Chapter 30 Uvulopalatopharyngoplasty – effects on the airway
1 HISTORY OF UVULOPALATOPHARYNGOPLASTY
Uvulopalatopharyngoplasty (UPPP) was first described by Fujita in 1981. It represented the first surgical procedure specifically designed to treat obstructive sleep apnea (OSA).1 Fujita modified an earlier procedure applied by Ikematsu as a treatment for snoring.
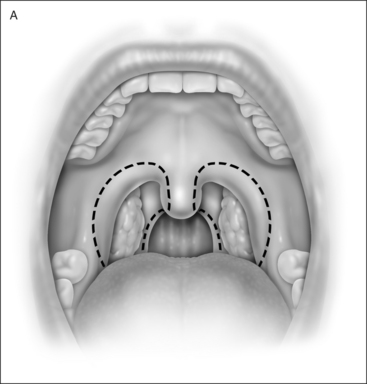
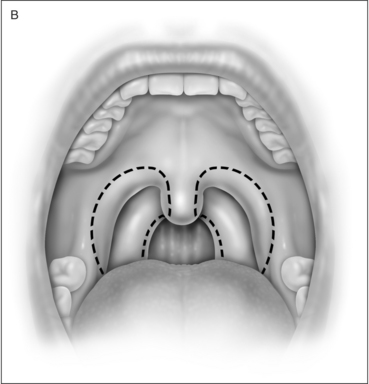
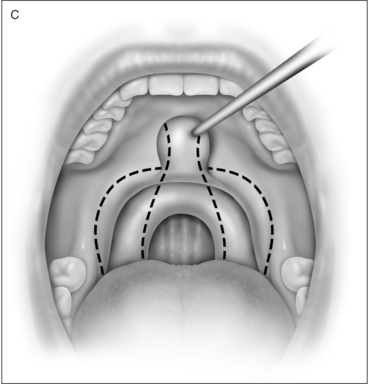
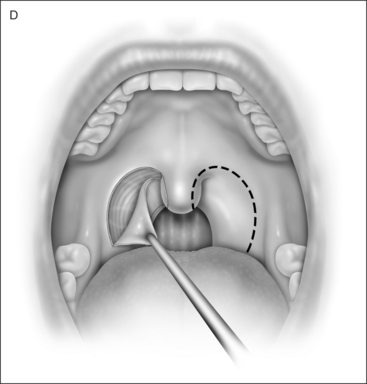
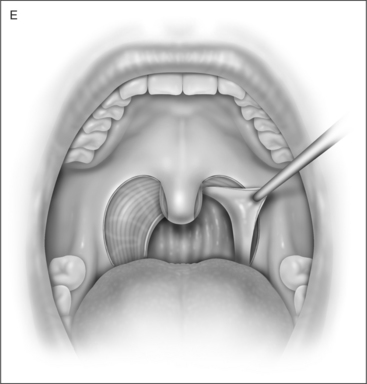
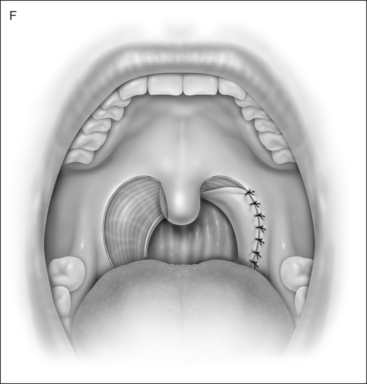
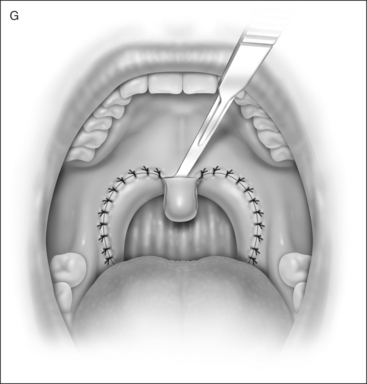
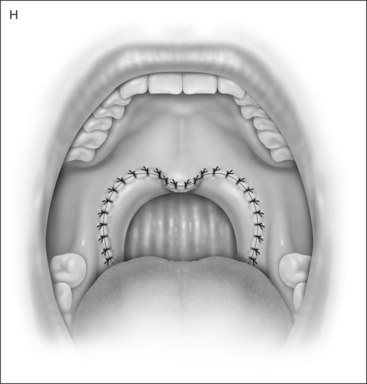
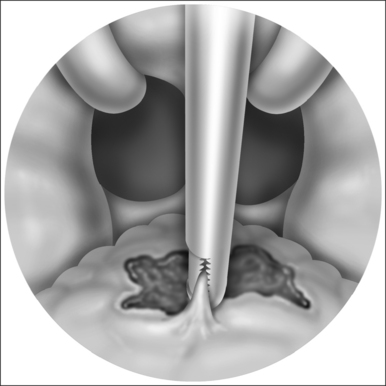
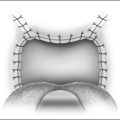
UPPP enlarges the retropalatal airway by excision of the tonsils (if not previously extirpated), trimming and reorienting the posterior and anterior tonsillar pillars, and excising the uvula and posterior portion of the soft palate (Fig. 30.1). A number of modifications of Fujita’s procedure were described shortly after his publication, but none has clearly improved outcome, nor become the predominant technique.2 However, more recent modifications seem promising: UPPP with creation of a uvulopalatal flap in lieu of extirpation of the uvula and posterior soft palate;3 tonsil reduction by coblation (rather than tonsillectomy) combined with a palatal flap technique.4 Different surgical tools can be applied to achieve UPPP, such as electrocautery vs. scalpel.5 UPPP can include tonsillectomy, but can also be performed in a patient previously tonsillectomized.6 A procedure described as lateral pharyngoplasty focuses on splinting the lateral pharyngeal walls through microdissection of the superior pharyngeal constrictor muscles within the tonsillar fossa, sectioning this muscle, and suturing the laterally based
flap consisting of that muscle to the same side palatoglossus muscle. A palatopharyngeal Z-plasty is performed to prevent retropalatal collapse.7,8 Laser-assisted uvulopalatoplasty (LAUP) is performed with laser, under topical and local anesthesia, without tonsillectomy. Though it may (in some cases) be applied in treatment for OSA, particularly in previously tonsillectomized patients, LAUP is not generally included among the surgical armamentaria for OSA, but rather for snoring.9
2 UPPP: THE PROCEDURE
3 WHY DOES UPPP WORK?
Structurally, the dorsum of the tongue is anterior to the soft palate. The dorsum of the tongue may push the anterior wall of the soft palate posteriorly during obstructive events (maintaining closure of the retropalatal airway). Depending upon specifics of pharyngeal anatomy, there is dynamic interaction between the tongue and soft palate during obstructive apnea, reflecting an abnormally highly collapsible airway at the retropalatal level.10 A model of the upper airway in OSA syndrome (OSAS) likens it to a simple