CHAPTER 6 Use of Compression Therapy
Historical Development
The oldest known illustration of compression bandages dates back to the Neolithic Age (5000–2500 BC) (Fig. 6.1).1 The ancient Hebrews, Egyptians, Greeks, and Romans used compression therapy for treatment of wounds and ulcers, as described in the Smith Papyrus (1650–1552 BC) and in the Book of Isaiah (Isaiah 1:6), eighth century BC.2 Hippocrates wrote about compression treatment in the fourth century BC, and this was followed by further refinements from Celsus and Virgo. Roman soldiers who marched for days at a time learned quickly that applying tight strappings to the legs reduced leg fatigue. The knowledge concerning the beneficial effects of compression was rediscovered by physicians during the Middle Ages, including Guy de Chauliac (1363), Giovanni Michele Savonarola (1440), and Fabrizio d’Aquapendente (1537–1619). They used compression bandages, plaster dressings, and laced stockings made from dog leather.3

Figure 6.1 Mural paintings in the Tassili caves (Sahara), 5000–2500 BC.
(From Partsch H, Rabe E, Stemmer R, Compression therapy of the extremities, Paris, 1999, Editions Phlébologiques Francaises.)
Ambroise Paré (1510–1590), Richard Wiseman (1622–1676), Christian Anton Theden (1714–1787), and Thomas Baynton (1797) were pioneers, especially in the treatment of leg ulcers, recommending different kinds of compression material that were mainly inelastic. In 1885, the dermatologist Paul Unna introduced his zinc paste boot for the treatment of venous dermatitis, and in 1910, his pupil, Heinrich Fischer, recommended firmly applied ‘Unna boots’ for treating venous thrombosis.3,4
The use of elastic compression occurred with the development of elastic stockings in the mid 1800s and the discovery by Charles Goodyear in 1839 of a vulcanizing process for rubber that would increase its elasticity and durability. In 1839, John Watson, MD, reported on the usefulness of an elastic stocking in treating varicose veins in a 23-year-old woman with Klippel–Trenaunay syndrome.5 However, these stockings, made exclusively from rubber threads, were uncomfortable. It was not until Jonathan Sparks patented a method for winding cotton and silk around the rubber threads that elastic stockings became comfortable and popular.3
Mechanism of Action
Edema
By increasing the tissue pressure, compression works against filtration, which is the basis of both prevention and removal of edema. Occupational leg swelling in sitting and standing professions can be prevented by light compression stockings,6 which are also able to reduce mild edema.7,8 Reduction in intradermal edema has been measured with 20-MHz ultrasound in patients with chronic venous insufficiency (CVI) and lipodermatosclerosis.9 Application of class I or II graduated compression stockings decreased dermal edema by 17% in 4 days, with no statistical difference between the two classes of compression. However, severe stages of limb swelling benefit more from compression devices exerting higher pressure.
Compression may also exert beneficial effects in nonphlebologic causes of edema, such as inflammatory edema (arthritis, cellulitis), cardiac edema, dysproteinemic edema, renal edema, lymphedema, and cyclic idiopathic edema.10A study by Arpaia et al11 showed an improvement in the quality of life (QOL) in patients with chronic CVI who wore class I graduated compression stockings.
Lymph drainage
Several beneficial mechanisms of compression therapy on the swollen extremity may be explained by its effects on the lymphatic system:12
One mechanism of central importance is the restriction of capillary filtration, which corresponds to the amount of the lymphatic load. With compression, the skin and dermal tissues are in closer contact with the superficial capillary network, which is otherwise separated by a pericapillary halo of protein-rich edema fluid.14
Compression removes more water than protein from the tissue, thereby increasing oncotic tissue pressure and reinforcing the need for sustained compression. Therefore, in chronic edema, success is dependent on continued compression.15
Compression together with movement enhances the contraction of the lymphatic system. Olszewski was able to demonstrate that both compression and exercise stimulated the movement of stagnating lymph through the lymph collector in lymphedema patients, in which the lymphatic trunks were filled.16,17 This is probably one explanation for the reduction in intralymphatic hypertension obtained by complex decongestive therapy, as demonstrated by Franzeck and co-workers by lymph capillary pressure measurements.18
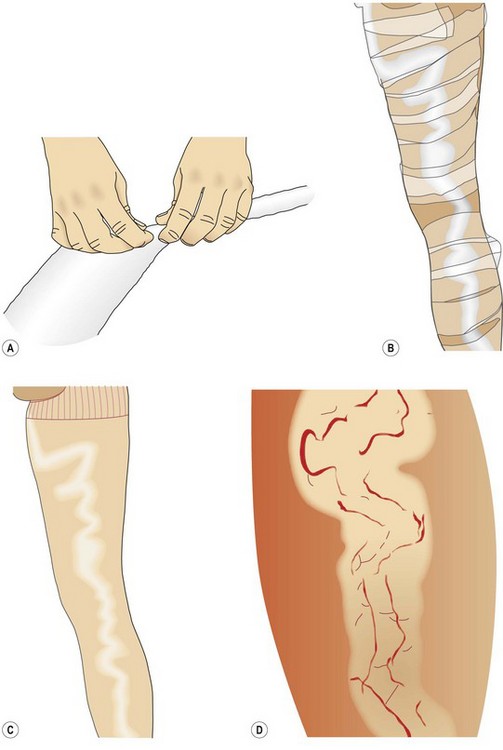
Intermittent pneumatic compression enhances prefascial lymph drainage.15 Unna boots are able to increase subfascial lymph transport, which is reduced in post-thrombotic syndrome.19 Consequent compression leads to a morphologic improvement of pathologic initial lymphatics in patients with lipodermatosclerosis, which can be demonstrated by indirect X-ray lymphography (Fig. 6.2).20
Venous system
Depending on the exerted pressure and the body position, external compression is able to narrow or occlude superficial and deep leg veins.21 In the supine position, an external pressure of 10 to 15 mmHg is enough to decrease the venous diameter. This results in an increase in blood flow velocity, as shown by measuring the circulation time with isotopes,22 and is the rationale for recommending light compression stockings for thromboprophylaxis in bedridden patients. A graduation in pressure (18 mmHg at the ankle, falling to 8 mmHg at the thigh) leads to a significantly increased velocity in the deep femoral vein flow.23
In the upright position, such low pressure will have only a minimal effect on decreasing the diameter of the leg veins.24 However, a very small decrease of venous diameter will result in an over-proportional decrease of the local blood volume, as demonstrated by several plethysmographic studies.25–32 Stockings with an ankle pressure of around 20 mmHg have been shown to improve the venous pump.25,30,31 Elastic compression stockings with as little as 8 mmHg pressure have also been found to significantly reduce symptoms of CVI in patients during daily work activity.33–35
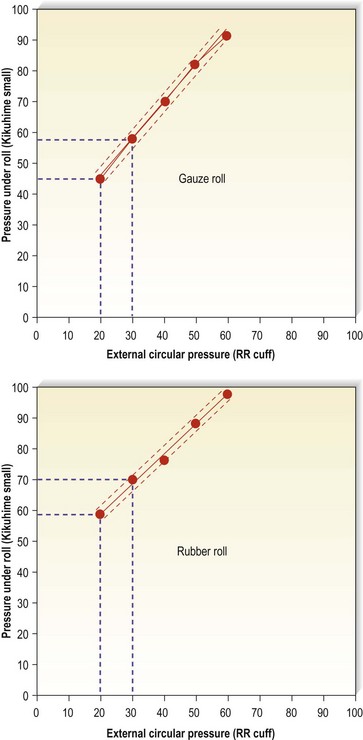
Bandages may provide much higher pressure in the upright position. Magnetic resonance imaging (MRI) is able to show that, during standing, deep veins will be narrowed by an external pressure of 42 mmHg and nearly occluded by a pressure of 82 mmHg (Fig. 6.3). During ankle movements and walking with stiff bandages, pressure peaks of this magnitude will therefore lead to an intermittent occlusion of the veins (Fig. 6.4). Such high pressure may be tolerated only with inelastic (not with elastic) material.
