V
Vacuum insulated evaporator (VIE). Container for storage of liquid O2 and maintenance of piped gas supply. An outer carbon steel shell is separated by a vacuum from an inner stainless steel shell, which contains O2. The inner temperature varies between −160 and −180°C, at a pressure of 7–10 bar. Gaseous O2 is withdrawn and heated to ambient temperature (and thus expanded) as required (Fig. 161); a pressure regulator distal to the superheater prevents pipeline pressure from exceeding 4.1 bar. If pressure within the container falls due to high demand, liquid O2 may be withdrawn, vaporised in an evaporator and returned to the system, restoring working pressure. If passage of heat across the insulation causes vaporisation of liquid O2 and a rise in pressure, gas is allowed to escape through a safety valve. The contents are indicated by a weighing device incorporated into the chamber’s supports.
Howells RS (1980). Anaesthesia; 35: 676–98
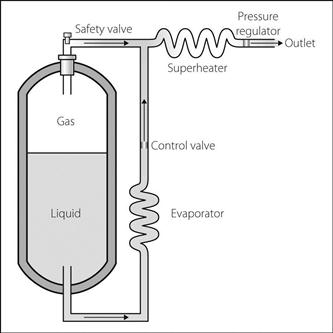
Fig. 161 Vacuum insulated evaporator
Vagus nerve. Tenth cranial nerve. Arises in the medulla from the:
 dorsal nucleus of the vagus (parasympathetic).
dorsal nucleus of the vagus (parasympathetic).
 nucleus ambiguus (motor fibres to laryngeal, pharyngeal and palatal muscles).
nucleus ambiguus (motor fibres to laryngeal, pharyngeal and palatal muscles).
 nucleus of the tractus solitarius (sensory fibres from the larynx, pharynx, GIT, heart and lungs, including taste fibres from the valleculae).
nucleus of the tractus solitarius (sensory fibres from the larynx, pharynx, GIT, heart and lungs, including taste fibres from the valleculae).
Leaves the medulla between the olive and inferior cerebellar peduncle, and passes through the jugular foramen of the skull. Descends in the neck within the carotid sheath between the internal jugular vein and internal/common carotid arteries (see Fig. 113; Neck, cross-sectional anatomy, and Fig. 104a; Mediastinum). Passes behind the root of the lung to form the pulmonary plexus, then on to the oesophagus to form the oesophageal plexus with the vagus from the other side. Both pass through the oesophageal opening of the diaphragm to supply the abdominal contents and GIT as far as the splenic flexure (see Fig. 21; Autonomic nervous system).
 to the external auditory meatus and tympanic membrane.
to the external auditory meatus and tympanic membrane.
 to muscles of the pharynx and soft palate.
to muscles of the pharynx and soft palate.
The vagi form a major part of the parasympathetic nervous system. Vagal reflexes causing bradycardia, laryngospasm and bronchospasm may occur during anaesthesia. Intense stimulation may result in partial or complete heart block or even asystole. Anal and cervical stretching (e.g. Brewer–Luckhardt reflex) and traction on the extraocular muscles (oculocardiac reflex) are particularly intense stimuli, but it may also follow skin incision and stimulation (e.g. surgical) of the mesentery, biliary tract, uterus, bladder, urethra, testes, larynx, glottis, bronchial tree and carotid sinus. Also involved in the diving reflex.
Anticholinergic drugs antagonise vagal reflexes during surgery. Should they occur, surgical activity should cease, and atropine or glycopyrronium be administered if necessary.
Valproate/valproic acid, see Sodium valproate
• Direct arterial BP tracings in normal subjects show four phases (Fig. 162):
 phase I: increase in intrathoracic pressure expels blood from thoracic vessels.
phase I: increase in intrathoracic pressure expels blood from thoracic vessels.
 phase II: decrease in BP due to reduction of venous return; activation of the baroreceptor reflex causes tachycardia and vasoconstriction, raising BP towards normal.
phase II: decrease in BP due to reduction of venous return; activation of the baroreceptor reflex causes tachycardia and vasoconstriction, raising BP towards normal.
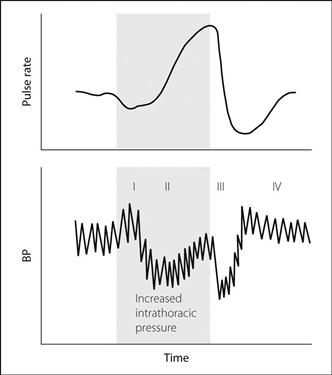
Fig. 162 Normal Valsalva response (see text)
 ‘square wave’ response, seen in cardiac failure, constrictive pericarditis, cardiac tamponade and valvular heart disease, when CVP is markedly raised. BP rises, remains high throughout the manoeuvre and returns to its previous level at the end.
‘square wave’ response, seen in cardiac failure, constrictive pericarditis, cardiac tamponade and valvular heart disease, when CVP is markedly raised. BP rises, remains high throughout the manoeuvre and returns to its previous level at the end.
 autonomic dysfunction, e.g. autonomic neuropathy, drugs. BP falls and stays low until intrathoracic pressure is released. Pulse rate changes and overshoot are absent.
autonomic dysfunction, e.g. autonomic neuropathy, drugs. BP falls and stays low until intrathoracic pressure is released. Pulse rate changes and overshoot are absent.
 an exaggerated reduction in BP may be seen in hypovolaemia, e.g. during IPPV.
an exaggerated reduction in BP may be seen in hypovolaemia, e.g. during IPPV.
Useful as a bedside test of autonomic function. Concurrent ECG tracing allows accurate measurement of changes in heart rate. The manoeuvre may be useful in evaluating heart murmurs, and may be successful in terminating SVT (because of increased vagal tone in phase IV).
Valtis–Kennedy effect. Shift to the left of the oxyhaemoglobin dissociation curve during blood storage, originally described in 1954 for acid–citrate–dextrose storage. The shift reflects progressive depletion of 2,3-DPG.
[DJ Valtis, Greek physician; Arthur C Kennedy (1922–2009), Glasgow physician]
Valveless anaesthetic breathing systems. Anaesthetic breathing systems designed to eliminate resistance due to adjustable pressure-limiting valves. In the Samson system, the valve is replaced by an adjustable orifice; in the Hafnia systems, expired gases pass through a port, assisted by an ejector flowmeter.
[Heyman H Samson, South African anaesthetist; Hafnia: Latin name for Copenhagen]
Valvular heart disease. Causes, features and anaesthetic management: as for congenital heart disease and individual lesions. Valve replacement: as for cardiac surgery. Many prosthetic valves are available in different sizes, e.g. Silastic ball-and-cage, metal flaps and porcine valves. Thrombosis may form on prostheses, hence the requirement for long-term anticoagulation. Patients with prosthetic valves may also require prophylactic antibiotics as for congenital heart disease.
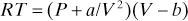
Van der Waals equation of state. Modification of the ideal gas law, accounting for the forces of attraction between gas molecules, and also the volume of the molecules:
Van der Waals forces. Weak attractive forces between neutral molecules and atoms, caused by electric polarisation of the particles induced by the presence of other particles.
Van Slyke apparatus. Device used to measure blood gas partial pressures. O2 and CO2 are released into a burette from the blood by addition of a liberating solution. Each gas in turn is converted to a non-gaseous substance by chemical reaction, and the pressure drop in the burette measured for each. The same reagents may be used as in the Haldane apparatus.
[Donald D van Slyke (1883–1971), US chemist]
See also, Carbon dioxide measurement; Gas analysis; Oxygen measurement
Vancomycin. Glycopeptide and antibacterial drug with bactericidal activity against aerobic and anaerobic Gram-positive bacteria (including multi-resistant staphylococci). Usually reserved for severe infections, resistant organisms or penicillin allergy. Despite this restriction in use, resistant species of vancomycin-resistant Staphylococcus aureus and entercocci are increasingly seen. Not absorbed orally.
• Dosage:
 125–250 mg orally qds, in pseudomembranous colitis (for 7–10 days).
125–250 mg orally qds, in pseudomembranous colitis (for 7–10 days).