collapsible tube. The tendency of the upper airway to collapse can be expressed quantitatively in terms of a critical pressure (Pcrit), defined as the pressure surrounding the focus of collapse. If atmospheric pressure is designated zero, then airway collapse will occur whenever Pcrit is a positive number (indicating that it is higher than atmospheric pressure). Pcrit levels are higher during sleep than during wakefulness in both normal individuals and OSAS patients. In normals, Pcrit rises from awake values that are more negative than −41 cm H2O to values in sleep of −13 cm H2O.11–13 This means that, in normals, atmospheric pressure is greater than Pcrit even during sleep and the pharynx will not collapse. In OSAS patients, the spectrum of awake values of Pcrit is −40 cm H2O to −17 cm H2O and Pcrit during sleep is +2.5 cm H2O.11,12,14,15 Although the pharyngeal airway of awake OSAS patients tends to be more collapsible than that of awake normals, Pcrit does not cross the critical line of zero (i.e. atmospheric pressure) except when the individual with OSAS has sleep onset, at which time an obstructive event results.11 Patients who have varying degrees of partial pharyngeal collapse have intermediate, but negative, levels of Pcrit during sleep: −6.5 cm H2O for asymptomatic snorers and −1.6 cm H2O for patients with hypopneas but no apneas.11,15 In general, Pcrit must be below −5 cm H2O to eliminate obstructive sleep disordered breathing.11 Pcrit for an OSAS patient can, alternatively, be defined as the lowest level of nasal continuous positive airway pressure (CPAP) at which airflow is maintained.16 Examples of the decrement in Pcrit that can be achieved by non-surgical interventions are −6 cm H2O through loss of 15% of body weight; −3 to −4 cm H2O through protriptyline treatment; and −4 to −5 cm H2O through the avoidance of sleeping in the supine position.11 Pcrit decrement resulting from upper airway surgery has been documented for UPPP. When 13 patients undergo UPPP, Pcrit decreases from a level of 0 to a level of –3 cm H2O (P=0.016). In those patients who have greater than 50% decrease in Respiratory Disturbance Index (RDI) in non-REM sleep, Pcrit decreases from −1 to −7 cm H2O (P=0.01). The degree of improvement in sleep disordered breathing is correlated significantly with the change of Pcrit (P=0.001), and the decrease in RDI is determined by the magnitude of the drop in Pcrit rather than by the initial level of Pcrit. No significant change in Pcrit is detected in non-responders.16,17 In a study performed under anesthesia and induced paralysis, 18 patients were analyzed for retropalatal pharyngeal closing pressure before and 3 months and 1 year after UPPP. UPPP decreased retropalatal airway closing pressure by 3.5 cm H2O. A direct correlation existed between the severity of OSA and retropalatal airway closing pressure. Patients who failed at UPPP had postoperative retropalatal airway closing pressure greater than zero. Reduced retropalatal airway collapsibility was maintained up to 1 year after UPPP.10,18