The compression pressure when starting walking counteracts the lateral expansion and dilation of leg veins during muscle contraction by encasing the veins in a semirigid envelope.36,37
The application of an external pressure with a blood pressure cuff blown up to 40 to 60 mmHg to various portions of the leg containing incompetent valves led to an abolishment of reflux.38,39 This effect was directly associated with a decreased vein diameter. Reduction of venous refluxes and improvement of ambulatory venous hypertension by external compression could be demonstrated even in patients without any valves (avalvulia), indicating that this effect is not necessarily explained by coaptation of distended valve leaflets but rather seems to be due to increasing the resistance to retrograde flow.40 Increasing external pressure in the upright position increases the ejection fraction of the calf muscle pump function.41
Conflicting results have been reported concerning an improvement in ambulatory venous hypertension by using compression stockings.36,42 One study showed a significant decrease of such hypertension with short-stretch bandages applied with a resting pressure on the distal leg of more than 50 mmHg, but not with elastic compression stockings exerting a pressure of 30 to 40 mmHg.37 This may be explained by the fact that inelastic, short-stretch bandages lead to an intermittent short venous occlusion during the muscle systole while walking. In patients with venous ulcers due to deep venous incompetence, short-stretch bandages are able to impede venous refluxes more effectively than are elastic stockings exerting the same resting pressure.43 Patients with severe stages of CVI benefit more from high compression pressure, whereas lower pressure is sufficient for milder stages such as varicose veins.44
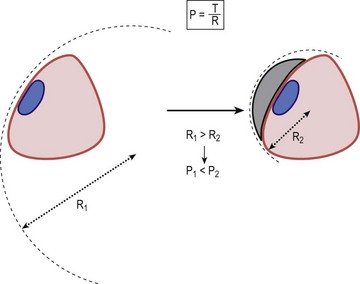
To achieve complete occlusion of superficial veins, the external pressure should be higher than the intravenous pressure, and this depends on the body position. It was shown that occlusion of the leg veins can be obtained with an external pressure in the range of 20 mmHg in the supine position, but that in the sitting and standing positions the pressure has to be between 50 and 70 mmHg.21 With compression stockings, such pressure ranges can only be achieved when rolls or pads are applied over the vein, thereby increasing the local pressure by reducing the local radius (law of Laplace, see later). Such rolls may be especially useful if local compression over treated veins on the thigh is intended.45
Microcirculation
Compression accelerates blood flow in the enlarged capillary loops and reduces capillary filtration due to enhanced tissue pressure. Improvements are seen in normalization of venular flow, volume, and velocity, improved distribution of microcirculation blood flow, and normalization of leukocyte adhesion.46–52 Different studies using electron microscopy were able to show a restoration of the structural changes in the media myocytes in stripped veins53 and a tightening of intercellular junctions.54 Laser Doppler flux measured a 29% increase in blood cell velocity in patients with CVI and lipodermatosclerosis.49 Increasing flow velocity may reduce the likelihood of white blood cells interacting or sticking to endothelium with release of various factors. Effects on mediators involved in the local inflammatory response may explain both the immediate pain relief that occurs with good compression and ulcer healing.55
Studies in patients wearing class II graduated compression stockings demonstrate an improvement in skin microcirculation in as little as 1 week, with near normalization of the functional state of microcirculation becoming apparent by day 30.52 Model experiments with intermittent pneumatic compression were able to demonstrate that there is an increased release of the endothelial relaxing factor (EDRF) nitrogen oxide from the endothelial cells, depending on the amount of shear stress produced by the compression waves.56
Compression tightens the junctions between the endothelial cells of capillaries57 and reduces pro-inflammatory cytokines in venous leg ulcers.58
Arterial flow
A reduction of arterial flow may be expected when the external compression pressure exceeds the intra-arterial pressure. This may happen in patients with arterial occlusive disease with a reduced peripheral arterial pressure. In order to avoid ischemic skin lesions from external compression, therefore, it is essential to measure the peripheral arterial pressure using a Doppler probe before strong compression bandages or stockings are applied. It is generally accepted that a Doppler ankle–brachial index (ABI) of less than 0.5 is a contraindication for sustained compression. However, external compression does not invariably mean reduction of arterial flow.59 Mayrovitz reported on several experiments concerning arterial blood flow and compression60–62 and was able to demonstrate an increase of the pulsatile flow below the knee in healthy volunteers using nuclear magnetic resonance flowmetry.60 He also demonstrated a reduction in toe blood perfusion, which was greater with increased compression, but not of sub-bandage skin perfusion.
Patients with edematous legs and with an ABI of between 0.5 and 0.8 may benefit from inelastic or short-stretch bandages applied with a mild resting pressure, due to the edema-removing massage effect that will occur with every ankle movement (see later). Completely inelastic bandages, together with walking, have a similar effect as intermittent pneumatic compression. The rhythmic pressure peaks of an inelastic bandage during walking can be compared with those exerted by an intermittent pneumatic pressure pump. Several experiments with intermittent pneumatic compression have demonstrated an increase of arterial flow in patients with arterial occlusive disease.63–68 The decisive mechanisms of action are the reduction of edema, an increase of the arteriovenous pressure gradient, myogenic mechanisms, and the release of vasoactive substances from the endothelial cells.
Basic Principles of Compression
Terminology
A confusing variety of partly overlapping terms can be found in the literature:1,69–79 Only terms of practical importance are listed here:
Compression pressure and Laplace’s law
The compression pressure (Pascal) is defined by the force (Newton), which is exerted to an area of 1 m2 (Fig. 6.6). The tension in a bandage is determined by the force applied to the fabric during application.
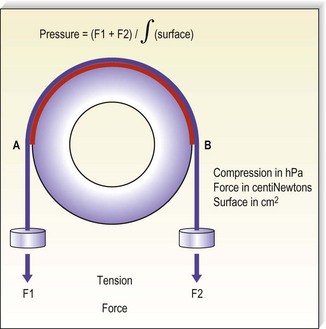
Figure 6.6 The pressure generated by an inelastic bandage is determined by the tension of the fabric.
(Courtesy Bernard Lun, Ganzoni, St Just, France.)