Vancomycin-resistant enterococci, see Infection control; Vancomycin
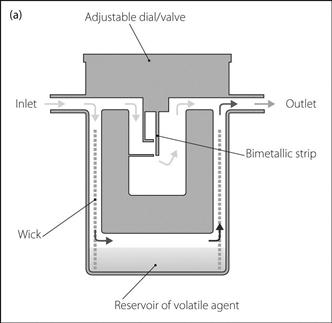
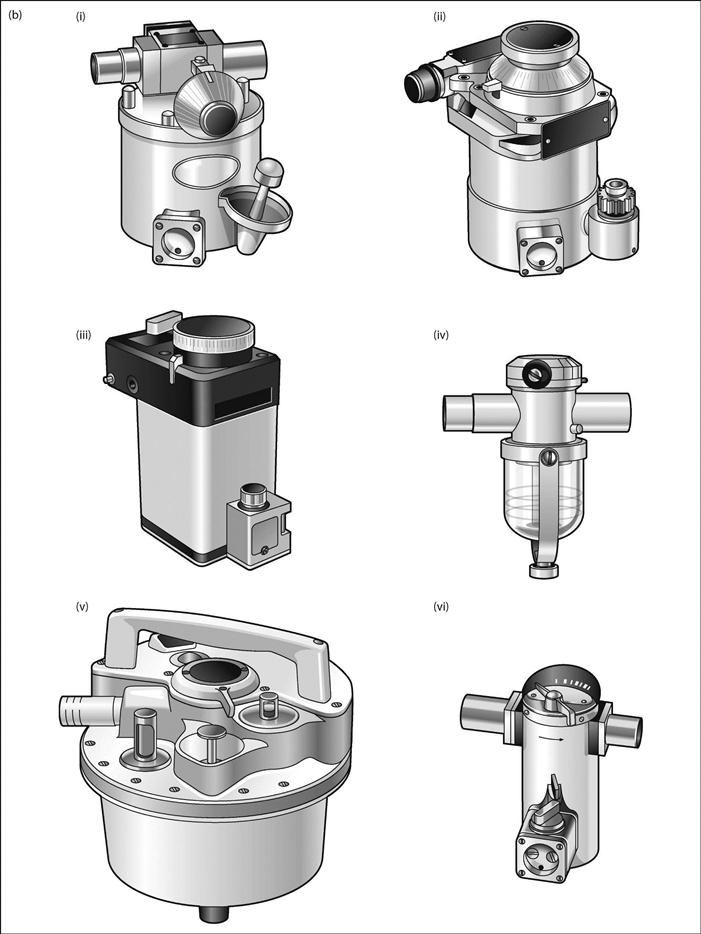
Vaporisers. Devices for delivering accurate and safe concentrations of volatile inhalational anaesthetic agents to the patient.
– gas passes through the vaporiser under pressure at the back bar of the anaesthetic machine.
– in most modern types (e.g. ‘Tec’ [temperature-compensated] vaporisers) fresh gas is divided by the control dial into two streams, one of which enters the vaporisation chamber, becomes fully saturated with agent and rejoins the other stream at the outlet (Fig. 163a). The ratio of the two streams (splitting ratio) determines the final delivered concentration (N.B. a different mechanism exists for the Tec 6 desflurane vaporiser: see below). In older vaporisers the delivered concentration was also affected by other factors (see below). In the obsolete ‘copper kettle’ type, a separate supply of O2 was passed through the vaporiser, becoming fully saturated. It was then added to the main fresh gas flow, at a rate calculated according to desired final concentration and vaporiser temperature. The original design included a large mass of copper as a heat sink, hence its name.
– have high resistance, so unsuitable for positioning in a circle system.
– performance is not affected by whether ventilation is spontaneous or controlled.
– include the Tec series of vaporisers. Features of the Mark 4 over the Mark 3 (Fig. 163b):
– flow of liquid agent into the delivery line is prevented if the vaporiser is inverted.
– interlock system prevents use of more than one vaporiser at a time, if mounted side by side.
– fitted with the key filling system (not fitted to all Mark 3 models).
Features of the Mark 5 over the Mark 4:
Features of the Mark 6 (desflurane vaporiser):
– cannot use the above mechanism because desflurane’s BP is very close to room temperature and therefore small variations in the latter result in large changes in SVP.
– requires an electrical power supply for the heating elements and control mechanisms.
Features of the Mark 7 over the Mark 5 (all modern agents but desflurane):
– more accurate and easily controllable output throughout different flow ranges.
– improved filling options and protection against spillage and contamination.
 draw-over vaporisers: despite their variable output, often preferred in the battlefield (e.g. triservice apparatus) and developing countries because they are cheap, simple and portable:
draw-over vaporisers: despite their variable output, often preferred in the battlefield (e.g. triservice apparatus) and developing countries because they are cheap, simple and portable:
– gas is drawn into the vaporising chamber by the patient’s inspiratory effort.
– performance is affected by minute ventilation, the output falling as ventilation increases.
– may be suitable for use within circle systems, e.g. Goldman vaporiser (Fig. 163b), a small, light, uncompensated device with a glass container (originally adapted from a motor vehicle fuel pump). Similar vaporisers were designed by McKesson and Rowbotham, the latter’s containing a wire gauze wick.
– also used for draw-over techniques, e.g. (Fig. 163b):
– EMO (Epstein and Macintosh of Oxford) diethyl ether inhaler: large vaporiser, incorporating a large vaporisation chamber, a water jacket for a heat sink and a temperature-compensating fluid-filled bellows at the outlet.
– obsolete types, used formerly for obstetric analgesia:
– Emotril (Epstein and Macintosh of Oxford/Trilene) trichloroethylene apparatus: incorporated within a metal box.
– Cardiff methoxyflurane inhaler: free-standing on a base.
 systems involving addition of liquid volatile agent directly to the fresh gas stream:
systems involving addition of liquid volatile agent directly to the fresh gas stream:
– incorporated into computerised anaesthetic machines.
– combined with a carbon filter/evaporator system that fits into the patient’s breathing system, conserving and recycling ~90% of the administered agent. Have been used for sedation on ICU without the need for anaesthetic machines.
• Factors affecting the delivered concentration:
 splitting ratio (plenum vaporisers).
splitting ratio (plenum vaporisers).
 temperature of the liquid: affects the SVP. As liquid vaporises, latent heat of vaporisation is lost, and temperature and thus SVP fall. Delivered concentration of agent would therefore fall if not for temperature compensation devices, e.g.:
temperature of the liquid: affects the SVP. As liquid vaporises, latent heat of vaporisation is lost, and temperature and thus SVP fall. Delivered concentration of agent would therefore fall if not for temperature compensation devices, e.g.:
– fluid-filled bellows at the gas outlet, e.g. EMO inhaler (see below); expands as temperature rises.
– longitudinally expanding metal rod at the gas outlet, e.g. Dräger models.
 surface area of the gas/liquid interface: increased with:
surface area of the gas/liquid interface: increased with:
– a cowl to direct gas flow on to or into the liquid (e.g. the original Boyle’s bottle).
Vaporisers have been associated with many hazards, and require regular servicing.
Vapour. Matter in the gaseous state below its critical temperature; i.e. its constituent particles may enter the liquid state. As liquid vaporises, heat is required (latent heat of vaporisation); as vapour condenses, an equal amount of heat is produced. These processes occur continuously above the surface of a liquid at equilibrium.
Vapour pressure. Pressure exerted by molecules escaping from the surface of a liquid to enter the gaseous phase. When equilibrium is reached at any temperature, the number of molecules leaving the liquid phase equals the number entering it; the vapour pressure now equals SVP. Raising the temperature of the liquid increases the molecules’ kinetic energy, allowing more of them to escape and raising the vapour pressure. When SVP equals atmospheric pressure, the liquid boils.
Vaptans, see Vasopressin receptor antagonists
Variance. Standard deviation squared. Thus an indicator of spread of values within a sample. Although standard deviation is commonly used when describing data, many statistical calculations employ its square, hence the use of variance as a meaningful term (e.g. analysis of variance, ANOVA).
Vascular access, see Central venous cannulation; Intravenous fluid administration
Vascular resistance, see Pulmonary vascular resistance; Systemic vascular resistance
Vasculitides. Group of conditions characterised by inflammation of blood vessels. All except giant cell arteritis are uncommon and associated with connective tissue diseases or drug hypersensitivity. Diagnosis requires biopsy, which often shows granuloma formation associated with vessel inflammation.
 group 1: systemic necrotising arteritis of small/medium arteries:
group 1: systemic necrotising arteritis of small/medium arteries:
– connective tissue disease-associated arteritis.
 group 2: small vessel vasculitis:
group 2: small vessel vasculitis:
– Henoch–Schönlein purpura: usually occurs in childhood following an upper respiratory tract infection. Features include fever, headache, macular/urticarial rash becoming purpuric, over the buttocks and limbs. Inflammatory synovitis is common. Focal glomerulonephritis may lead to nephrotic syndrome and, rarely, renal failure.
– mixed cryoglobulinaemic vasculitis.
– connective tissue disease-associated vasculitis.
 group 3: giant cell arteritis/large artery vasculitis:
group 3: giant cell arteritis/large artery vasculitis:
– temporal arteritis: usually affects the elderly and often associated with polymyalgia rheumatica. Headache, often localised, is the predominant symptom. Blindness may result if corticosteroids are not given promptly.