4 WHY DOES UPPP FAIL TO CORRECT OSAS, AND WHY DO SALVAGE PROCEDURES WORK?
The likely explanation is that upper airway collapsibility has been inadequately addressed. The degree of improvement in severity of OSAS is correlated significantly with the change in Pcrit (P=0.001). The decrease in RDI is determined by the magnitude of the fall in Pcrit. No significant change in Pcrit is detected in non-responders. UPPP failures reveal retropalatal airway closing pressure greater than zero.10,16–18 Alternative (not mutually exclusive) explanations for UPPP failure are: (1) UPPP does not address all sites of narrowing or collapse; or (2) UPPP addresses sites of narrowing or collapse in an inadequate manner. Evidence for these explanations has been documented through application of upper airway manometry, measurement of pharyngeal cross-sectional area, videoendoscopy, and cephalometry.19–22 Further evidence comes from clinical experience. Surgical modification of the upper airway at sites other than those addressed by UPPP may salvage UPPP failures. Thus, procedures believed to diminish collapsibility of the retrolingual airway (unlike UPPP which addresses primarily the retropalatal airway) may achieve surgical salvage after UPPP failure. These procedures include: mandibular advancement, laser midline glossectomy, lingualplasty, radiofrequency tongue base ablation, genioglossal advancement and hyoid myotomy and suspension. Maxillomandibular advancement enlarges the retropalatal and retrolingual airway and may achieve surgical salvage after failure of various combinations of UPPP and the other procedures outlined above.16,23 On the other hand, additional surgical modification of the palate (addressing the retropalatal airway, as does UPPP) also salvages UPPP failures. Transpalatal advancement pharyngoplasty (TPAP) increases the retropalatal airway size by excising posterior hard palate and advancing the soft palate. Sequential performance of TPAP after UPPP results in incremental decrease in Pcrit to a level below that resulting from UPPP alone. When four patients underwent TPAP after previous UPPP, mean post-UPPP Pcrit of 5 was decreased to –4 after TPAP (P<0.01). TPAP increased the post-UPPP retropalatal airway cross-sectional area from 30 to 95 cm2 (P<0.01).24 Other studies have demonstrated that the degree of improvement in OSAS is correlated significantly with the change of Pcrit (P=0.001), and the decrease in RDI is determined by the magnitude of the fall in Pcrit.13 It is likely that each surgical procedure successfully decreasing OSAS severity results in decreased Pcrit, and that procedures performed concomitantly or in sequence (at a single or at multiple sites of airway narrowing/collapse) result in incremental decreases in Pcrit. Further data are needed for confirmation.11