From Figure 6.6 it is clear that the curvature of the leg plays a deciding role for the exerted pressure. If the cylinder in the model was replaced by a cube, the pressure over the flat areas would be zero, while it would be very high along the sharp edges of the cube. This is described by Laplace’s law stating that the pressure (P) is directly proportional to the tension (T) of the bandage but inversely proportional to the radius (R) of the curvature to which it is applied (Fig. 6.7):
Practical consequences of Laplace’s law
In general, pressure is calculated for the circumference of the limb at a specific level. Because the leg has an irregular cross-section that is not circular, the applied point pressures vary at different locations around the leg. Using Laplace’s formula, it is evident that the effective pressure is greatest at the point of minimum radius and least at the point of maximum radius. Thus, when a stocking is applied, the anterior aspect of the leg receives the greatest amount of pressure, and the lateral and medial sides of the leg receive the least compression pressure. This is especially important in the malleolar area, where the lowest degree of compression occurs, because the medial and lateral surfaces are flat or hollow, the local radius being ‘negative’ (Fig. 6.8). If there is a venous ulcer situated in the dip behind the malleolus, the only way to bring compression to this region is to put a pad over that area (Fig. 6.9). The reduction of the local radius by pads or rolls in order to increase local pressure has been termed ‘positive eccentric compression’.1
On the other hand, tendons and bony prominences are susceptible to a high compression pressure and should therefore be protected under a bandage by decreasing the radius using a cotton wool inlay. The enlargement of the local radius has been termed ‘negative eccentric compression’.1
Measurement of compression pressure
Laboratory measurements of compression stockings
The effects of compression depend widely on the exerted pressure, which should be adapted to the underlying condition. Basically, the pressure of a stocking is calculated from the force–extension diagram of the elastic fabric on a wooden leg model with defined circular cross-sections using Laplace’s formula (Fig. 6.10). The range of the compression pressure indicated by the manufacturers is determined by the measurement of the force which is necessary to stretch the stocking at certain leg levels (B, B1, C, D, F, G) in a transverse direction. The proportion of stretch and force for each circumference level, which corresponds to the steepness of the so-called slope in the hysteresis curve, reflects the elasticity of the material of the stocking.
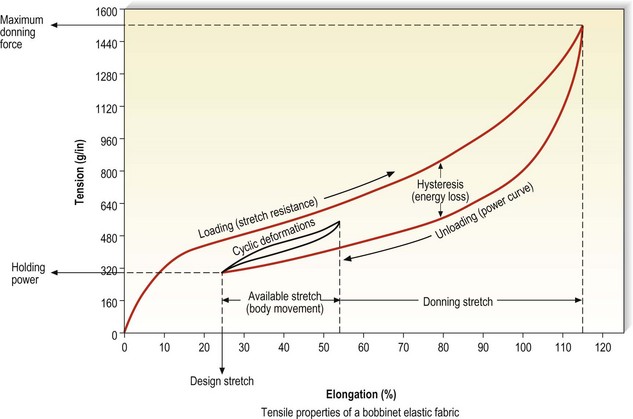
Figure 6.10 Hysteresis curve generated by a bobbinet elastic fabric.
(Courtesy of Beiersdorf-Jobst, Charlotte, N.C.)
Measuring points, lengths, and girths defined by the European standardization proposal (CEN, Centre Européen de Normalisation)69 are shown in Figure 6.11.
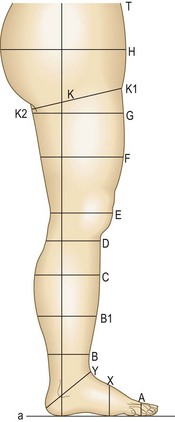
Figure 6.11 Measuring points, lengths, and girths on the human leg. Note: measurements should be taken of the patient’s leg in a standing position.69
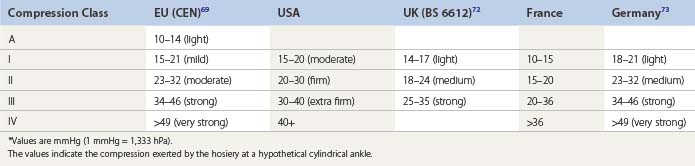
Table 6.1 gives a comparison of compression classes for ready-to-wear and custom stockings used in several countries. The range of compression pressures, and also the verbal description of these classes, are amazingly variable from one country to another. Additionally, it is important to realize that the given ranges are measured by different methods, so comparisons are problematic. These facts underline the necessity of in vivo pressure measurements on the individual leg, at least in future clinical studies. For a better universal understanding, it is recommended to use the pressure range in mmHg rather than compression classes in general.
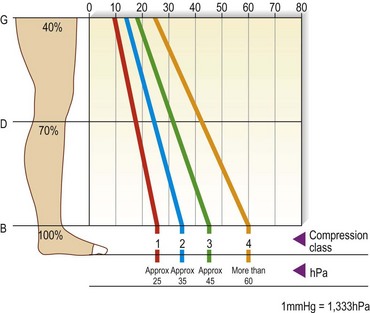
The pressure values in Table 6.1 refer to level B. The European prestandard69 defines the ranges of pressure profiles in comparison with the pressure at the smallest leg circumference (position B) as follows: for level B1 70% to 100%, for C and D 50% to 80%, and for F and G 20% to 40% for compression classes III and IV; 20% to 60% for compression classes A and I, and 20% to 50% for compression class II (Fig. 6.12). The producers of compression stockings recommend adjusting the compression class according to the clinical severity.
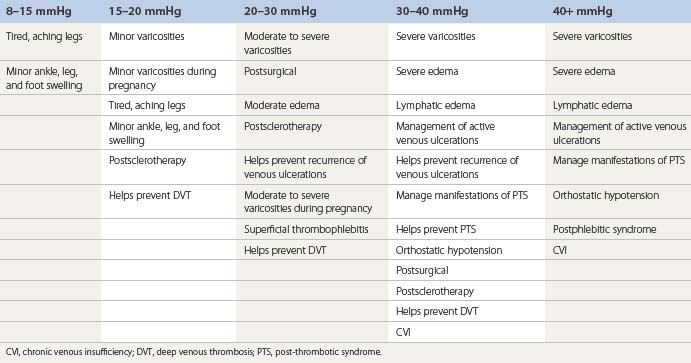
There is no American standard. Table 6.2 gives an example as recommended by one company (BSN-Jobst, Charlotte, N.C.).
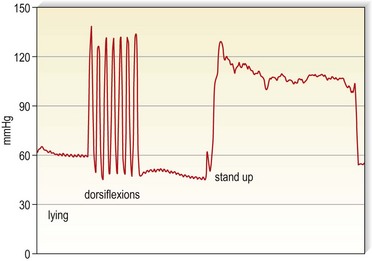
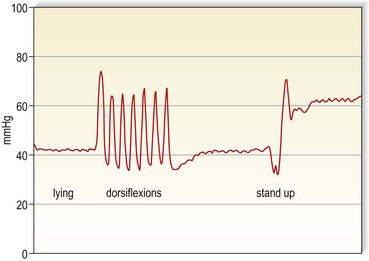
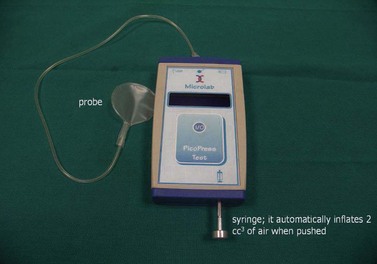
Measurements of interface pressure on the leg
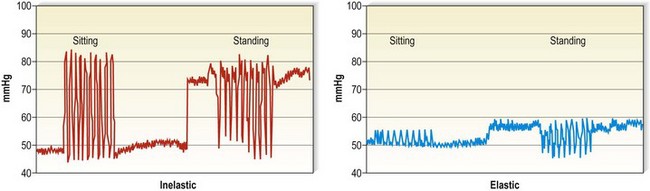
Several instruments are available, which should be calibrated on the leg according to a recent consensus recommendation.81 In this consensus paper, some prerequisites of an ‘ideal’ pressure sensor are summarized. One location that should always be included in future pressure measurements is B1. This is where the tendinous part of the gastrocnemius muscle changes into the muscular part, showing the most pronounced protrusion of the tendon and the most extensive enlargement of the leg circumference during dorsiflexion or by standing up from the supine position. Whenever in vivo measurements of interface pressure are performed, it is essential to indicate the exact measuring point, the main specifications of the instrument, including the dimensions of the probe, and the body position in which the measurements have been performed. Figure 6.13 shows a pressure measuring instrument which allows continuous pressure registration. The flat probe is inflated only when pressure is measured and can stay on the leg for several days. Figures 6.4 and 6.5 show pressure curves obtained with this instrument.