– Takayasu’s arteritis: rare large vessel arteritis affecting young women. Affects the aorta and its branches, causing inflammation and then stenosis of affected vessels. Features include cerebrovascular insufficiency (fainting, dizziness) and reduced peripheral pulses. Treatment depends on the underlying condition but usually includes immunosuppressive drugs.
Vasoconstrictor drugs, see Vasopressor drugs
Vasodilator drugs. Drugs causing vasodilatation as their primary effect (cf. isoflurane, morphine). The term is sometimes reserved for drugs acting directly at vascular smooth muscle. Nitric oxide is thought to be a common end pathway for most drugs.
• May be divided according to their main site of action, although considerable overlap occurs:
 venous system: GTN, isosorbide.
venous system: GTN, isosorbide.
 arterial system: hydralazine, calcium channel blocking drugs, salbutamol, diazoxide, minoxidil, adenosine.
arterial system: hydralazine, calcium channel blocking drugs, salbutamol, diazoxide, minoxidil, adenosine.
 venous and arterial systems: sodium nitroprusside, α-adrenergic receptor antagonists, angiotensin converting enzyme inhibitors, ganglion blocking drugs, potassium channel activators.
venous and arterial systems: sodium nitroprusside, α-adrenergic receptor antagonists, angiotensin converting enzyme inhibitors, ganglion blocking drugs, potassium channel activators.
• Used to reduce SVR and thus:
 systemic BP, e.g. in hypotensive anaesthesia, hypertensive crisis, pre-eclampsia. Their effect is sometimes offset by reflex tachycardia.
systemic BP, e.g. in hypotensive anaesthesia, hypertensive crisis, pre-eclampsia. Their effect is sometimes offset by reflex tachycardia.
 afterload and ventricular work, e.g. in cardiac failure, shock. Increase stroke volume and reduce myocardial O2 demand.
afterload and ventricular work, e.g. in cardiac failure, shock. Increase stroke volume and reduce myocardial O2 demand.
Also reduce preload via venous dilatation. Also used to reduce pulmonary vascular resistance in pulmonary hypertension, although the systemic circulation is usually affected too.
Vasomotor centre. Group of neurones in the ventrolateral medulla, involved in the control of arterial BP. Projects to sympathetic preganglionic neurones in the spinal cord. Normal continuous discharge causes partial contraction of vascular smooth muscle (vasomotor tone) and resting sympathetic stimulation of the heart.
 chemoreceptor discharge.
chemoreceptor discharge.
 hypoxia (causes direct stimulation initially, but depression follows).
hypoxia (causes direct stimulation initially, but depression follows).
 baroreceptor discharge.
baroreceptor discharge.
Thus responds to hypotension (reduced baroreceptor discharge) by increasing sympathetic activity.
Dorsal and medial neurones functionally constitute the cardioinhibitory centre, stimulation of which inhibits the vasomotor centre and increases vagal activity.
Vasopressin (Arginine vasopressin, AVP; Antidiuretic hormone, ADH). Neuropeptide synthesised in the cell bodies of the supraoptic and paraventricular nuclei of the hypothalamus. Transported down their axons to the posterior lobe of the pituitary gland, from where it is secreted. Metabolised in the kidney and liver, it has a circulatory half-life of 10–30 min. There are at least three types of vasopressin receptor, all of which are G protein-coupled receptors: V1 receptors are Gq-coupled and located primarily on vascular smooth muscle and platelets; V2 receptors (Gs-coupled) mediate vasopressin’s antidiuretic actions on the kidney; and V3 receptors (coupled to multiple G proteins) are located centrally and involved in vasopressin’s neurotransmitter actions.
 water retention by the kidney, acting via V2 vasopressin receptors. These increase adenylate cyclase activity and cAMP levels, triggering insertion of water channels (aquaporins) into the luminal membranes of cells in the renal collecting ducts. This results in water reabsorption from the renal tubules. Urine volume decreases; its concentration increases. Conversely, plasma volume increases; its concentration decreases.
water retention by the kidney, acting via V2 vasopressin receptors. These increase adenylate cyclase activity and cAMP levels, triggering insertion of water channels (aquaporins) into the luminal membranes of cells in the renal collecting ducts. This results in water reabsorption from the renal tubules. Urine volume decreases; its concentration increases. Conversely, plasma volume increases; its concentration decreases.
 has a role in temperature regulation, control of circadian rhythm and memory function.
has a role in temperature regulation, control of circadian rhythm and memory function.
 increased plasma levels of coagulation factor VIII.
increased plasma levels of coagulation factor VIII.
 increased plasma osmolality; detected by osmoreceptors in the anterior hypothalamus.
increased plasma osmolality; detected by osmoreceptors in the anterior hypothalamus.
 decreased ECF volume and hypotension (e.g. in haemorrhage); detected by baroreceptors.
decreased ECF volume and hypotension (e.g. in haemorrhage); detected by baroreceptors.
 pain, nausea, hypoxaemia, emotional and physical stress.
pain, nausea, hypoxaemia, emotional and physical stress.
 drugs, e.g. morphine, barbiturates.
drugs, e.g. morphine, barbiturates.
 drugs, e.g. alcohol, butorphanol.
drugs, e.g. alcohol, butorphanol.
• Used therapeutically in various forms:
 argipressin: synthetic vasopressin; used in pituitary diabetes insipidus (DI; 5–20 U sc/im, 4-hourly) and for control of bleeding oesophageal varices (20 U iv over 15 min). Side effects include pallor, nausea, abdominal cramps and myocardial ischaemia. GTN (patch or iv) has been used to reduce the incidence and severity of side effects.
argipressin: synthetic vasopressin; used in pituitary diabetes insipidus (DI; 5–20 U sc/im, 4-hourly) and for control of bleeding oesophageal varices (20 U iv over 15 min). Side effects include pallor, nausea, abdominal cramps and myocardial ischaemia. GTN (patch or iv) has been used to reduce the incidence and severity of side effects.
 terlipressin: a prodrug, it is enzymatically cleaved to release vasopressin. Dosage: 2 mg iv followed by 1–2 mg 4–6-hourly for up to 72 h. Side effects are milder than after argipressin.
terlipressin: a prodrug, it is enzymatically cleaved to release vasopressin. Dosage: 2 mg iv followed by 1–2 mg 4–6-hourly for up to 72 h. Side effects are milder than after argipressin.
 desmopressin: may be given nasally, orally or by im/sc/iv injection. Minimal vasoconstrictor activity; used in pituitary DI and to boost factor VIII levels in haemophilia and von Willebrand’s disease.
desmopressin: may be given nasally, orally or by im/sc/iv injection. Minimal vasoconstrictor activity; used in pituitary DI and to boost factor VIII levels in haemophilia and von Willebrand’s disease.
 felypressin: used as a vasoconstrictor in local anaesthesia.
felypressin: used as a vasoconstrictor in local anaesthesia.
Vasopressin has been used as an alternative to adrenaline in the treatment of cardiac arrest and septic shock, and as a means of preserving organ function in brainstem-dead donors. Vasopressin receptor antagonists have been studied for use in cardiac failure and hyponatraemia.
Treschan TA, Peters J (2006). Anesthesiology; 105: 599–612
See also, Syndrome of inappropriate antidiuretic hormone secretion
Vasopressin receptor antagonists (Vaptans). Competitive antagonists at V2 vasopressin receptors, used for the treatment of hyper- and euvolaemic hyponatraemia, e.g. in cardiac failure/hepatic failure and syndrome of inappropriate antidiuretic hormone secretion (SIADH) respectively. Cause increased free water excretion, leading to an increase in plasma sodium concentration and reduced total body water.
Increased water intake due to increased thirst may reduce their efficacy. Other side effects include dehydration, nausea, skin rashes and orthostatic hypotension. Contraindicated in hypovolaemic hyponatraemia. All vaptans are substrates and inhibitors of the CYP3A4 isoenzyme of the cytochrome oxidase system; caution is therefore required when co-administered with drugs causing enzyme induction/inhibition. Tolvaptan is the only agent available in the UK and is licensed for the treatment of SIADH.
Vasopressor drugs. Drugs causing vasoconstriction; used to increase arterial BP, e.g. during anaesthesia, intensive care or CPR, or to prolong the action of local anaesthetic agents by preventing their systemic absorption. Formerly used rather indiscriminately to increase BP, they are now reserved for situations where vasodilatation is a specific problem, e.g. anaphylaxis, spinal anaesthesia.
vCJD, see Creutzfeldt–Jakob disease
Vecuronium bromide. Non-depolarising neuromuscular blocking drug, introduced in the UK in 1983. A monoquaternary aminosteroid, similar in structure to pancuronium. Initial dose is 80–100 µg/kg; good intubating conditions occur within 90–120 s. Relaxation lasts for 20–30 min; duration is increased to 50 min if 150 µg/kg is used, and 80 min if 250 µg/kg is used. Supplementary dose: 20–30 µg/kg (30–50 µg/kg initial dose after administration of suxamethonium for intubation). May also be given by infusion, at 50–80 µg/kg/h.