5 WHAT ARE LONG-TERM POLYSOMNOGRAPHY OUTCOMES OF UPPP?
Efficacy of UPPP may diminish over time: 60% success (defined as RDI diminished by 50%) at mean of 6 months postoperatively declined to 50% at mean of 46 months postoperatively. Success of 64% (defined as RDI diminished by 50% and postoperative RDI < 10 apneas and hypopneas per hour) at mean of 6 months postoperatively declined to 48% at mean 48–96 months postoperatively. Success of 67% (defined as RDI diminished by 50%) at 3–6 months postoperatively declined to 33% at mean of 88 months post-operatively. Weight gain was implicated as an explanation for long-term recurrence in some, but not all cases.25–27
6 CAN PATIENT SELECTION IMPACT UPPP OUTCOME?
Lateral cephalometry and fiberoptic endoscopy have been widely applied for preoperative characterization of the pharyngeal airway (as Type 1, 2, or 3) and, hence, as a method of patient selection. The assumption was that Type 1 patients were favorable for UPPP, whereas Types 2 and 3 were not. The original goal of patient characterization was to permit selection of a candidate pool for UPPP who would exceed the 50% success rate (PSG criteria) reported in the literature. Neither of these approaches has been clearly documented to be an effective screening tool. Indeed, different investigators have widely different degrees of success predicting UPPP success through application of fiberoptic endoscopy and lateral cephalometry.23,28–38 Weaknesses of each technique are readily apparent. Both are applied in the awake patient, while OSAS occurs only in the asleep patient. Both are generally applied in a sitting position, while the sleeping patient is generally not in this position. Lateral cephalometry is adynamic and assesses the airway in only two dimensions, while airway collapse in OSAS is dynamic and occurs in three dimensions. Endoscopic data are highly subjective and dependent on observer interpretation, while the quality of cephalometric films can be variable and dependent on attention to detail in shooting. Nonetheless, pharyngeal classification into Types 1–3 by techniques including fiberoptic endoscopy and lateral cephalometry permitted identification of two subgroups with markedly different UPPP success rates: 52% success for Type 1 and 5% for types 2 and 3.23 It also provided the basis for development of new surgical procedures designed to salvage UPPP failures. Several reports document OSAS cure rates (by PSG criteria) close to 100%, achieved by complex upper airway modification utilizing these procedures. Depending upon the complexity of anatomical compromise, one or multiple procedures may be required.39–42 However, the pharyngeal classification system does not explain failure of UPPP in 48% of patients classified as Type 1. It is likely that nuances of pharyngeal anatomy and function are not discriminated by these techniques of evaluation. Alternatively, lack of consistency in interpretation of endoscopic data may be a consequence of its subjective nature, and interpretation of cephalometric views may be compromised by lack of attention to detail in execution and interpretation of cephalometric analysis. Studies comparing fiberoptic endoscopy with pharyngeal manometry (awake and asleep) demonstrate disagreement between these techniques in identifying pharyngeal dynamics as well as discrepancies in observation with the same technique applied in wakefulness and in sleep.19,37,38 An alternative approach to prognostic classification of patients being considered for UPPP was introduced. A total of 134 patients were retrospectively classified by means of a staging system which included: (a) palate position in relationship to tongue (b) tonsil size, and Body Mass Index (BMI). This staging system did correlate success of UPPP based on postoperative PSG results with palate position and tonsil size (Table 30.1). Success rate for Stage I was 81%, for Stage II was 37%, and for Stage III was 8%. Success was defined as reduction of the RDI by at least 50% to an RDI less than 20 apneas and hypopneas per hour. Statistical analysis demonstrated a highly significant relationship between Friedman stage and success of surgery (P<0.0001). Friedman further explored the relationship between stage and the efficacy of UPPP, applying stepwise multivariate discriminant analysis. Preoperative criteria used to stratify patients into stages (BMI, tonsil size and palate position) were the only indices introduced into the stepwise analysis. Success or failure of surgical treatment with UPPP was used as the categorical endpoint. Friedman derived equations with representation of tonsil size and palate position which permitted correct outcome in 95% of 134 patients.43 It was subsequently demonstrated that preoperative application of a modified version of this staging paradigm permitted improvement of surgical outcomes through application of UPPP with additional surgical intervention aimed at the retrolingual area in patients having an unfavorable prognostic prediction for UPPP as a sole procedure.44
1. Fujita S, Conway W, Zorick F, et al. Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981;89:923-934.
2. Ikematsu T, Fujita S, Simmons BF, et al. Uvulopalatopharyngoplasty: variations. In Fairbanks DNF, Fujita S, editors: Snoring and Obstructive Sleep Apnea, 2nd edn, New York: Raven Press, 1994.