Resting and working pressure
Some probes allow measurements of interface pressure not only at rest but also continuously during movement. Figure 6.14 shows an example where the interface pressure on the distal leg was measured continuously in different body positions, both for an inelastic and for an elastic bandage. Starting with comparable resting pressure for both bandages, the inelastic bandage has a higher working pressure than the elastic bandage. This difference has a major impact on the efficacy of the compression device concerning edema reduction and improvement of venous pump. Stockings with high stiffness or slope value, even at the same compression level, are better for patients with edema from CVI or other causes.82 Inelastic bandages are more effective to reduce venous refluxes and ambulatory venous hypertension.37,43
Measurements of intramuscular pressure have shown higher resting pressure with elastic than with inelastic material, suggesting that elastic compression applied over a long period in the recumbent posture may impede microcirculation and jeopardize tissue viability.83
Measurement of stiffness
Stiffness is defined as the increase in compression per centimeter increase in the circumference of the leg, expressed in millimeters of mercury per centimeter.69 This parameter characterizes the distensibility of a textile as well as the elastic property of a composite bandage, which plays an important role concerning the performance of a compression device during standing and walking. Stiffness may be measured in the laboratory, where it corresponds to the slope of the hysteresis curve. The fact that it can also be assessed by in vivo measurements on the individual leg will certainly achieve increasing practical importance in future trials.80,81,84
Measurement of dynamic stiffness during walking requires sophisticated instrumentation and can therefore not be used in routine clinical practice.80 In order to obtain valuable information on the elastic property of a compression device, which may be quite complex when several materials are combined, the so-called ‘static stiffness index (SSI)’ may be a useful alternative.79 A calibrated pressure sensor is fixed to the medial aspect of the leg at B1. This is the area which will show the most extensive changes in local curvature and leg circumference when the body position is changed between supine and standing. The difference between the interface pressure in the standing and in the lying position, called SSI, is a valuable parameter for the stiffness of the compression system, which determines the relationship between resting and working pressure. As is shown in Figure 6.15, inelastic material produces a much higher pressure increase in the upright position than elastic material. It is important to note that different indices may be obtained with different sensors. Therefore, reliable comparisons of different compression devices will only be possible by testing using the same sensor on the same site.
It has been shown that different padding materials may change the stiffness of the final bandage.84
Compression Material
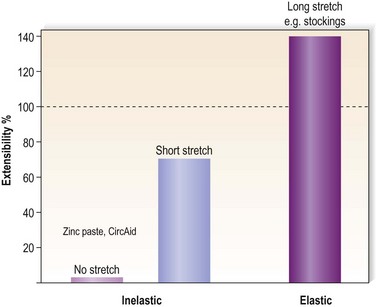
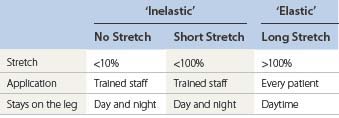
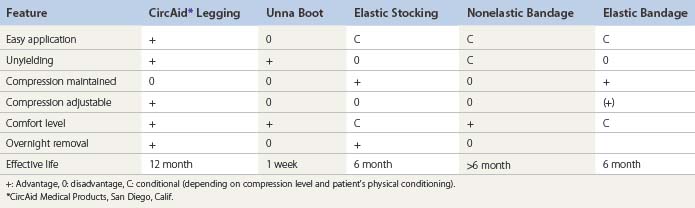
Different devices/materials are available for compression therapy (Box 6.1). The main categories of compression concerning the elastic properties of the materials are summarized in Table 6.3. Extensibility is the ability of a bandage to increase in length in response to an applied force.
Compression bandages
There are three basic types of bandages: completely nonelastic bandages, virtually without any stretch, e.g. Unna’s boot or Velcro-band products; short-stretch bandages (<100% extensibility); and long stretch (>100% extensibility) (see Table 6.3).
No-stretch and short-stretch material is frequently called ‘inelastic’ and long-stretch material ‘elastic’ (Figure 6.14).
Standards for compression bandages
There is currently only the British standard, (BS) 7505:1995, for compression bandages. It contains four categories of compression bandages,72 which are summarized in Table 6.4.
Table 6.4 Classification of compression bandages by British Standard72
| Bandage Type BS 7505 | Level of Compression | Pressure British Standard (mmHg) |
|---|---|---|
| 3A | Light | Up to 20 |
| 3B | Moderate | 21–30 |
| 3C | High | 31–40 |
| 3D | Extra high | 41–60 |
By definition, the indicated pressure levels should be achieved on an ankle 23 cm in circumference, when applied with a 50% overlap. This classification was constructed entirely based on in vitro measurements and does not correspond to the clinical reality, according to which the resulting pressure of a bandage mainly depends on the sretch during application and far less on the material. Only a few measurements of compression pressure on the human leg have been reported, applying different materials with light, moderate, and high strength.85 It could be demonstrated that the interface pressure of a bandage on the human leg was, on average, one class higher compared with the values in Table 6.1 for compression stockings. Even with intentionally very loose bandaging in an attempt to achieve ‘light compression’, the pressure of the 5-m-long bandage, short stretch and long stretch, was always higher than 20 mmHg with one bandage and higher than 30 mmHg with a multilayer technique.
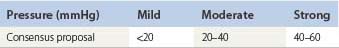
Because of these dicrepancies, new proposals concerning a bandage classification were made in a consensus conference based on practical measurements in vivo.70 The eponym ‘PLACE’ was proposed, containing the main characteristics to be considered when compression bandages are applied: P stands for pressure, LA for layers, C for components and E for the elastic property of the single bandage used. Table 6.5 shows the definition of different pressure ranges. Bandages are always applied with some overlap so that one layer bandages do not exist. The only one layer system is a compression stocking. Actually, the so-called four-layer bandage is applied with much more than four layers and should correctly be called a ‘four-component bandage’ since it contains four different bandage materials. It was proposed to use the terms ‘elastic’ and ‘inelastic’ only for single bandages based on their elastic properties, but not for a final bandage consisting of different single bandages. In fact, the elastic property of the final bandage cannot be predicted based on the elasticity of the single components. Adding several bandages does not only increase the sub-bandage pressure but enhances the stiffness of the final bandage as well.