Causes minimal histamine release, ganglion or vagal blockade, even at several times the usual doses. Thus has minimal effects on BP and pulse, but may allow unopposed vagal stimulation to cause bradycardia. Metabolised in the liver to the active 3-desacetylvecuronium. Excreted mainly in bile, but also in urine. Reversal of action is fast, and acetylcholinesterase inhibitors may not always be required. Cumulation is unlikely.
Vegetative state. Disorder of consciousness in which the patient appears to be awake but is unaware of him-/herself or the surrounding environment; differs from coma (patient is neither awake nor aware) or the minimally conscious state (patient is awake and appears to be intermittently aware). Due to injury to cortical, subcortical and thalamic structures.
• May be:
 acute: head injury, hypoxic/anoxic brain injury, infection (meningitis, encephalitis), CVA.
acute: head injury, hypoxic/anoxic brain injury, infection (meningitis, encephalitis), CVA.
 subacute: in the course of a neurodegenerative process e.g. Alzheimer’s disease.
subacute: in the course of a neurodegenerative process e.g. Alzheimer’s disease.
 time spent in vegetative state (only 3% of patients regain independence after 6 months).
time spent in vegetative state (only 3% of patients regain independence after 6 months).
 age (best prognosis is in those <20 years old).
age (best prognosis is in those <20 years old).
 type of brain injury (traumatic injuries have better outcomes than non-traumatic).
type of brain injury (traumatic injuries have better outcomes than non-traumatic).
[Alois Alzheimer (1864–1915), German neurologist and pathologist]
Venous admixture. Refers to lowering of arterial PO2 from the ‘ideal’ level which would occur if there were no shunt or  mismatch, either of which may lower PO2. Defined as the amount of true shunt that would give the observed PO2. May be calculated from the shunt equation.
mismatch, either of which may lower PO2. Defined as the amount of true shunt that would give the observed PO2. May be calculated from the shunt equation.
Venous cannulation, see Central venous cannulation; Intravenous fluid administration
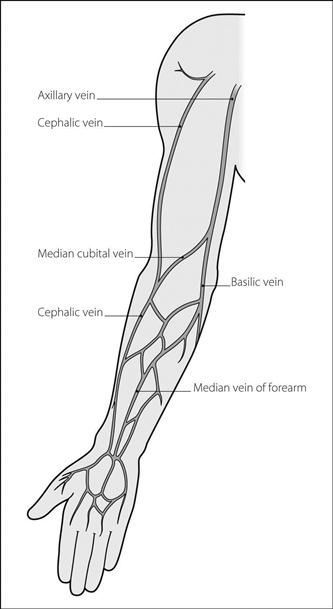
Venous drainage of arm. Deep veins accompany the arteries (deep venae comitantes). Superficial veins on the back of the hand form the dorsal venous arch, from which the basilic and cephalic veins arise. Smaller veins arise from the anterior aspect of the arm (Fig. 164). The anatomy of the veins may vary considerably, especially that of the cephalic vein.
Venous drainage of head and neck, see Cerebral circulation; Jugular veins
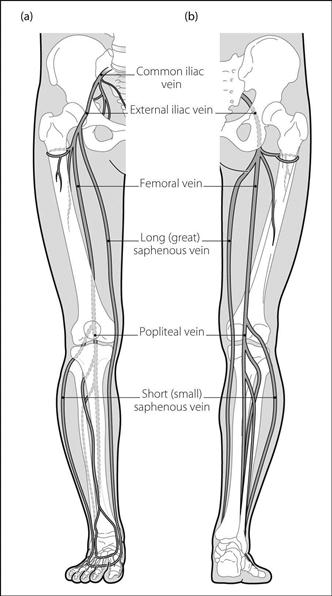
Venous drainage of leg. Comprises superficial and deep veins (Fig. 165):
Venous pressure, see Central venous pressure; Jugular venous pressure; Venous waveform
Venous return. Refers to the volume of blood entering the right atrium per minute. A major determinant of cardiac output, as described by Starling’s law.
Venous waveform. Obtained from the tracing of CVP. Can be seen but not felt in the neck as the JVP. Consists of named waves and descents (Fig. 166):
 ‘a’ wave is due to atrial contraction.
‘a’ wave is due to atrial contraction.
 ‘v’ wave is due to atrial filling.
‘v’ wave is due to atrial filling.
 ‘x’ descent is due to atrial relaxation.
‘x’ descent is due to atrial relaxation.
• Abnormalities seen in the JVP wave may assist diagnosis of certain valve and rhythm disorders:
– stiff right ventricle, e.g. pulmonary stenosis, pulmonary hypertension.
 enlarged ‘v’ wave: tricuspid regurgitation, e.g. due to cardiac failure.
enlarged ‘v’ wave: tricuspid regurgitation, e.g. due to cardiac failure.
 cannon waves (large waves, not corresponding to ‘a’, ‘v’ or ‘c’ waves):
cannon waves (large waves, not corresponding to ‘a’, ‘v’ or ‘c’ waves):
– complete heart block (irregular).
– junctional arrhythmias (regular).
A similar waveform is seen in the left atrial pressure tracing.
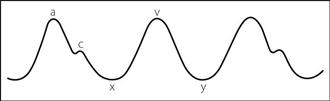
Fig. 166 Venous waveform (see text)
Ventilation, controlled, see Airway pressure release ventilation; Assisted ventilation; High-frequency ventilation; Inspiratory pressure support; Inspiratory volume support; Intermittent mandatory ventilation; Intermittent negative pressure ventilation; Intermittent positive pressure ventilation; Inverse ratio ventilation; Mandatory minute ventilation; Pressure-regulated volume control ventilation; Proportional assist ventilation; Synchronised intermittent mandatory ventilation
Ventilation, liquid, see Liquid ventilation
Ventilation, spontaneous, see Breathing, control of; Breathing, work of; Respiratory muscles
Ventilation/perfusion mismatch ( mismatch). Imbalance between alveolar ventilation (
mismatch). Imbalance between alveolar ventilation ( ) and pulmonary capillary blood flow (
) and pulmonary capillary blood flow ( ). In the ideal lung model, ventilation would be distributed uniformly to all parts of the lung and would be matched by uniform distribution of blood flow (i.e.
). In the ideal lung model, ventilation would be distributed uniformly to all parts of the lung and would be matched by uniform distribution of blood flow (i.e.  = 1). However, even in a healthy 70 kg male, alveolar ventilation and blood flow are unequal (4 l/min and 5 l/min respectively), giving a
= 1). However, even in a healthy 70 kg male, alveolar ventilation and blood flow are unequal (4 l/min and 5 l/min respectively), giving a  ratio of 0.8.
ratio of 0.8.
In addition, gravitational forces result in a gradient of  ratios in the lung as one travels from the base to the apex in the upright position (Fig. 167). Both ventilation and perfusion decrease from base to apex, but perfusion to a greater extent than ventilation. Thus the
ratios in the lung as one travels from the base to the apex in the upright position (Fig. 167). Both ventilation and perfusion decrease from base to apex, but perfusion to a greater extent than ventilation. Thus the  ratio is higher at the apex (
ratio is higher at the apex ( = 3.3) than at the base (
= 3.3) than at the base ( = 0.63). Similar but smaller changes occur across the lung in the supine position.
= 0.63). Similar but smaller changes occur across the lung in the supine position.
 mismatch may result in
mismatch may result in  ratios ranging from zero (perfusion but no ventilation) to infinity (ventilation but no perfusion). Its effects on gas exchange are those of shunt and dead space respectively, and can be assessed by determining venous admixture and physiological dead space.
ratios ranging from zero (perfusion but no ventilation) to infinity (ventilation but no perfusion). Its effects on gas exchange are those of shunt and dead space respectively, and can be assessed by determining venous admixture and physiological dead space.  mismatch is a common cause of hypoxaemia in pulmonary disease, e.g. COPD, asthma, chest infection and pulmonary oedema and circulatory disorders, e.g. PE.
mismatch is a common cause of hypoxaemia in pulmonary disease, e.g. COPD, asthma, chest infection and pulmonary oedema and circulatory disorders, e.g. PE.
Mismatch may be measured using radioisotope scanning of ventilation and perfusion separately, e.g. with xenon and technetium.