3. Powell N, Riley R, Guilleminault C, et al. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep. 1996;19:593-599.
4. Friedman M, Ibrahim H, Lowenthal S, et al. Uvulopalatoplasty (UP2): a modified technique for selected patients. Laryngoscope. 2004;114:441-449.
5. Altman JS, Senior B, Ransom E. The effect of electrocautery vs. cold scalpel technique on the incidence of early postoperative tonsillar pillar dehiscence after uvulopalatopharyngoplasty with tonsillectomy. Laryngoscope. 2004;114:294-296.
6. McGuirt WFJr., Johnson JT, Sanders MH. Previous tonsillectomy as prognostic indicator for success of uvulopalatopharyngoplasty. Laryngoscope. 1995;105:1253-1255.
7. Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 2003;113:1961-1968.
8. Cahali MB, Formigoni GG, Gebrim EM, et al. Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep. 2004;27:942-950.
9. Littner M, Kushida CA, Hartse K, et al. Practice parameters for the use of laser-assisted uvulopalatoplasty: an update for 2000. Sleep. 2000;24:603-619.
10. Isono S, Shimada A, Tanaka A, et al. Effects of uvulopalatopharyngoplasty on collapsibility of the retropalatal airway in patients with obstructive sleep apnea. Laryngoscope. 2003;113:362-367.
11. Winokur SJ, Smith PL, Schwartz AR. Pathophysiology and risk factors for obstructive sleep apnea. Semin Resp Crit Care Med. 1998;19:999-1112.
12. Suratt PM, Wilhoit SC, Cooper K. Induction of airway collapse with subatmospheric pressure in awake patients with sleep apnea. J Appl Physiol. 1984;57:140-146.
13. Schwartz AR, Smith PL, Wise RA, et al. Induction of upper airway occlusion in sleeping individuals with subatmospheric pressure in awake patients with sleep apnea. J Appl Physiol. 1988;64:535-542.
14. Horner RL, Mohiaddin RH, Lowell DG, et al. Sites and sizes of fat deposits around the pharynx in obese patients with obstructive sleep apnoea and weight matched controls. Eur Resp J. 1989;2:6113-6122.
15. Gleadhilll IC, Schwartz AR, Schubert OI, et al. Upper airway collapsibility in snorers and in patients with obstructive hypopnea and apnoea. Am Rev Respir Dis. 1991;143:1300-1303.
16. Sher AE. Upper airway surgery for obstructive sleep apnea. Sleep Med Rev. 2002;6:195-212.
17. Schwartz AR, Schiebert N, Rothman W, et al. Effect of uvulopalatopharyngoplasty on airway collapsibility in obstructive sleep apnea. Am Rev Respir Dis. 1992;145:522-532.
18. Isono S, Tanaka A, Nishino T. Dynamic interaction between the tongue and soft palate during obstructive apnea in anesthetized patients with sleep disordered breathing. J Appl Physiol. 2003;95:2257-2264.
19. Sher AE. Soft tissue surgery for obstructive sleep apnea syndrome. Semin Resp Crit Care Med. 1998;19:165-173.
20. He J, Kryger M, Zorick F, et al. Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest. 1988;94:9-14.
21. Guilleminault C, Stoohs R, Clerk A, et al. A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest. 1993;104:7810-7817.
22. Osnes T, Rollheim J, Hartmann E. Effect of UPPP with respect to site of pharyngeal obstruction in sleep apnoea: follow-up at 18 months by overnight recording of airway pressure and flow. Clin Otolaryngol Allied Sci. 2002;27:38-43.
