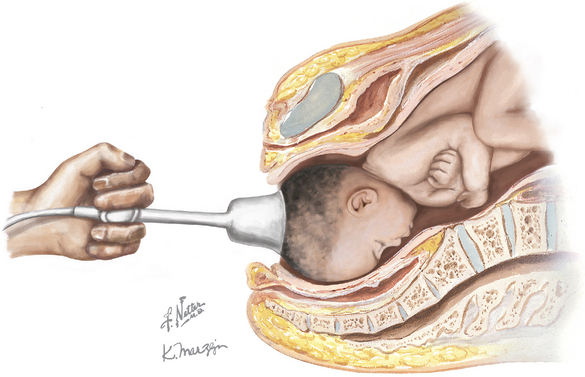
Chapter 254 Vacuum-Assisted Delivery
COMPLICATIONS
It is difficult (if not impossible) to separate the effects of vacuum-aided vaginal delivery from those of spontaneous vaginal delivery. Randomized trials and meta-analysis studies have failed to show conclusive differences. Both forceps delivery and vacuum extraction have been associated with the development of maternal hematomas and possibly linked to pelvic floor injury. However, other factors associated with pelvic floor injury include normal spontaneous vaginal delivery, episiotomy, prolonged second stage of labor, and increased fetal size. Similarly, studies have failed to identify neonatal or fetal injuries or developmental abnormalities that can be directly linked to vacuum-assisted delivery. Fetal scalp lacerations, cephalohematoma (14% to 16%), subgaleal (subaponeurotic) hematoma (26 to 45 per 1000), intracranial hemorrhage, hyperbilirubinemia, and retinal hemorrhage are all possible. The higher rates of neonatal jaundice associated with vacuum delivery may be related to the higher rate of cephalohematoma. Overall, the incidence of serious complications with vacuum extraction is approximately 5%.
CPT CODE(S)
Carmody F, Grant A, Mutch L, et al. Follow up of babies delivered in a randomized controlled comparison of vacuum extraction and forceps delivery. Acta Obstet Gynecol Scand. 1986;65:763.
Chenoy R, Johanson R. A randomized prospective study comparing delivery with metal and silicone rubber vacuum extractor cups. Br J Obstet Gynaecol. 1992;99:360.
Cohn M, Barclay C, Fraser R, et al. A multicentre randomized trial comparing delivery with a silicone rubber cup and rigid metal vacuum extractor cups. Br J Obstet Gynaecol. 1989;96:545.
Hofmeyr GJ, Gobetz L, Sonnendecker EW, Turner MJ. New design rigid and soft vacuum extractor cups: a preliminary comparison of traction forces. Br J Obstet Gynaecol. 1990;97:681.
Kuit JA, Eppinga HG, Wallenburg HC, Huikeshoven FJ. A randomized comparison of vacuum extraction delivery with a rigid and a pliable cup. Obstet Gynecol. 1993;82:280.
Vacca A, Grant A, Wyatt G, Chalmers I. Portsmouth operative delivery trial: a comparison of vacuum extraction and forceps delivery. Br J Obstet Gynaecol. 1983;90:1107.
Williams MC, Knuppel RA, O’Brien WF, et al. A randomized comparison of assisted vaginal delivery by obstetric forceps and polyethylene vacuum cup. Obstet Gynecol. 1991;78:789.
Johanson R, Menon V. Soft versus rigid vacuum extractor cups for assisted vaginal delivery. Cochrane Database Syst Rev. 2000. CD000446.
Johanson RB, Menon BKV. Vacuum extraction versus forceps for assisted vaginal delivery (Cochrane Review). In: The Cochrane Library, Issue 4. Oxford: Update Software; 1999.
Lim FT, Holm JP, Schuitemaker NW, et al. Stepwise compared with rapid application of vacuum in ventouse extraction procedures. Br J Obstet Gynaecol. 1997;104:33.
Ngan HY, Miu P, Ko L, Ma HK. Long-term neurological sequelae following vacuum extractor delivery. Aust N Z J Obstet Gynaecol. 1990;30:111.
Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709.
American College of Obstetricians and Gynecologists. Operative vaginal delivery. ACOG Practice Bulletin 17. Washington, DC: ACOG, 2000.
American College of Obstetricians and Gynecologists. Vaginal birth after previous cesarean delivery. ACOG Practice Bulletin 54. Obstet Gynecol. 2004;104:203.
Cunningham FG, Gant NF, Leveno KJ, et al, editors Williams Obstetrics 21st ed. 2001 McGraw-Hill New York 503