See also, Pulmonary circulation
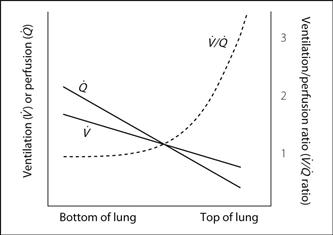
Fig. 167  mismatch graph
mismatch graph
Ventilator-associated lung injury (VALI). Acute lung injury associated with mechanical IPPV. Attributed to: the use of high inspiratory plateau pressures; high tidal volumes; and repeated collapse and expansion of airways and associated lung units. These result in barotrauma, volutrauma and atelectrauma, respectively which, in turn, lead to biotrauma (local and systemic inflammation with activation of neutrophils and release of cytokines). Lung protection strategies aim to mitigate these effects.
Gattinoni L, Protti A, Caironi P, Carlesso P (2010). Crit Care Med; 38(Suppl): S539–48
See also, Barotrauma; Intermittent positive pressure ventilation
Ventilator-associated pneumonia (VAP). Nosocomial pneumonia developing more than 48 h after tracheal intubation and IPPV. Accounts for ~30% of ICU infections and is an important cause of ICU mortality. Early infections are most often due to common respiratory flora, late infections often due to pseudomonas species, resistant staphylococci and acinetobacter species. Viruses and fungi may also be causal agents.
 patient-related: age, cardiorespiratory disease, immunodeficiency, ARDS, coma, MODS.
patient-related: age, cardiorespiratory disease, immunodeficiency, ARDS, coma, MODS.
 ventilator-related: duration of IPPV >7 days, tracheal cuff pressure <20 cmH2O, reintubation, tracheostomy.
ventilator-related: duration of IPPV >7 days, tracheal cuff pressure <20 cmH2O, reintubation, tracheostomy.
 general ICU care: supine position, invasive devices, aspiration, H2 receptor antagonists, recent antibiotic therapy.
general ICU care: supine position, invasive devices, aspiration, H2 receptor antagonists, recent antibiotic therapy.
Diagnostic criteria include: CXR infiltrates; fever; leucocytosis; purulent sputum; and positive microbiological cultures of tracheobronchial aspirates or brush specimens. Differential diagnosis includes pulmonary oedema, atelectasis, PE, ARDS and pulmonary haemorrhage.
Treatment includes chest physiotherapy and appropriate antibiotic therapy, guided either by positive cultures and sensitivities, or empirical selection based on the most likely organisms.
Preventive measures, often delivered as a care bundle, include: good oral care; elevation of the bed-head to 30–45°; prevention of over-sedation; protocol-driven weaning from ventilators; and monitoring of tracheal cuff pressures.
Hunter JD (2012). Br Med J; 344: e3325
See also Chest infection; Intubation, tracheal; Nosocomial infections; Sepsis
Ventilators. Mechanical devices for ventilating the lungs. First described in the early 1900s as an alternative to resuscitation equipment incorporating bellows. The polio epidemic in Denmark in 1952 was a major impetus to the development of reliable positive pressure ventilators.
 negative pressure devices used for intermittent negative pressure ventilation: the negative pressure around the thorax causes chest expansion and draws in air:
negative pressure devices used for intermittent negative pressure ventilation: the negative pressure around the thorax causes chest expansion and draws in air:
– tank ventilators (‘iron lungs’):
– enclose the whole body (apart from the head and neck) within an airtight casing.
– efficient, but access to the patient is very restricted.
– enclose the thorax and upper abdomen. Inflatable jacket versions have been described.
– less restrictive but less efficient.
Do not protect against aspiration of gastric contents. Their effectiveness may be reduced by indrawing of the soft tissues of the upper airway during inspiration. Tracheostomy may be required if this occurs.
 positive pressure devices used for IPPV: deliver positive pressure to the lungs either invasively via a tracheal tube, tracheostomy, or injector device, or non-invasively via facemask or nasal mask (non-invasive positive pressure ventilation).
positive pressure devices used for IPPV: deliver positive pressure to the lungs either invasively via a tracheal tube, tracheostomy, or injector device, or non-invasively via facemask or nasal mask (non-invasive positive pressure ventilation).
Positive pressure ventilators are widely used during anaesthesia and in ICU. They may be powered:
– by a separate supply of compressed air or O2, employing fluidics or pneumatics (e.g. Penlon Nuffield ventilator).
– by anaesthetic gases (e.g. Manley ventilator). These types are ‘minute volume dividers’ (see below).
 ‘mechanical thumbs’: intermittent occlusion of the open limb of a T-piece, e.g. by a solenoid, e.g. the Sheffield infant ventilator. ‘Intermittent blowers’ may be used to achieve a similar effect by moving a column of driving gas forwards and backwards along a length of tubing connecting the ventilator with the T-piece, e.g. the Penlon Nuffield ventilator attached to the Bain coaxial anaesthetic breathing system. Anaesthetic gases are delivered separately through the other limb of the T-piece. A similar technique may be used with a circle system.
‘mechanical thumbs’: intermittent occlusion of the open limb of a T-piece, e.g. by a solenoid, e.g. the Sheffield infant ventilator. ‘Intermittent blowers’ may be used to achieve a similar effect by moving a column of driving gas forwards and backwards along a length of tubing connecting the ventilator with the T-piece, e.g. the Penlon Nuffield ventilator attached to the Bain coaxial anaesthetic breathing system. Anaesthetic gases are delivered separately through the other limb of the T-piece. A similar technique may be used with a circle system.
 ‘minute volume dividers’: supply only the minute volume of anaesthetic gas delivered to them, by dividing the preset minute volume into equally sized breaths, e.g. Manley ventilators and (obsolete) ‘vents’ (e.g. Minivent, East–Freeman automatic vent: small devices, placed at the patient end of an anaesthetic breathing system, that intermittently allow gas flow when upstream pressure is sufficient to overcome the resistance offered by a magnetised bobbin within them). Delivered minute volume may be read directly from the anaesthetic machine flowmeters.
‘minute volume dividers’: supply only the minute volume of anaesthetic gas delivered to them, by dividing the preset minute volume into equally sized breaths, e.g. Manley ventilators and (obsolete) ‘vents’ (e.g. Minivent, East–Freeman automatic vent: small devices, placed at the patient end of an anaesthetic breathing system, that intermittently allow gas flow when upstream pressure is sufficient to overcome the resistance offered by a magnetised bobbin within them). Delivered minute volume may be read directly from the anaesthetic machine flowmeters.
 ‘intermittent blowers’: produce intermittent flow from a high-pressure source, e.g. cylinders. Include the Bird ventilators used on ICU, and small devices used for transportation of ventilated patients, e.g. Pneupac ventilator. The Penlon Nuffield ventilator is suitable for use with the Bain and circle systems; it may also be used for children (with a paediatric pressure release valve) using the T-piece.
‘intermittent blowers’: produce intermittent flow from a high-pressure source, e.g. cylinders. Include the Bird ventilators used on ICU, and small devices used for transportation of ventilated patients, e.g. Pneupac ventilator. The Penlon Nuffield ventilator is suitable for use with the Bain and circle systems; it may also be used for children (with a paediatric pressure release valve) using the T-piece.
 jet ventilators: include those used for injector techniques and high-frequency ventilation.
jet ventilators: include those used for injector techniques and high-frequency ventilation.
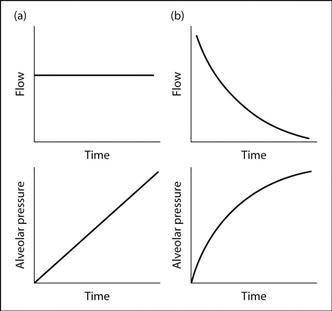
– flow generators: produce a high generating pressure (e.g. 400 kPa) and are thus able to deliver flow which is unaffected by patient characteristics. The flow produced may be constant or non-constant (usually the former). Non-constant flow generators include the Cape ventilator, in which flow is sinusoidal because of the crank mechanism employed. Most ICU ventilators are flow generators (Fig. 168a), as they are able to produce the high inflation pressures required to achieve the preset flow in non-compliant lungs, e.g. in bronchospasm. Barotrauma may occur if high airway pressures are reached.
– pressure generators: produce low generating pressure (e.g. 1.5 kPa); thus the flow delivered is affected by patient characteristics (Fig. 168b). Since the airway pressure attainable is preset, the risk of barotrauma is reduced. However, the tidal volume delivered depends on the resistance of the tubing and the patient’s respiratory mechanics, e.g. compliance, airway resistance. Pressure generators are usually employed in paediatric anaesthesia, to reduce the risk of barotrauma. Examples of constant pressure generators are the Manley and East Radcliffe ventilators.
– pressure-cycled: expiration begins when a preset airway pressure is reached, e.g. Bird ventilator.
During expiration, airway pressure may be allowed to fall to atmospheric pressure; most ventilators also allow application of PEEP. Negative end-expiratory pressure is no longer used. The switch from expiratory to inspiratory phases is usually time-cycled, although it may be triggered by the patient in some modes.