Inelastic and short-stretch bandages
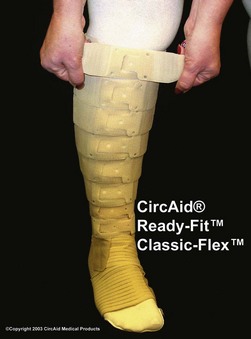
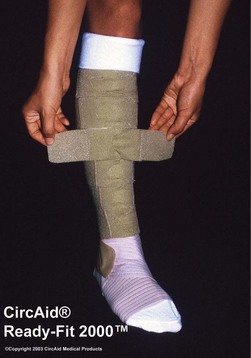
Bandages with an extensibility close to zero, such as zinc paste (Unna boot) and rigid Velcro-bands like Circ-Aid (CircAid Medical Products, San Diego, Calif.) or Hydroboot, (Incappe Inc, Brandon, Miss.) are examples of completely nonelastic material. Nonelastic bandages must be applied with skill and some knowledge. If light compression is indicated they should be applied without extension of the fabric by moulding the material to the leg without tension. When strong compression is indicated, completely rigid zinc paste bandages need to be applied with full extension of the material and adjusted to the configuration of the leg. Figure 6.16 shows a bandage applied with zinc paste on the lower leg, wrapped over with a short-stretch bandage and with adhesive bandages over the knee and thigh of a patient with a proximal deep vein thrombosis (DVT).
Short-stretch bandages can be extended 30% to 100% and should be applied with a pressure of more than 50 mmHg on the distal leg if strong compression pressure is indicated. Due to an immediate removal of edema, this pressure will fall down to pressure values which are also well tolerated in the supine position. After some hours they have a low to slight resting pressure but still a high and very effective working pressure. Short-stretch bandages exert little pressure when the calf muscles are relaxed but prevent expansion in calf diameter when the muscles are contracting during standing and walking (‘high working pressure’). They are, therefore, comfortable when patients are recumbent, and they act to decrease venous pressure with ambulation.37 The main disadvantage is that they may become loose after a few hours of wear, especially when applied too loosely. In immobile patients, correctly applied short-stretch and inelastic bandages are even more effective than long-stretch material. Even minimal toe movement or passive ankle mobilization performed by physiotherapists will produce a much higher massaging effect compared to elastic material.
Stiff bandage material is not easy to handle. Most untrained persons apply inelastic bandages with too low a pressure. In order to obtain a resting pressure on the distal leg of about 40 mmHg, the initial pressure after application should reach about 60 mmHg. As can be seen from the example in Figure 6.17, the resting pressure in the supine position drops from 70 mmHg to 50 mmHg after 2 hours. This pressure exerted by an inelastic bandage is also well tolerated during night time. However, there is less pressure loss in the standing position, so an effective range of pressure values is still maintained after 24 hours (see Fig. 6.17). Especially in the first days after bandage application, the reduction of swelling may be so pronounced that the bandages will get loose and have to be renewed. When edema reduction is stabilized, inelastic bandages may stay on the leg for several days.
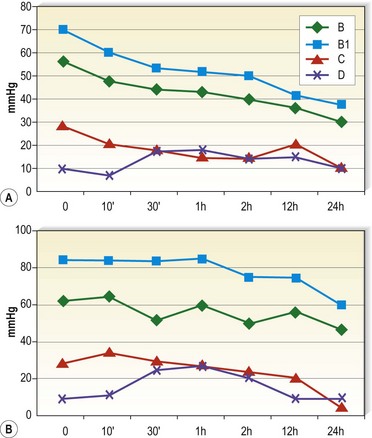
Figure 6.17 Interface pressure exerted by a multilayer short-stretch bandage (Rosidal sys, Lohmann) measured by an MST tester119 on the medial leg in the supine (A) and in the standing position (B). Measuring points: B = behind the inner ankle, B1 = 8 cm above, C = 19 cm above, D = 27 cm above the ankle. The pressure drop of this multilayer short-stretch bandage is more pronounced in the supine than in the standing position.
A study of elastic, minimal-stretch, and nonelastic orthoses (CircAid), demonstrated that 4 hours after application, elastic bandages had 94% of their initial pressure, compared with 70% for minimal-stretch and 63% for the nonelastic orthoses.86 In the supine position, the decrease at 4 hours was 72% for elastic, 59% for minimal-stretch, and 44% for nonelastic compression. One of the advantages of this particular orthosis is the fact that it can be readapted by the patient when it gets loose (Figs 6.18 and 6.19). Smaller but significant decreases in pressure under short-stretch bandages were also found in studies on changes in pressure with exercising.87,88 Measurement of compression after walking for 3 hours and then again 7 days later showed a decrease in pressure from 80.5 mmHg to 43.6 mmHg after 3 hours and to 26.3 mmHg after 7 days. In this study, Comprilan (Beiersdorf, Germany) with an extensibility of 70% was used.87 In the second study, elastic bandages did not demonstrate a similar degree of compression loss after tip-toe exercise.88 Although the authors speculate that the loss in pressure during exercise may be related to application technique of the short-stretch bandage with a maximum tension of 45% (Compridur, Beiersdorf, Germany), this could also be explained by an immediate volume reduction of the leg as shown in healthy volunteers and in lymphedema patients (Rosidal sys and Rosidal Lymphset, Lohmann & Rauscher, Germany).89
When the bandage gets loose, it should be renewed in order to prevent refilling of the extremity with edema and to avoid tourniquet effects from the down-gliding compression material. In patients with lymphedema who are best treated with short-stretch bandages in the initial phase, this may be necessary once a day.90
Elastic, long-stretch bandages
Long-stretch bandages can be extended 140% to 200% and thus have a high resting pressure; that is, they exert pressure on the superficial venous system when the limb is at rest with a decreased working pressure as compared with short-stretch bandages (see Fig. 6.15). Because of their intrinsic high resting pressure, they can damage arterial, lymphatic, and venous flow if not applied carefully, so they are best used while patients are ambulatory. Their advantage is that they may be more easily molded around the heel and ankle and can sustain their pressure better than inelastic bandages.
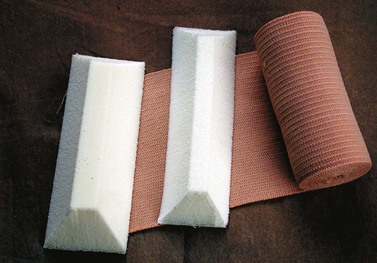
Multilayer bandages
In the above-mentioned consensus paper it is stated that ‘multilayer bandages’ are actually multicomponent bandages consisting of different materials for padding retention and compression.70
From these definitions it is quite obvious that many combinations of different materials are possible, which will lead not only to an increasing pressure with each layer but also to variable elastic properties of the final bandage. In a comparative trial with different brands of four-layer bandages it was found that, in fact, a bandage applied as part of a multilayered system achieves only about 70% of the pressure that it exerts when applied alone, thus challenging the commonly held assumption that the final pressure achieved by a multilayer bandaging system is the sum of the pressures exerted by each individual layer.91 The elastic property of the final bandage will change toward a more inelastic bandage due to the friction of several layers, so that it can also be tolerated in the supine position92 (Fig. 6.20). One example is the so-called four-layer bandage which consists of several components of different material (wool, crepe, elastic and self-cohesive) and which may be worn day and night (Profore, Smith & Nephew, Hull, UK).
