Chapter 11 Uterine Contractility and Dystocia
 Normal Labor
Normal Labor
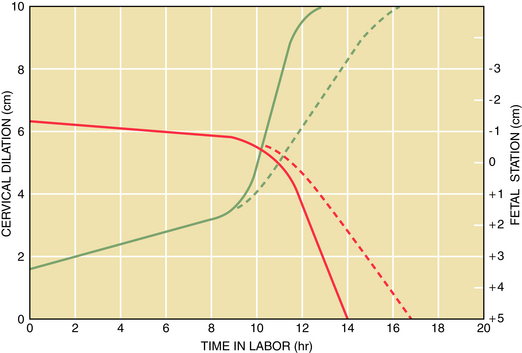
The early part, or latent phase, of labor is involved with softening and effacement of the cervix with minimal dilation. This is followed by a more rapid rate of cervical dilation, known as the active phase of labor, which is further divided into the acceleration (maximal slope) and deceleration phases. The descent of the fetal presenting part usually begins during the active phase of labor, then progresses at a more rapid rate toward the end of the active phase and continues after the cervix is completely dilated. A useful method for assessing the progress of labor and detecting abnormalities in a timely manner is to plot the rate of cervical dilation and descent of the fetal presenting part (Figure 11-1).
 Abnormalities of the Active Phase of Labor
Abnormalities of the Active Phase of Labor
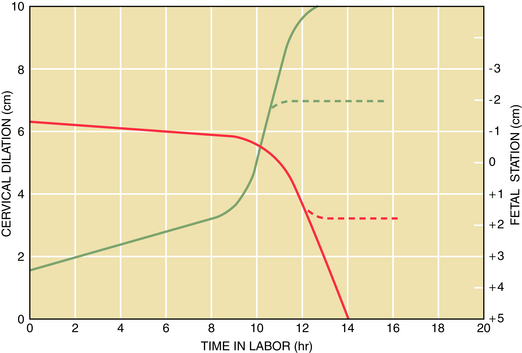
When the cervix dilates to about 3 to 4 cm, the rate of dilation progresses more rapidly. Cervical dilation of less than 1.2 cm/hour in nulliparous women and 1.5 cm in multiparous women constitutes a protraction disorder of the active phase of labor. During the latter part of the active phase, the fetal presenting part also descends more rapidly through the pelvis and continues to descend through the second stage of labor. A rate of descent of the presenting part of less than 1 cm/hour in nulliparous women and 2 cm/hour in multiparous women is considered to be a protraction disorder of descent (Figure 11-2). If a period of 2 hours or more elapses during the active phase of labor without progress in cervical dilation, an arrest of dilation has occurred; a period of more than 1 hour without a change in station of the fetal presenting part is defined as an arrest of descent (Figure 11-3).
DYSTOCIA CAUSED BY ABNORMAL PRESENTATION AND POSITION
Presentations other than vertex and positions other than occipitoanterior (OA) are considered to be abnormal in the laboring patient. Disorders of the dilation and descent phases of labor occur with increased frequency in cases of abnormal presentation or position because of the altered relationship between the presenting part of the fetus and the maternal pelvis. Fetal malpresentations are discussed further in Chapter 13.
DYSTOCIA CAUSED BY ABNORMALITIES OF FETAL STRUCTURE
DYSTOCIA CAUSED BY MATERNAL PELVIC ABNORMALITIES
Cephalopelvic disproportion (CPD) exists if the maternal bony pelvis is not of sufficient size and of appropriate shape to allow the passage of the fetal head. This problem may occur as a result of contraction of one of the planes of the pelvis. Relative CPD may exist with a normal pelvis, if the fetal head is excessively large or if it is in an abnormal position. Contraction of the maternal pelvis may occur at the level of the inlet or midpelvis, but contraction of the outlet is extremely unusual unless it is found in association with a midpelvic contraction (see Chapter 8).
DYSTOCIA CAUSED BY CONDUCTION ANESTHESIA
The use of epidural anesthesia for pain control during the first stage of labor has gained wide acceptance. Refinement of the epidural technique has allowed a segmental block and titratable continuous infusion of narcotics and local anesthetics to better tailor pain control, with less interference with the process of labor (see Chapter 8).
American College of Obstetricians and Gynecologists. Shoulder dystocia. Washington, DC: ACOG Practice Bulletin No. 40; 2002.
American College of Obstetricians and Gynecologists. Vaginal birth after previous cesarean section. Washington, DC: ACOG Practice Bulletin No. 54; 2004.
Gottlieb A.G., Galan H.L. Shoulder dystocia: An update. Obstet Gynecol Clin North Am. 2007;34:501-531. xii
Lowe N.K. A review of factors associated with dystocia and cesarean section in nulliparous women. J Midwifery Womens Health. 2007;52:216-228.
Shields S.G., Ratcliffe S.D., Fontaine P., Leeman L. Dystocia in nulliparous women. Am Fam Physician. 2007;75:1671-1678.

 Physiologic Changes of Labor
Physiologic Changes of Labor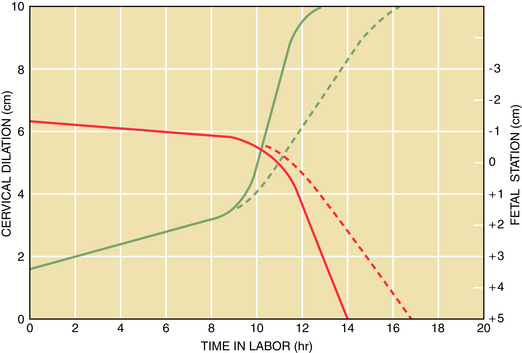
 Abnormalities of the Latent Phase of Labor
Abnormalities of the Latent Phase of Labor