The ideal ventilator for use on ICU should: be flexible in flow or pressure generation and cycling as above; allow PEEP and special modes (e.g. for weaning); allow humidification and administration of nebulised drugs; be easy to sterilise; and incorporate monitors and alarms. Specific advanced ventilator modes used in ICU include airway pressure release ventilation, inspiratory pressure support, inspiratory volume support, intermittent mandatory ventilation, inverse ratio ventilation, mandatory minute ventilation, pressure-regulated volume control ventilation, proportional assist ventilation and synchronised intermittent mandatory ventilation. Many permit alteration of the I : E ratio, inspiratory waveform and PEEP.
Ventile, see Scavenging
Ventricular ectopic beats (VEs, VEBs; Premature ventricular contractions/beats, PVCs/PCBs). Contraction of ventricular muscle caused by an ectopic focus instead of normal impulse conduction. The ventricles discharge early; the next sinus impulse finds the ventricular muscle refractory, causing a pause before the next beat. VEs typically appear as wide bizarre complexes on the ECG (Fig. 169); VEs arising from different sites (i.e. multifocal) may have different configurations.
They may occur in normal hearts, but may also indicate organic heart disease. Other causes include drugs (e.g. halothane, digoxin, antiarrhythmic drugs), electrolyte and acid–base disturbances, hypoxaemia, hypercapnia and pain. Common during anaesthesia, especially with spontaneous ventilation with halothane. May occur at regular intervals, e.g. every second or third beat. Usually do not require treatment, apart from correction of the cause. Antiarrhythmic drugs (usually lidocaine) are usually recommended for VEs more common than 5 per minute, or if multifocal or close to the preceding T wave with risk of the R on T phenomenon.
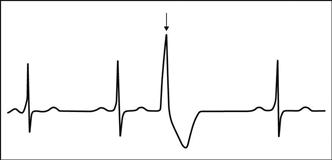
Fig. 169 Ventricular ectopic beat (arrowed)
Ventricular fibrillation (VF). Uncoordinated and ineffective ventricular contraction caused by completely irregular ventricular depolarisation. May follow the R on T phenomenon. Causes include myocardial ischaemia, MI, hypoxaemia, electrocution, electrolyte imbalance, hypothermia and drug toxicity (e.g. adrenaline, digoxin). There is no cardiac output; asystole therefore follows unless treated. VF is the most common cause of cardiac arrest. The ECG shows continuous random electrical activity without QRS complexes (Fig. 170).
Treated by defibrillation, although a single precordial thump is advocated for monitored arrests.

Fig. 170 Ventricular fibrillation
Ventricular septal defect (VSD). Accounts for 20–30% of congenital heart disease; may also follow MI or trauma. The commonest congenital form involves the membranous septum immediately below the tricuspid valve; bulbar or muscular septal involvement is rarer. Blood flows across the defect from left to right during systole. As right ventricular pressures decrease after birth, shunt increases. May cause cardiac failure in infancy. Small defects with normal pulmonary artery pressures are often asymptomatic (maladie de Roger) and may close spontaneously. Large defects may lead to pulmonary hypertension and Eisenmenger’s syndrome.
 harsh pansystolic murmur, heard best in the left fourth intercostal space (louder with small defects). Splitting of the second heart sound.
harsh pansystolic murmur, heard best in the left fourth intercostal space (louder with small defects). Splitting of the second heart sound.
 of Eisenmenger’s syndrome if present.
of Eisenmenger’s syndrome if present.
 of left and right ventricular hypertrophy on ECG and CXR.
of left and right ventricular hypertrophy on ECG and CXR.
Up to 25% of patients may be affected by bacterial endocarditis at some time.
• Treated by surgery or placement of a septal occluder using a percutaneous technique. Anaesthesia is as for congenital heart disease and cardiac surgery.
Ventricular stretch receptors, see Baroreceptors
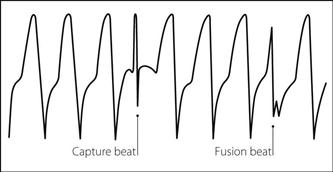
Ventricular tachycardia (VT). Rapid series of ventricular ectopic beats (usually defined as more than three in succession). The pulse rate usually lies between 130 and 250 beats/min. Normal atrial activity may continue independently, or the ventricular impulses may pass retrogradely to the atria.
• Distinguished from SVT by the following features (Fig. 171):
 QRS complexes are usually wide and bizarre.
QRS complexes are usually wide and bizarre.
 retrograde conduction to the atria may result in inverted P waves (which may be hidden by the QRS complexes).
retrograde conduction to the atria may result in inverted P waves (which may be hidden by the QRS complexes).
 independent atrial activity may be suggested by:
independent atrial activity may be suggested by:
– capture beats (normal QRS complexes following occasional normal atrioventricular conduction).
 marked left axis deviation, with all of the chest leads either negative or positive.
marked left axis deviation, with all of the chest leads either negative or positive.
Both VT and SVT may be regular, and associated with normotension or hypotension. Differentiation between broad-complex VT and SVT may be particularly difficult. The response to adenosine may aid diagnosis. Causes are as for ventricular ectopic beats.
• Treatment (following CPR if necessary):
 antiarrhythmic drugs, e.g. amiodarone.
antiarrhythmic drugs, e.g. amiodarone.
 cardioversion if there are adverse signs (e.g. hypotension) or drugs are contraindicated/ineffective.
cardioversion if there are adverse signs (e.g. hypotension) or drugs are contraindicated/ineffective.
 cardiac pacing has also been used.
cardiac pacing has also been used.
European Resuscitation Council (2010). Resuscitation; 81: 1219–76
Venturi principle. Entrainment of a fluid into an area of low pressure caused by a constriction in a tube (Bernoulli effect). Entrainment depends on appropriate positioning of the side-arm or entrainment port, a suitably shaped constriction and the gradual increase in diameter of the limb distal to the constriction.
The principle is employed in gas-mixing devices (including fixed performance oxygen therapy devices), suction equipment, ejector flowmeters, scavenging equipment and devices used to circulate gases round breathing systems.
Verapamil hydrochloride. Calcium channel blocking drug, mainly used as an antiarrhythmic drug to treat SVT. Acts by prolonging conduction through the atrioventricular node. Also used in angina and hypertension. Undergoes extensive first-pass metabolism when given orally. Excreted renally.
• Dosage:
 hypertension: up to 480 mg orally tds.
hypertension: up to 480 mg orally tds.
• Side effects: hypotension, bradycardia, complete heart block and asystole, especially if the patient has received β-adrenergic receptor antagonists. Contraindicated in Wolff–Parkinson–White syndrome, since atrioventricular block may promote conduction through accessory pathways with resultant arrhythmia. Its action may be potentiated by inhalational anaesthetic agents, especially halothane.
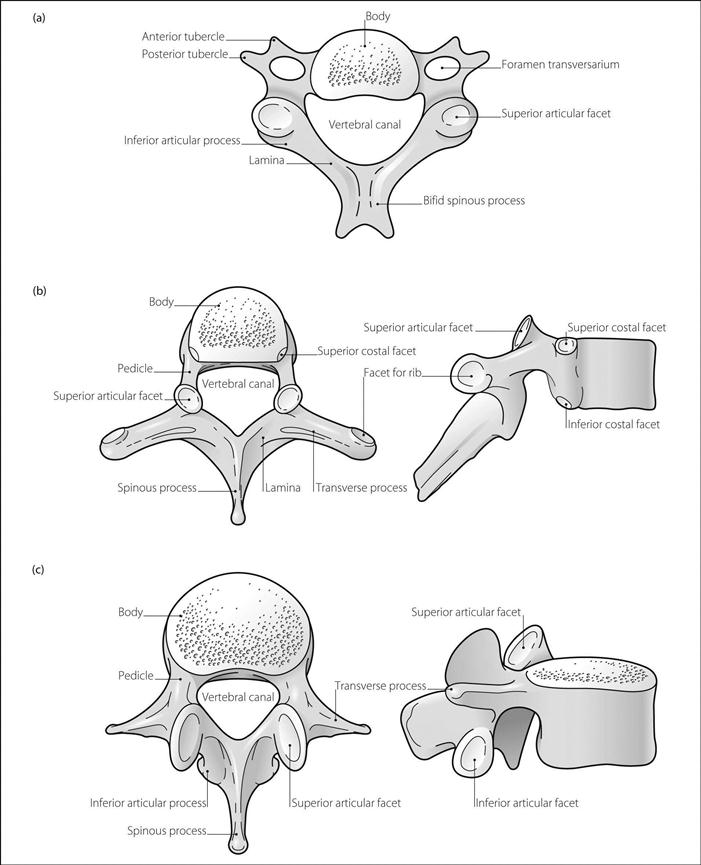
Vertebrae. Bony components of the vertebral column, which is about 70 cm long in the adult male and is flexed throughout its length in the fetus; after birth two secondary curves appear so that the cervical and lumbar regions are convex forwards and the thoracic and sacral regions are concave. There are 7 cervical vertebrae, 12 thoracic, 5 lumbar, 5 fused sacral and 3–5 fused coccygeal. Vertebral bodies of C2 to L5 are separated by fibrocartilaginous vertebral discs, accounting for about 25% of the spine’s total length. Each has an outer fibrous annulus fibrosus, and the more fluid inner nucleus pulposus. The latter may prolapse through the former, impinging upon the spinal cord or spinal nerves. Discs thin with age, resulting in reduced height. Vertebrae and discs are united by the vertebral ligaments.