23. Sher AE, Schechtman KB, Piccirrillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19:156-177.
24. Woodson BT. Retropalatal airway characteristics in uvulopalatopharyngoplasty compared with tranpalatal advancement pharyngoplasty. Laryngoscope. 1997;107:735-740.
25. Larsson LH, Carlsson-Nordlander B, Svanborg E. Four-year follow-up after uvulopalatopharyngoplasty in 50 unselected patients with obstructive sleep apnea syndrome. Laryngoscope. 1994;104:1362-1368.
26. Janson C, Gislason T, Bengtsson H, et al. Long term follow-up of patients with obstructive sleep apnea treated with uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg. 1997;123:257-262.
27. Lee S-J, Chong S-Y, Shiao G-M. Comparison between short-term and long-term post-operative evaluation of sleep apnoea after uvulopalatopharyngoplasty. J Laryngol Otol. 1995;109:308-312.
28. Hessel NS, de Vries N. Results of uvulopalatopharyngoplasty after diagnostic workup with polysomnography and sleep endoscopy: a report of 136 snoring patients. Eur Arch Otorhinolaryngol. 2002;260:91-95.
29. Millman RP, Carlisle CC, Rosenberg C, et al. Simple predictors of uvulopalatopharyngoplasty outcome in the treatment of obstructive sleep apnea. Chest. 2000;118:1025-1030.
30. Boot H, Poublon RM, Van Wegen R, et al. Uvulopalatopharyngoplasty for the obstructive sleep apnea syndrome: value of polysomnography, Mueller manoeuvre and cephalometry in predicting surgical outcome. Clin Otolaryngol Allied Sci. 1997;22:504-510.
31. Woodson BT, Conley SF. Prediction of uvulopalatopharyngoplasty response using cephalometric radiographs. Am J Otolaryngol. 1997;18:179-184.
32. Woodson BT, Conley SF, Dohse A, et al. Posterior cephalometric radiographic analysis in obstructive sleep apnea. Ann Otol Rhinol Laryngol. 1997;106:310-313.
33. Aboussouan LS, Golish JA, Wood BG, et al. Dynamic pharyngoscopy in predicting outcome of uvulopalatopharyngoplasty for moderate and severe obstructive sleep apnea. Chest. 1995;107:946-951.
34. Doghramji K, Jabourian AH, Pilla M, et al. Predictors of outcome for uvulopalatopharyngoplasty. Laryngoscope. 1995;105:311-314.
35. Petri N, Suadicani P, Wildschiodtz G, et al. Predictive value of Muller maneuver, cephalometry, and clinical features for the outcome of uvulopalatopharyngoplasty. Acta Otolaryngol (Stockh). 1994;114:565-575.
36. Sher AE, Thorpy MJ, Shprintzen RJ, et al. Predictive value of Muller maneuver in selection of patients for uvulopalatopharyngoplasty. Laryngoscope. 1985;95:1483-1487.
37. Woodson BT, Wooten MR. Comparison of upper airway evaluation during wakefulness and sleep. Laryngoscope. 1994;104:821-828.
38. Skatvedt O. Localization of site of obstruction in snorers and patients with obstructive sleep apnea syndrome: a comparison of fiberoptic nasopharyngoscopy and pressure measurements. Acta Otolaryngol (Stockh). 1993;113:206-209.
39. Chabolle F, Wagner I, Blumen M, et al. Tongue base reduction with hyoepiglottoplasty: a treatment for severe obstructive apnea. Laryngoscope. 1999;109:1273-1280.
40. Riley RW, Powell NB, Guilleminault C, et al. Obstructive sleep apnea syndrome: a review of 306 consecutively treated surgical patients. Otolaryngol Head Neck Surg. 1993;108:117-125.
41. Troell RJ, Powell JB, Riley RW. Hypopharyngeal airway surgery for obstructive sleep apnea syndrome. Semin Resp Crit Care Med. 1998;19:175-183.
42. Prinsell JR. Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients. Chest. 1999;116:1519-1529.
43. Friedman M, Ibrahim H, Bass C. Clinical staging for sleep disordered breathing. Otolaryngol Head Neck Surg. 2002;127:13-21.
44. Friedman M, Ibrahim H, Joseph N. Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope. 2004;114:454-459.
45. American Academy of Sleep Medicine Task Force on Sleep Related Breathing Disorders in Adults. Recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;5:667-689.
