15 Using an integrated and inter-professional approach
Definition
The term ‘horizontal integration’ is used to describe the bringing together of subjects in the same phase of the curriculum. ‘Vertical integration’ is applied to the integration of subjects normally taught in different phases of the curriculum. Traditionally, the early years of the medical course were devoted to the study of the basic medical sciences. More recently we have seen, as described in Chapter 11, the introduction of clinical learning opportunities into the earlier years and the basic sciences related to this. More attention needs to be
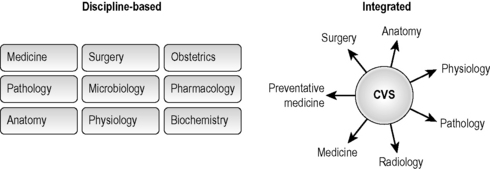
Fig 15.1 A comparison between how subjects are covered in a discipline-based and integrated curriculum.
paid to the integration of the basic sciences with clinical medicine in the later years of the curriculum.
Advantages of integration
• Integrated teaching reflects the practice of medicine. An integrated approach, more than a discipline-based approach, encourages the student to take a holistic view of the patient and his or her problems. In a final examination in a medical school that had a discipline-based curriculum we observed that a student, when asked to take a history from a woman with abdominal pain, enquired whether he should take a medical, surgical or gynaecological history. He had clearly failed to integrate what he had learned in the different clinical attachments.
• Integration motivates the students. Most students are not interested in becoming anatomists or physiologists and the relevance of the basic sciences to the practice of medicine may not be appreciated by them. The traditional curriculum, sadly, was often associated with a decrease in the early years in the students’ enthusiasm and interest in medicine.
• Integration by relating theory to practice makes learning more effective. The ability to retrieve an item from memory depends on the similarity between the condition in which it was learned and the context in which it is to be retrieved. In the classic diver experiment, divers learned from a text underwater and on the surface. When tested subsequently on the surface they performed better on the text learned on the surface. When tested underwater they performed better on the text they had learned underwater. This has been replicated in many other studies. It is also recognised that knowledge learned in isolation and not applied is easily forgotten – so called ‘inert’ knowledge.
• An integrated curriculum can help to avoid unnecessary re-duplication. An integrated curriculum highlights what is important for the student to know and can be seen as a response to the problem of information overload.
• The integrated curriculum may be more cost effective. Greater efficiency can be achieved by sharing teaching and learning resources such as the facilities in a clinical skills laboratory.
• An integrated approach promotes collaboration and communication between staff. An integrated approach requires a discussion between staff as to how each subject can contribute to the learning outcomes. Staff who collaborate in their teaching may go on to collaborate in their research activities.
Focus for integration
The focus for integration may be:
• The body systems. This is the most commonly adopted approach in the early years of the medical course with students studying, for example, a 6-week course on the cardiovascular system, a 5-week course on the respiratory system, etc.
• The life cycle. A focus for the integration may be the life cycle including the newborn, the child, the adolescent, the adult, the elderly and death. This may be used in conjunction with a system-based approach.
• Clinical presentations or a set of descriptions of the tasks facing a doctor. Task-based learning as described in Chapter 14 and in Appendix 3 is a useful approach to integration, particularly in the later years of the course (Harden et al 2000).
The integration continuum
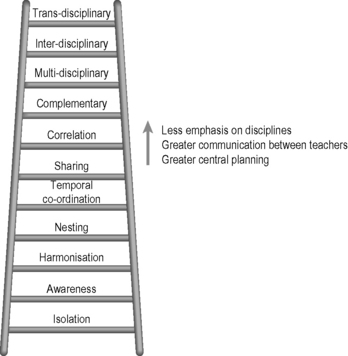
Discussions about integration have been polarised with some teachers arguing in favour and others against integrated teaching. In the SPICES model for educational strategies, integration is presented as a continuum with full integration at one end and discipline-based teaching at the other (Harden 2000). Any position between the two extremes may be adopted as described on the integration ladder (Fig. 15.2). The most appropriate level to suit a particular curriculum can be identified.
Inter-professional education
Continuum of inter-professional education
Inter-professional education can be described along a continuum of 11 stages, from isolation where healthcare professionals are taught separately from each other with no contact, to trans-professional education where learning is based in practice (Harden 1999). The steps are similar to the steps described on the integration ladder.
Principles of inter-professional learning
The Centre for the Advancement of Interprofessional Education (CAIPE) in the UK developed seven principles to guide provision, commissioning and development of inter-professional education (Freeth 2010). The vision is that inter-professional education:
1. works to improve the quality of care
2. focuses on the needs of service users and carers
3. involves service users and carers
4. encourages professions to learn with, from and about each other
5. respects the integrity and contribution of each profession
Implementation
Inter-professional education is generally well received, enabling knowledge and skills necessary for collaborative working to be learned (Hammick et al 2007). Methods used to implement inter-professional education in practice as described by Barr (2009) include:
• exchange-based learning: for example debates, case studies, shared lectures and e-learning
• action-based learning: for example problem-based learning (PBL) and task-based learning (TBL)
• observation-based learning: for example joint visits to a patient by students from different professions, shadowing another profession and work-related practice placements
• simulation-based learning: for example role-play, games, skills lab and a simulated ward
Reflect and react
1. Think about the approach to integration in your course. What is the focus for the integration and where are you on the integration ladder?
2. If you have an integrated curriculum, do the learning outcomes, the learning opportunities provided and the assessment all reflect an integrated approach?
3. In planning and implementing your training programme, has an inter-professional approach been considered? Have you discussed this with teachers in other professions?
Barr H. Interprofessional education. In Dent J.A., Harden R.M., editors: A Practical Guide for Medical Teachers, third ed., London: Elsevier, 2009. Chapter 24)
A useful account of interprofessional education..
Hammick M., Freeth D., Koppel I., Reeves S., Barr H. The best evidence systematic review of interprofessional education. BEME Guide No. 9. Med. Teach.. 2007;29:735-751.
Hammick M., Olckers L., Campion-Smith C. Learning in Interprofessional Teams. MEE Guide No. 38. Dundee: AMEE, 2009.
An overview of the place of inter-professional education in the healthcare professions..
Harden R.M. Multiprofessional Education. AMEE Medical Education Guide 12. Dundee: AMEE, 1999.
A description of approaches to multi-professional education..
Harden R.M. The integration ladder: a tool for curriculum planning and evaluation. Med. Educ.. 2000;34:551-557.
A description of the 11 steps in the integration ladder..
Harden R.M., Crosby J., Davis M.H., et al. Task-based learning: the answer to integration and problem-based learning in the clinical years. Med. Educ.. 2000;34:391-397.
A description of how TBL provides a focus for integration in the clinical years..
Bandaranayake R. The Integrated Medical Curriculum. London: Radcliffe Publishing; 2011.
A definitive and practical account of integration in the medical curriculum..
Fogarty R. How to Integrate the Curricula. Illinois: IRI/Skylight Training and Publishing; 1991.
A view of the integrated curriculum from the perspective of schools..
Freeth D. Interprofessional education. In: Swanwick T., editor. Understanding Medical Education: Evidence, Theory and Practice. Chichester: Wiley-Blackwell, 2010. (Chapter 4).
Miller B.M., Moore D.E.Jr., Stead W.W., et al. Beyond Flexner: a new model for continuous learning in the health professions. Acad. Med.. 2010;85:266-272.
This article describes a model that promotes inter-professional education..