• Structure of a typical vertebra:
 body: short and cylindrical and lies anteriorly.
body: short and cylindrical and lies anteriorly.
 arch: encloses the vertebral canal and lies posteriorly. Composed of the rounded pedicles anteriorly and the flattened laminae posteriorly. The laminae are united in the midline by the spinous process. They also bear transverse processes and superior and inferior articular processes which bear facets for articulation with adjacent vertebrae.
arch: encloses the vertebral canal and lies posteriorly. Composed of the rounded pedicles anteriorly and the flattened laminae posteriorly. The laminae are united in the midline by the spinous process. They also bear transverse processes and superior and inferior articular processes which bear facets for articulation with adjacent vertebrae.
– each has the foramen transversarium passing through its transverse processes, through which pass the vertebral arteries.
– articular facets articulate superiorly with the base of the skull.
– facet on the anterior edge of the vertebral canal articulates with the odontoid peg.
– C2–6: bifid spinous processes.
– body: heart-shaped, articulating with the ribs via superior and inferior costal facets at the rear of the body.
– spinous processes: long, inclined at about 60° to the horizontal.
– T1: has a longer upper facet for the first rib and a smaller lower facet for the second rib.
– T10–12: usually bear single costal facets on their bodies.
– T12: spinous process has notched lower edge.
– spines: project horizontally backwards.
 sacral: fused to form the sacrum, enclosing the sacral canal.
sacral: fused to form the sacrum, enclosing the sacral canal.
 coccygeal: fused to form the triangular coccyx, the base of which articulates with the sacrum.
coccygeal: fused to form the triangular coccyx, the base of which articulates with the sacrum.
Vertebral arteries. Arise from the subclavian arteries, passing upwards through the foramina transversaria of the upper six cervical vertebrae and passing medially behind the lateral mass of the atlas. They enter the skull through the foramen magnum, uniting to form the basilar artery after piercing the dura. Vertebrobasilar insufficiency typically results in dizziness, vertigo, diplopia and hemiparesis.
May be punctured during central venous cannulation and brachial plexus block.
Vertebral canal. Triangular canal within the vertebrae, with its base posteriorly. Contains:
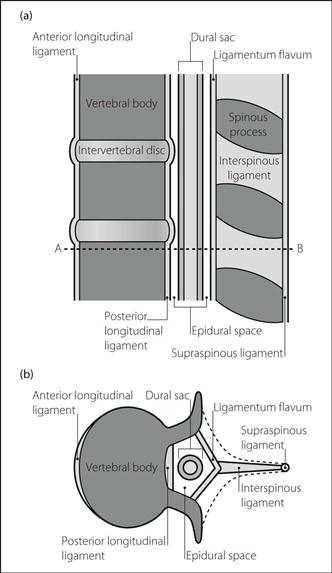
Vertebral ligaments. Individual vertebrae are linked by a number of ligaments (Fig. 173):
 interspinous ligaments: run between the spines of adjacent vertebrae.
interspinous ligaments: run between the spines of adjacent vertebrae.
 supraspinous ligament: runs from C7 to the sacrum, attached to the tips of the spines.
supraspinous ligament: runs from C7 to the sacrum, attached to the tips of the spines.
• Additional ligaments at the atlanto-occipito-axial complex:
 alar ligaments: pass from the sides of the odontoid peg to the occipital condyles.
alar ligaments: pass from the sides of the odontoid peg to the occipital condyles.
 posterior: overlies the sacral hiatus.
posterior: overlies the sacral hiatus.
 anterior: passes over the anterior aspect of the sacrum and coccyx.
anterior: passes over the anterior aspect of the sacrum and coccyx.
 lateral: joins the lateral angle of the sacrum to the transverse processes of the coccyx.
lateral: joins the lateral angle of the sacrum to the transverse processes of the coccyx.
Viagra, see Sildenafil
Victoria, Queen (1819–1901). British monarch, given chloroform by Snow during the births of her eighth and ninth children: Prince Leopold in 1853, and Princess Beatrice in 1857 (on the latter occasion, Prince Albert administered chloroform himself before Snow’s arrival). This gave respectability to pain relief during labour, which had been criticised as being against God’s will.
[Leopold (1853–1884), Beatrice (1857–1944), Albert (1819–1861)]
Vigabatrin. Anticonvulsant drug used as an adjuvant treatment for partial and secondary generalised seizures. Its efficacy in tonic–clonic seizures is less well documented. Irreversibly inhibits γ-aminobutyric acid transaminase (GABA-T), the enzyme responsible for breakdown of GABA. Duration of action approximately 24 h with elimination half-life of 7 h. Excreted unchanged in the urine.
Viscosity (η). Tendency of fluids to resist flow. Measured in poise. Equal to shear force (force per unit surface area) divided by velocity gradient between adjacent fluid layers. Dependent on intermolecular attractive forces (e.g. van der Waals forces) and entanglement of bulky molecules. Decreased at high temperatures; particles have more kinetic energy and may escape from their neighbours more easily. Laminar flow is inversely proportional to viscosity.
Blood viscosity depends largely on haematocrit (increasing exponentially as haematocrit increases), red cell characteristics and blood protein concentration. It rises with age and smoking. It is increased slightly by volatile anaesthetic agents. Blood viscosity alters with different flow rates; i.e. blood is a non-Newtonian fluid. At vessel diameters of less than 0.3 mm, it drops markedly, resulting in greater flow than with a Newtonian fluid. The reason is unclear, but may involve ‘plasma skimming’ (the tendency of cellular components of blood to remain in the middle of vessels whilst plasma passes into branches arising from the vessel wall). Blood cell deformability may also be important. At very low blood flow, viscosity increases as the cells clump together.
Relative viscosity (compared with water) of normal plasma is 1.5; that of normal whole blood is 3.5.
Vishnevskiy technique (Transverse injection anaesthesia). Injection of local anaesthetic agent into a transverse ‘slice’ of a limb; originally described using procaine. Infiltration is performed from skin to bone, using large volumes of agent. Has been called the ‘squirt and cut’ technique.
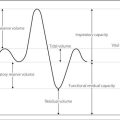
Vital capacity. The maximum volume of gas that can be expired slowly after maximal inspiration; measured by a spirometer. Reduced in the supine position. Also reduced in the elderly, and in patients with restrictive lung disease, muscle weakness, abdominal swelling and pain.
See also, Forced vital capacity; Lung function tests; Lung volumes
Vitamin B12 (Cobalamin). Water-soluble vitamin present in many animal tissues, especially eggs and liver. Exists as various related compounds, e.g. hydroxo- or cyanocobalamin. Combines with gastric intrinsic factor, enabling its absorption from the terminal ileum. Required for red blood cell maturation and as a cofactor for methionine synthase. Deficiency may be caused by failure of intrinsic factor production due to atrophic gastritis (pernicious anaemia) or gastric resection, or by disease/resection of the ileum. Dietary deficiency is rare. Inhibited by N2O. Deficiency results in macrocytic megaloblastic anaemia and subacute combined degeneration of the spinal cord.
Administered im 3-monthly as hydroxocobalamin; cyanocobalamin requires more frequent administration. Also used in the treatment of cyanide poisoning.
Vitamin deficiency. May occur in:
 inadequate intake relative to requirements, e.g. malnutrition (including inadequate provision during TPN).
inadequate intake relative to requirements, e.g. malnutrition (including inadequate provision during TPN).
 malabsorption, e.g. due to gastric disease (vitamin B12), pancreatic disease (fat-soluble vitamins: A, D, E and K).
malabsorption, e.g. due to gastric disease (vitamin B12), pancreatic disease (fat-soluble vitamins: A, D, E and K).
 impaired metabolism of precursors, e.g. osteomalacia in renal failure.
impaired metabolism of precursors, e.g. osteomalacia in renal failure.
 antagonism by drugs, e.g. warfarin (vitamin K), N2O (folate and vitamin B12).
antagonism by drugs, e.g. warfarin (vitamin K), N2O (folate and vitamin B12).