It had been claimed that such bandages have not lost pressure at 1-week follow-up.93 Actually some of our own measurements revealed a pressure loss starting immediately after application which is less pronounced compared to short-stretch bandage systems.
One study compared eight different compression bandages under standardized conditions.92 Multilayer bandage systems composed of short and medium stretch bandages exhibit the smallest pressure loss with patient activity and have a significant pressure decrease when the patient is supine. These systems gave better postural and interface pressure changes than all types of single-layer bandages, obviously due to an increase of the stiffness of the final multilayer bandage.79,85
There are also multilayer systems consisting of short-stretch material, which are equally effective in ulcer healing when applied correctly.94,95 Examples are the Pütter bandage (Hartmann, Germany), Rosidal sys (Lohmann & Rauscher, Germany), the adhesive Actico bandage (Activa Healthcare, UK), the Coban 2 bandage (3M, Minnesota, USA) and the Fischer bandage, consisting of a tightly applied Unna boot with a short-stretch bandage on top. This latter bandage was recommended by Heinrich Fischer, the pupil of Unna, in 1910 for the treatment of DVT4 and is still one of the author’s favorites in patients with DVT, post-thrombotic syndrome, or venous leg ulcers (see Fig. 6.16). The tradition of using multilayer short-stretch bandages is rather restricted to central European countries and to the Netherlands, while many bandagers in the UK are more familiar with multilayer systems containing rather long-stretch material.
Several trials have compared multilayer long-stretch bandages with short stretch, some showing better results with the short stretch,94,95 some with long-stretch multilayer systems.96,97 Frequently unfair comparisons have been made comparing properly applied versus inadequately applied bandages. In future trials, sufficient training of the bandagers should be provided for both systems and interface pressure and stiffness should be measured.
The principle of applying several compression layers over each other is also a promising concept for elastic stockings, with regards to an increase in both compression pressure and stiffness.98,99
Training in the application of bandages
A major drawback of bandages is their non-uniform application. A comparison of the range in pressures measured during application of a long-stretch elastic bandage by skilled nurses versus nursing students demonstrated that the skilled bandager’s pressure ranged from 25 to 50 mmHg, and the unskilled bandager’s pressure ranged from 15 to 70 mmHg.100
A recent study checking the sub-bandage pressure showed that especially nurses with long professional experience tend to apply short-stretch bandages much too loosely (< 20 mmHg) and that this can be greatly improved by training.101
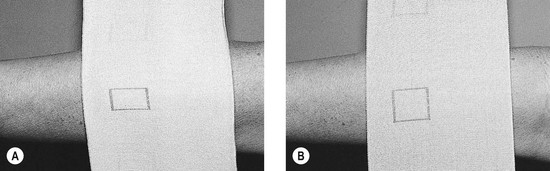
Several elastic bandages are marked with geometrical figures, such as a rectangle that becomes a square when stretched to the proper length (e.g. Setopress, Seton Healthcare Group, Oldham, UK; Proguide, Smith and Nephew, UK; Velpeau, Lohmann & Rauscher, France) (Fig. 6.21). Setopress was studied in five skilled nurses and five unskilled assistants, who also applied an Elastocrepe (Smith and Nephew, UK) bandage to the opposite leg. The Setopress bandage applied by experienced nurses most closely approximated target sub-bandage pressures whereas the unskilled group differed significantly among themselves. As before, both groups differed significantly in applying sub-bandage pressure with the Elastocrepe bandage, with a significant difference noted between the skilled nurses and unskilled bandagers.102 An additional study of 18 nurses applying an adhesive compression bandage showed 10 nurses producing a tourniquet effect, 5 producing inadequate ankle pressure, 2 excessive ankle pressure, and 1 appropriate ankle pressure but with an improper gradient in the calf.103 Training significantly improved performance. Another study of 48 trained community nurses that compared one inelastic and two elastic bandages showed similar results.104 The most common problem was production of a calf tourniquet.
In addition, even with physicians who are experts in applying bandages, a true graduation in pressure may not always be obtained. One study of five surgeons showed a range of 21.9 to 52.7 mmHg with application of a short-stretch bandage, with each individual surgeon having a range of 10 to 20 mmHg between bandage applications.105 The coefficient of variation in each individual ranged from 9.9% to 25.2% with a mean (standard deviation) of 17.0 (4.9%).
Based on the information just presented, it is obvious that training in the application of bandages is very important.101–107 This is especially true for inelastic bandages, which should be applied with a higher initial pressure compared to elastic material. Instruction of compression application with the use of interface pressure measurement has been shown to improve technique.107 In teaching 156 persons at a wound healing course, the application of appropriate interface pressures required approximately 10 exercises with the use of interface pressure transducers.
Important points to consider when applying a bandage are:
Compression bandages or compression stockings?
In general, compression bandages are able to achieve higher pressure than compression stockings.85 Therefore, in severe stages of venous disease, treatment may be initiated with compression bandages.
Multilayer bandages consisting of several layers of long-stretch material obtain the elastic property of short-stretch bandages (see Fig. 6.20) and may also stay on the leg for several days.
Table 6.6 gives an overview of some practical characteristics of different products.
Compression stockings
Graduated compression stockings are useful both for acute therapy after surgery or sclerotherapy treatment of varicose or telangiectatic leg veins and for long-term therapy in patients with CVI.75,108 In the supine position, blood is pressed from the superficial to the deep veins. This effect may be used to improve the opacification of the deep veins when performing computed tomography (CT) venography.109 During standing, they achieve only a rather modest reduction on the venous diameters in the leg.21,110,111 However, they provide an external support to prevent swelling. By virtue of their ‘graduation’ (see Fig. 6.12), compression stockings help to propel blood toward the heart during walking.36–44,112,113 Unlike nonelastic bandages, they do not lose compression with time (except after months of continuous use).
Although they usually do not have adverse effects when properly fitted, some types of elastic stockings may rarely cause an allergic reaction. This has been reported with elastic stockings composed of 76% nylon and 24% Elastane (Scholl Soft Grip, Scholl UK) in less than 1% (2 of 126) of patients.114 More commonly, the silicone beads used to help hold the stocking up on the thigh cause an allergic reaction (Fig. 6.23).
Ready-made stockings
Ready-made or off-the-shelf stockings are manufactured in fixed sizes. Most manufacturers have several sizes, varying in both length and width at various points on the ankle, calf, and thigh (Fig. 6.24). Although the sizes are standardized to some degree by associations of stocking manufacturers, such as the Gütezeichengemeinschaft Medizinischer Kompressionsstrümpfe e.V. (Quality Seal Association for Medical Compression Stockings) in Germany,73 there may be considerable variation between the sizings of different manufacturers. Therefore it may be prudent for distributors and physicians who dispense stockings to carry multiple brands in the event that some patients experience a poor fit with certain makes. It may be estimated that 80% to 90% of patients seeking treatment for venous disease can be fitted with some form of ready-made stockings.