46. Boudewyns A, DeCock W, Willemen M, et al. Influence of UPPP on alpha-EEG arousals in nonapnoeic snorers. Eur Respir J. 1997;10:129-132.
47. Esclamado RM, Glenn MG, McCulloch TM, et al. Perioperative complications and risk factors in the surgical treatment of obstructive sleep apnea syndrome. Laryngoscope. 1989;99:1125-1129.
48. Farmer WC, Giudici SC. Site of airway collapse in obstructive sleep apnea after uvulopalatopharyngoplasty. Ann Otol Rhinol Laryngol. 2000;109:581-584.
49. Haavisto L, Suonpaa J. Complications of uvulopalatopharyngoplasty. Clin Otolaryngol. 1994;19:243-247.
50. Haraldsson P.-O, Carenfelt C, Lysdahl M, et al. Does uvulopalatopharyngoplasty inhibit automobile accidents? Laryngoscope 1995;105:657–661.
51. Keenan SP, Heather B, Ryan CF, et al. Long-term survival of patients with obstructive sleep apnea treated by uvulopalatopharyngoplasty or nasal CPAP. Chest. 1994;105:155-159.
52. Kezirian EJ, Weaver EM, Yuch B, et al. Risk factors for serious complication after uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg. 2006;132:1091-1098.
53. Langin T, Pepin JL, Pendlebury S, et al. Upper airway changes in snorers and mild sleep apnea sufferers after uvulopalatopharyngoplasty (UPPP). Chest. 1998;113:1595-1603.
54. Li HY, Lee LA, Wang PC, et al. Taste disturbance after uvulopalatopharyngoplasty for obstructive sleep apnea. Otolaryngol Head Neck Surg. 2006;134:985-990.
55. Lysdahl M, Haraldsson P-O. Long-term survival after UPPP in non-obese heavy snorers. Arch Otolaryngol Head Neck Surg. 2000;126:1136-1140.
56. Marti S, Sampol G, Munoz X, et al. Mortality in severe sleep apnoea hypopnea syndrome patients: impact of treatment. Eur Respir J. 2002;20:1511-1518.
57. Mickelson SA, Hakim I. Is postoperative intensive care monitoring necessary after uvulopalatopharyngoplasty? Otolaryngol Head Neck Surg. 1998;119:352-356.
58. Milljetieg H, Mateika S, Haight JS, et al. Subjective and objective assessment of uvulopalatopharyngoplasty for treatment of snoring and obstructive sleep apnea. Am J Respir Crit Care Med. 1994;150:1286-1290.
59. Mortimer IL, Bradley PA, Murray JA, et al. Uvulopalatopharyngoplasty may compromise nasal CPAP therapy in sleep apnea syndrome. Am J Respir Crit Care Med. 1996;154:1759-1762.
60. Peker Y, Hedner J, Norum J, et al. Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. Am J Respir Crit Care Med. 2002;166:159-165.
61. The International Classification of Sleep Disorders: Diagnostic and Coding Manual, 2nd edn. Westchester, IL: AASM; 2005:51–3.
62. Weaver EM, Maynard C, Yueh B. Survival of veterans with sleep apnea: continuous positive airway pressure vs. surgery. Otolaryngol Head Neck Surg. 2004;130:659-665.
63. Weaver EM, Sher AE, in preparation.
64. Weaver EM, Woodson BT, Steward DL. Polysomnography indexes are discordant with quality of life, symptoms, and reaction times in sleep apnea patients. Otolaryngol Head Neck Surg. 2005;132:255-262.
65. Woodson BT, Wooten MR. Manometric and endoscopic localization of airway obstruction after uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1994;111:38-43.
66. Zohar Y, Finkelstein Y, Talmi YP, et al. Uvulopalatopharyngoplasty: evaluation of complications, sequelae, and results. Laryngoscope. 1991;101:775-779.
67. Zorick F, Roehrs T, Conway W, et al. Effects of uvulopalatopharyngoplasty on the daytime sleepiness associated with sleep apnea syndrome. Bull Europ Physiopath Resp. 1983;19:600-603.