• Specific deficiency states of possible anaesthetic importance:
 vitamin A: night blindness, dry skin.
vitamin A: night blindness, dry skin.
 vitamin B1 (thiamine): peripheral neuropathy, Wernicke’s syndrome (ataxia, nystagmus, ophthalmoplegia and encephalopathy), cardiomyopathy (beriberi). May accompany chronic alcoholism. Vitamin B1 is used in ethylene glycol poisoning.
vitamin B1 (thiamine): peripheral neuropathy, Wernicke’s syndrome (ataxia, nystagmus, ophthalmoplegia and encephalopathy), cardiomyopathy (beriberi). May accompany chronic alcoholism. Vitamin B1 is used in ethylene glycol poisoning.
 vitamin B2 (riboflavin): anaemia, mouth lesions.
vitamin B2 (riboflavin): anaemia, mouth lesions.
 vitamin B6 (pyridoxine): convulsions, anaemia. May accompany chronic alcoholism. Vitamin B6 is used in ethylene glycol poisoning and isoniazid therapy.
vitamin B6 (pyridoxine): convulsions, anaemia. May accompany chronic alcoholism. Vitamin B6 is used in ethylene glycol poisoning and isoniazid therapy.
 niacin: dermatitis, diarrhoea, dementia (pellagra).
niacin: dermatitis, diarrhoea, dementia (pellagra).
 vitamin B12: anaemia, subacute combined degeneration of the cord.
vitamin B12: anaemia, subacute combined degeneration of the cord.
 vitamin C: generalised bleeding (especially gums), anaemia, weakness, poor wound healing (scurvy).
vitamin C: generalised bleeding (especially gums), anaemia, weakness, poor wound healing (scurvy).
 vitamin D: hypocalcaemia, hyperphosphataemia, muscle weakness, rickets (in children), osteomalacia (in adults).
vitamin D: hypocalcaemia, hyperphosphataemia, muscle weakness, rickets (in children), osteomalacia (in adults).
 vitamin E: haemolysis, oedema.
vitamin E: haemolysis, oedema.
Vitamin K. Fat-soluble group of vitamins that catalyse the carboxylation of glutamic acid residues to activate coagulation factors II, VII, IX and X. Deficiency results in increased tendency to bleed and may result from:
 inadequate intake: rare in adults, common in the newborn.
inadequate intake: rare in adults, common in the newborn.
 inadequate absorption, e.g. malabsorption syndromes, biliary obstruction.
inadequate absorption, e.g. malabsorption syndromes, biliary obstruction.
 inadequate utilisation, e.g. liver disease.
inadequate utilisation, e.g. liver disease.
 drug therapy: especially warfarin and similar drugs, which act as vitamin K antagonists.
drug therapy: especially warfarin and similar drugs, which act as vitamin K antagonists.
Anaphylaxis has been reported.
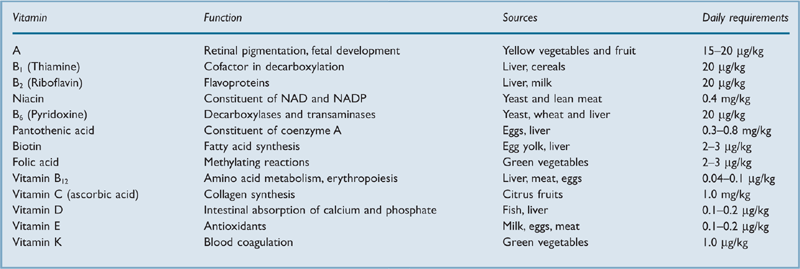
Vitamins. Term derived from ‘vital amines’. Group of dietary compounds necessary for health and growth but which do not supply energy (Table 43). Lack of one or more produces vitamin deficiency states. Vitamins A, D, E and K are fat-soluble; the rest are water-soluble.
Volatile anaesthetic agents, see Inhalational anaesthetic agents
Volt. Unit of electrical potential. One volt is the potential difference between two points when 1 joule of work is done per coulomb of electricity passing from one point to the other.
Volume of distribution (Vd). Theoretical term indicating the degree to which a drug redistributes and/or accumulates in body tissues. Equals the ratio of the amount of drug present in the body at a given time, to the concentration of the drug in plasma at that time. Alternatively described as the volume of plasma throughout which an injected dose would have to be distributed in order to give the measured plasma concentration. May be used to estimate the loading dose required to achieve a desired plasma concentration, e.g. in a target-controlled infusion.
Examples (approximate values for a 70 kg man):
Drugs or poisons with a small Vd are more readily cleared from the plasma by haemodialysis or haemoperfusion; those with large Vd may be cleared from the plasma but levels tend to rise again (with possible recurrence of toxic effects) following cessation of dialysis.
Volume support, see Inspiratory volume support
Volutrauma, see Ventilator-associated lung injury
Vomiting. Reflex involving retrograde passage of gastric contents through the mouth. The vomiting centre in the lateral medullary reticular formation receives afferent impulses from the:
 GIT, abdominal organs and peritoneum via the vagus and sympathetic nerves.
GIT, abdominal organs and peritoneum via the vagus and sympathetic nerves.
 heart mainly via the vagus nerve.
heart mainly via the vagus nerve.
 chemoreceptor trigger zone (CTZ).
chemoreceptor trigger zone (CTZ).
Chemical irritants stimulate the vomiting centre via receptors in the GIT. Drugs (e.g. apomorphine) and neurotransmitters (e.g. dopamine, noradrenaline, acetylcholine, 5-HT) stimulate the CTZ. Raised ICP is thought to cause vomiting via increased pressure on the floor of the fourth ventricle.
Motor impulses travel through cranial nerves V, VII, IX, X and XII to the facial muscles and upper GIT and through spinal nerves to the diaphragm and abdominal muscles.
Nausea is a sensation that may or may not be associated with the act of vomiting itself, although the two are usually considered together since the neurological pathways are similar. The incidence of PONV has been found to vary from 15 to 90%. Usually distressing, it is particularly undesirable in ear and ophthalmic surgery, and neurosurgery.
• Effects of prolonged vomiting:
 loss of water and hydrogen, chloride, potassium and sodium ions, causing metabolic alkalosis.
loss of water and hydrogen, chloride, potassium and sodium ions, causing metabolic alkalosis.
 renal bicarbonate loss to restore pH, causing alkaline urine.
renal bicarbonate loss to restore pH, causing alkaline urine.
 fall in sodium and ECF causing aldosterone release, which causes renal sodium and fluid retention, in exchange for potassium and hydrogen ions. If hypokalaemia is severe, hydrogen ion loss predominates, with paradoxical acid urine.
fall in sodium and ECF causing aldosterone release, which causes renal sodium and fluid retention, in exchange for potassium and hydrogen ions. If hypokalaemia is severe, hydrogen ion loss predominates, with paradoxical acid urine.
 thus dehydration, metabolic alkalosis and total body potassium depletion may occur.
thus dehydration, metabolic alkalosis and total body potassium depletion may occur.
Von Recklinghausen’s disease, see Neurofibromatosis
Von Willebrand’s disease. Commonest inherited coagulation disorder (affects ~1:100–1000 people but may be very mild); first described in 1926, with mostly autosomal dominant transmission, depending on the subtype. Abnormality of von Willebrand factor (VWF), a protein involved in platelet adhesion and carriage of coagulation factor VIII, leads to factor VIII deficiency, abnormal platelet adhesiveness and abnormal vascular endothelium. Epistaxis and bruising are more common than haemarthrosis and haematoma, although there is marked variation in clinical severity.
• Classified into three main types:
 type 1: quantitative reduction in VWF; accounts for ~90% of cases.
type 1: quantitative reduction in VWF; accounts for ~90% of cases.
 type 3: similar to type 1 but a severe autosomal recessive form; accounts for <1% of cases.
type 3: similar to type 1 but a severe autosomal recessive form; accounts for <1% of cases.
Definitive diagnosis is made via VWF activity assay, VWF antigen testing and factor VIII assay; in combination these have high sensitivity and specificity but may not be readily available, e.g. for emergency surgery. Routine coagulation studies are more accessible, but less useful for diagnosis:
Desmopressin boosts levels of factor VIII and VWF, and may be used preoperatively (0.3 µg/kg iv, effects lasting 6–8 h) for treatment of mild type 1 and 2A disease. Severe disease is treated with fresh frozen plasma, cryoprecipitate or specific factor concentrates before surgery. Tranexamic acid 1 g orally may be useful. Antiplatelet drugs must be avoided.
During pregnancy, levels of factor VIII and VWF increase, but they may fall rapidly after delivery.
[Erik von Willebrand (1870–1949), Swedish physician]
Voriconazole. Broad-spectrum triazole antifungal drug, related to fluconazole and used for severe fungal infections.
 mismatch, see Ventilation/perfusion mismatch
mismatch, see Ventilation/perfusion mismatch