Custom-made stockings
Made-to-measure stockings should be prescribed under the following circumstances:
Prescription of a stocking
A common error made by the physician to avoid prescribing a made-to-measure stocking is that of prescribing the next larger size of a ready-made stocking. This results in a lower pressure being exerted at the ankle; in addition, the counter-pressures are altered because the wider stocking is designed at all levels for different leg measurements. Proper measurement and fit of a compression stocking becomes increasingly important when higher compression classes are required. Therefore, made-to-measure stockings have particular application for compression classes above 40 mmHg, as used, for example, in lymphedema.115
All manufacturers of compression stockings use a ‘standard’ wooden leg (the so-called Hohenstein leg), whose circumferences in each segment are circular.1 This is also true for the B segment (see Fig. 6.11), representing the ankle area, which is taken as the reference point for indicating the pressure class of the stocking. In real life, this B segment is the area in which the cross-section through a human leg shows the most extensive deviations from a circle.80 Here, the radius varies dramatically, being small over the malleoli and the Achilles tendon and even ‘negative’ between the inner ankle and the tendon. According to the law of Laplace, the compression pressure will therefore also change considerably, which explains the discrepancy between in vitro and in vivo measurements of interface pressure especially in this segment. However, a good correlation could be shown between the pressure ranges declared by the producers of high-quality stockings and the actual interface pressure exerted on the human leg.116
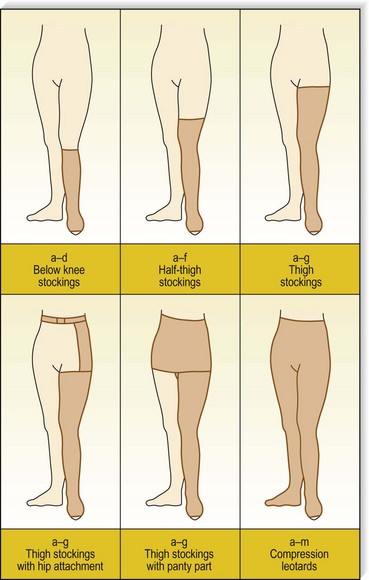
Stocking lengths
Up to six styles of medical compression stockings are available, depending on the manufacturer: knee-length, mid-thigh or high-thigh pantyhose or leotard, one-legged pantyhose, thigh with waist attachment, and maternity pantyhose. Some manufacturers have open-toed kinds available for some of the types, especially the single leg, high-thigh variety. Regardless of the style, most stockings are available in three lengths: knee length, mid thigh, and high thigh. According to the standardized figure, a knee-length stocking is designated as ‘AD’, a mid-thigh stocking as ‘AF’, and a (high) thigh-length stocking as ‘AG’ (see Fig. 6.11).
Pressure gradient
Graduation is not only a result of the leg circumference, it can also be added to a circular knit by altering the knitting construction from the ankle to the knee or thigh to reduce the tension from distal to proximal. Some studies have demonstrated that a pressure drop of 26% to 59% from the ankle to the thigh is desirable with graduated medical stockings.117–119
As previously explained, it is postulated that compression of the leg should be applied in a graduated manner to ensure and aid the optimal unidirectional flow of blood toward the heart and to avoid a proximal tourniquet effect. The measurement of an ideal pressure profile on the human leg depends on several factors, especially on the shape of the measuring point.120
It has to be considered that the pressure gradient postulated for compression hosiery is based on pressure readings on the smallest segment of a wooden leg model in the laboratory (B-point) presenting a circular cross-section. Owing to the fact that the human leg is flat or even concave at the corresponding medial ankle region, in vivo measurements at this point frequently show lower pressure values than at the B1-point 12 cm above (see Fig. 6.17).
New stockings have been introduced that exert a higher pressure over the calf than over the ankle area. These are easier to put on and are not only advocated in sports121 but also in venous patients.122
Donning medical compression stockings
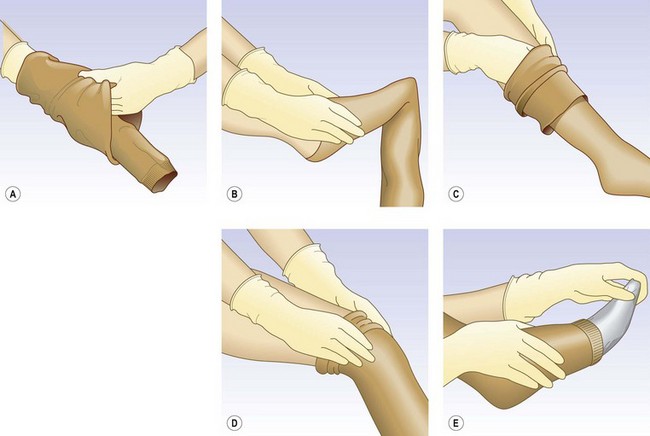
Before donning the stocking, the patient should be advised of the following considerations. Hand jewelry should be removed to avoid damaging the stockings. Fingernails should be smooth and relatively short. Rubber gloves are helpful and recommended both to prevent damage to the stockings from long fingernails and to grip the stocking. Talcum powder may be applied to the leg, or a light Perlon pantyhose or stocking may be worn under the compression stocking, to create a smoother leg over which to slide the stocking. Finally, satin foot ‘socks’ and foam-rubber foot pads provided by the stocking manufacturer are helpful in getting an open-toe stocking over the ankle (Fig. 6.25).
After preparing the foot and leg, turn the stocking inside out with the foot from the heel to the toe tucked into the stocking (Fig. 6.26A). Stretch the foot opening with the fingers or thumbs of both hands and pull the stocking foot over the foot up to the instep. Draw the stocking upward over the heel until pulling becomes difficult (Fig. 6.26B). Push the fold that forms across the instep and heel of the stocking over the heel. Finally, pull the stocking up in sections, always remembering not to pull it over long distances all at once but to proceed in small steps (Fig. 6.26C). When the stocking is applied without folds over the calf, the thigh section is then pulled over the knee (Fig. 6.26D). Finally, remove the foot ‘sock’ (Fig. 6.26E).
An application aid for compression stockings is also available from various compression stocking companies. These devices are cleverly designed, simple metal supports that make donning compression stockings easier, even when the stockings must be placed over compression padding (Fig. 6.27). The compression stocking is pulled over the half-circle bracket located on the front (open) side of the device so that the heel portion of the stocking is 2 to 3 inches (about 5–7.5 cm) below the top on the half-circle bracket. The heel portion is positioned facing the user, and the toe of the stocking is facing toward the open side of the device. The patient’s foot is then placed into the foot of the stocking until the foot is completely on the floor or until the heel is in place. The metal grips on either side are then used to pull the rest of the stocking onto the leg. Once the stocking is above the calf, the device may be pulled away and the remainder of the stocking then can be easily pulled up.
Patient compliance
Noncompliance is the most important factor limiting the use of compression stockings. The reasons for noncompliance can be grouped into two interdependent major categories: (1) wear-comfort factors and (2) the intangible sense of restriction imposed by the stockings.123
In addition to a measurable improvement in multiple parameters of CVI, a study on symptoms of CVI has demonstrated an improvement after 1 and 16 months of wearing graduated compression stockings.124 In this study, 112 patients with CVI and significant CEAP classification (clinical state [C], etiology [E], anatomy [A], and pathophysiology [P]) were treated with a 30- to 40-mmHg graduated compression stocking. Patients rated on a five-point scale the degree of swelling, pain, skin discoloration, cosmetic problems, activity tolerance, depression, and sleep problems caused by CVI. There were statistical improvements in all scores at 1 month, with continued improvement at 16 months. Most importantly, 70% of patients were still wearing their stockings at 16 months, demonstrating their comfort over the symptoms of CVI. This is in contrast with the impression of poor compliance and indicates improved comfort with modern compression stockings. Similar degrees of improvement were also demonstrated in 31 patients with CVI wearing low- or medium-grade stockings.125 There was no significant difference in symptoms in these patients despite the difference in graduated compression. Therefore, patients who cannot tolerate class II stockings should be fitted with class I stockings. Mild compression is better than no compression.
