Uterosacral Nerve Transection
Pain fibers emanating from the cervix and the lower portion of the uterine corpus traverse the uterosacral ligaments posteriorly to the sacrum and finally to the inferior hypogastric plexus (Fig. 39–1A, B). Section of these ligaments close to their origin at the junction of the upper vagina and the cervix has been advocated for the relief of dysmenorrhea. The operation does not relieve pain as completely as does presacral neurectomy. Nevertheless, uterosacral transection is a simpler operation to perform and usually is done via the laparoscopic approach.
The structures that must be identified to avoid injury are the right and left ureters and the uterine arteries. The latter are millimeters from the anterolateral aspect of the uterosacral ligaments. The former are within 1 to 2 cm of the ligaments (i.e., laterally located).
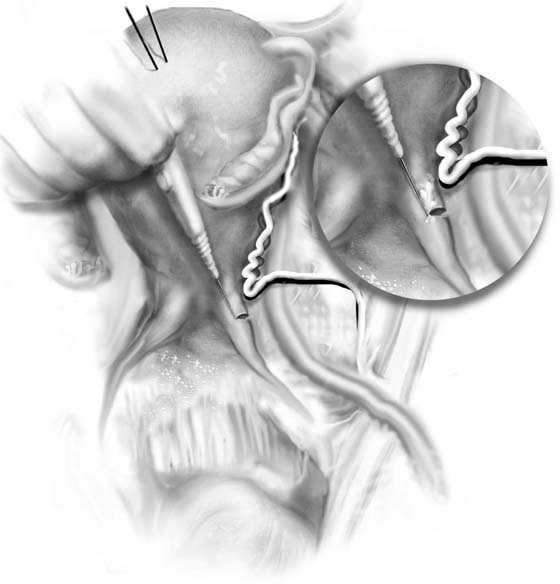
The uterosacral transection may be performed by laser ablation or by electrosurgical cutting. It is preferable to cut the ligament starting 1 to 2 mm from the lateral margin and to extend the cut medially toward the cul-de-sac (Fig. 39–2). The incision starts 4 to 5 mm distal from the locus where the ligament attaches to the uterus. The cut should be approximately 4 to 5 mm deep as well (Fig. 39–2, Inset). Some surgeons prefer to carry a 2-mm shallow incision across the posterior surface of the uterus, connecting the two severed uterosacral ligaments (Fig. 39–3).
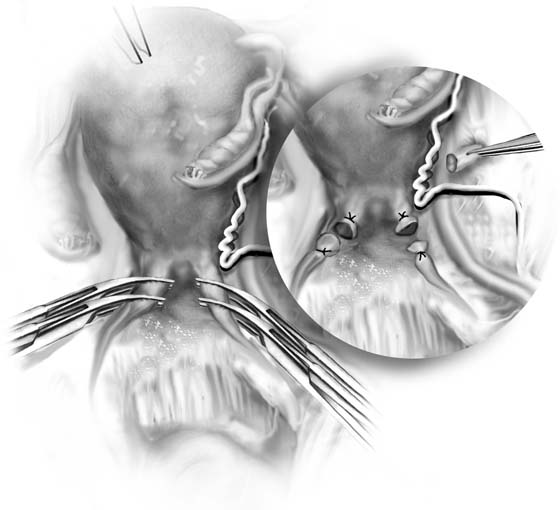
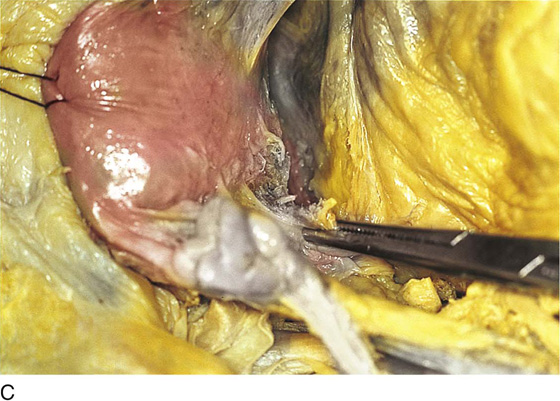
Alternatively, the ligament can be doubly clamped and incised, and each end suture-ligated with permanent sutures. A 5- to 10-mm chunk of ligament thus is excised and is sent to pathology in fixative (Figs. 39–4 through 39–6).
At the terminus of the procedure, bleeding points are checked and secured. The ureters are again examined to ensure their integrity.
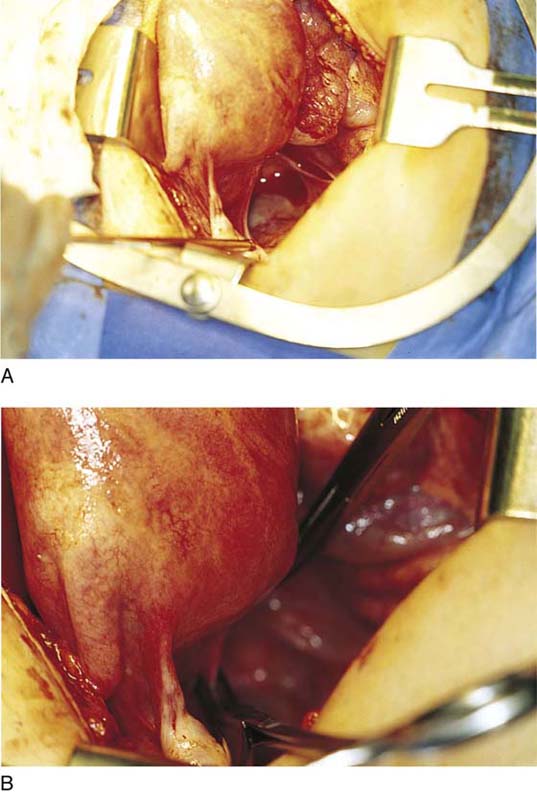
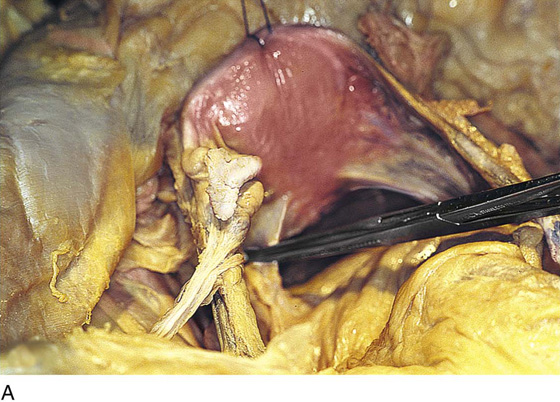
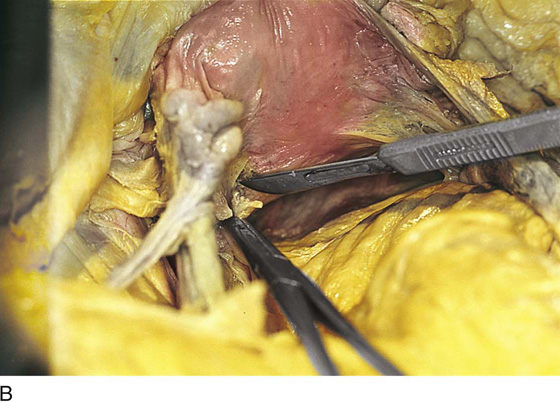
FIGURE 39–1 A. Normal uterus in situ. The left uterosacral ligament is grasped. B. Close-up of the same uterus as in Figure 39–1A. Pain fibers from the body of the uterus and the cervix are transmitted through the ligament, and pain is referred to the lower back via these fibers through the pelvic nerves and hypogastric plexus.
FIGURE 39–2 With an electrosurgical needle, the uterosacral ligament is transected. Note that the motion is from lateral to medial. The inset details the technique. Cutting current (blend one) at 30 to 40 W is applied at the lateral edge for short bursts to diminish conduction spread of thermal injury. Note that the ablation is initiated far enough posteriorly to avoid entry into the uterine artery. The sigmoid colon (medial) must be protected from conduction (electric current) injury.
FIGURE 39–3 The ablation is completed by continuing a 2- to 3-mm-deep extension across the back of the cervix (i.e., connecting the right and left uterosacral ablation lines).
FIGURE 39–4 Alternatively, the uterosacral ligaments may be clamped and cut. A segment of tissue (inset) may be sent to pathology to document excision and to determine whether any pathology exists within the ligament (e.g., endometriosis).
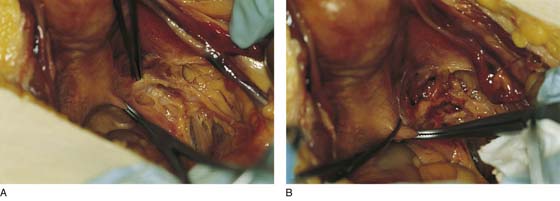
FIGURE 39–5 A. Actual application of the technique illustrated in Figure 34–4. B. The right uterosacral ligament is doubly clamped. The ureter has been identified lateral to the ligament.
FIGURE 39–6 A. Fixed cadaveric uterus with left uterosacral ligament clamped. B. A scalpel divides the uterosacral ligament close to its uterine insertion. C. The ligament is completely divided. The key to accurate isolation and sectioning of the uterosacral ligaments is tension. The best demonstration of the ligaments can be produced only by pulling the uterus upward (cranially) and sharply dissecting in the anterior direction, as illustrated here.