Patients’ compliance in wearing their compression stockings is frequently underestimated by the physicians. In a Canadian survey, physicians estimated that 50% of patients after DVT would wear compression stockings daily, 30% occasionally, and 20% would never wear them.126 In this study the most important reasons for noncompliance were thought to be discomfort (74%), hard to put on (71%), and high costs (53%). When the patients were asked, daily use was reported by 87%, once or twice weekly by 3%, less than once a week by 6%, and never or rarely by 4%. In a European follow-up of patients, it was shown that there is less swelling of the thrombosed leg when the stockings are still being worn 2 years after DVT compared to in those patients who stop compression therapy before this time and that most of those patients who still suffer from pronounced residual swelling use them.127
Care of the medical compression stocking
Because these stockings are worn on a daily basis in extremely close contact with the skin, they are subjected to considerable wear and tear. The chemical stresses from sweat, soaps, creams, and body oils, in addition to the physical stresses of the nearly continuous stretch and relaxation with movements of the leg, result in a gradual decline in the compressive effect of the stockings. This decline was measured in class II and class III stockings. Flat-knitted and round-knitted European class II stockings showed a mean pressure decrease from 29.3 to 26.5 mmHg after 3 months of daily wear. Strong stockings had a similar rate of decreasing pressure from 47.5 to 44.2 mmHg.128 Compression stockings, therefore, have a limited effective life. To ensure that they last as long as possible, special care is required.
Ideally, compression stockings should be washed every day. In fact, a study of six stocking types machine washed 15 times at 40°C demonstrated no decrease in resting pressure or elasticity.93 Therefore, if long-term use is required, it is best to provide the patient with two pairs of stockings that can be alternated between washings. Most compression stockings incorporating spandex can be machine washed on a fine-gentle cycle with warm (40°C) water. This gives a better cleansing action than hand washing. (Consult the manufacturer’s guidelines for specific instructions.) Gentle detergents without bleach or alkali are best. Gentle spinning after the washing cycle is harmless to compression stockings and quickens the drying process. Rather than being hang-dried from a line, compression stockings should be laid flat on a drying rack or towel. Low heat may be used in the drying process with most brands of compression stockings. With normal wear and proper care, compression stockings should have an effective life of 4 to 6 months.
Dangers, Complications and Contraindications
Because the degree of compression with manual bandages is unpredictable, arterial ischemia can occur. This is of concern particularly in the presence of venous leg ulcers during treatment. Two studies estimated the frequency of unsuspected arterial insufficiency among patients with chronic leg ulcers at 21%129 and 31%.130 Callam et al131 surveyed consultants in general surgery in Scotland regarding their experience with compression therapy in the previous 5 years and found 147 cases of cutaneous ulceration caused by the compression bandage. Of these consultants, 32% reported at least one case of ulceration or cutaneous necrosis aggravated by compression bandages; 21% reported more than one experience. Compression bandages accounted for 74 of 147 cases reported, with elastic and antiembolism stockings accounting for 36 and 38 cases, respectively. Also, eight patients were reported who required amputations of the digits or feet as a direct result of arterial ischemia caused by an excessively tight compression bandage or stocking. It has been estimated that up to 50% of patients over 80 years of age with leg ulcerations also have significant arterial disease.129 In a survey of 1416 venous reflux ulcers 13.6% had moderate and 2.2% had severe arterial disease.132
Consequently, the physician should always check arterial pulses before and after applying a compression bandage or fitting a compression stocking, especially in the elderly. Low-stretch bandages offer more safety in patients with arterial disease because these bandages can be applied with a very low resting pressure, achieving still-effective pressure peaks during ambulation. The natural history of such patients presenting with mixed ulceration has been described by Marston et al.133 Doppler ultrasound allows measurement of arterial pressure, which has to be done in every case before a high-pressure bandage is applied for the first time. An ankle–arm index of arterial pressure below 0.5 is considered to be a contraindication for compression.1,76,108
Sensory disturbances should be a warning for re-evaluating the degree of compression in the post-treatment period (see Chapter 8). If the patient suffers from diabetic neuropathy, a minimal pressure damage of the skin may stay unrecognized and may be the starting point of skin necrosis when the bandage or the stocking is not removed.
When firm compression bandages are applied to both legs, a considerable volume of blood can be shifted toward the heart.134 This can lead to an increase of the preload of the heart and affect cardiac output. Therefore, severe decompensated heart failure should be considered as a contraindication for bilateral firm bandages.
Clinical Indications for Compression Therapy
In a recent review all randomized controlled trials (RCTs) assessing the clinical efficacy of compression in venous and lymphatic disorders of the lower extremity have been published.135
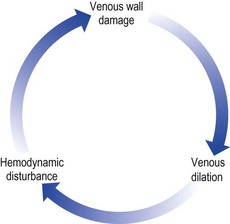
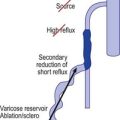
The use of compression alone in preventing varicose and telangiectatic leg veins
Varicose and telangiectatic leg veins progress when the volume and subsequent pressure of blood within the vessel lumen exceed the vessel’s capacity to enclose that volume. The deep venous system, by virtue of its position within a musculofibrous sheath, can accommodate such changes. Major parts of the superficial venous system are not enclosed in a rigid sheath. Thus, to accommodate the increase in flow, the vessel lumen increases in diameter. When this increase in diameter is supraphysiologic, the one-way valve cusps no longer meet and they become incompetent. This causes excessive pressure, with blood volume routed into smaller branching vessels, producing an abnormal dilation. This hemodynamic explanation of varicose vein development is best regarded as a vicious cycle (Fig. 6.28).
Externally supporting untreated varicose veins will narrow their diameter and decrease retrograde blood flow.136 External pressure may also provide a normalization of cutaneous blood flow. In support of this theory, improvement in cutaneous oxygenation has been demonstrated with the use of compression in patients with venous stasis after only 10 to 15 minutes.137
Patients with varicose veins note relief of aching symptoms with all classes of compression stockings.34,35,112 This has also been shown in a randomized controlled trial in patients with symptomatic varicose veins of pregnancy.138 Patients with postphlebitic limbs find that the 30- to 40-mmHg and 40- to 50-mmHg stockings control edema and symptoms better than do 20- to 30-mmHg stockings. It is interesting to note that although symptoms are improved with all classes of compression stockings, patients with varicose veins achieve physiologic improvement only when 30- to 40-mmHg and 40- to 50-mmHg compression stockings are worn. Therefore, 30- to 40-mmHg graduated compression stockings are best used for conservative treatment of varicose veins, and 40- to 50-mmHg compression stockings are best used for conservative treatment of CVI (see previous discussion).44
There are no RCTs available showing that compression is able to prevent the progression of venous disease.135,139
Rationale for the use of compression in varicose vein sclerotherapy
The basic concept of Fegan’s ‘empty vein technique’ is to keep the blood clot after injection of the sclerosing agent as small as possible.140–142 Postsclerotherapy compression primarily eliminates a thrombophlebitic reaction and substitutes a ‘sclerophlebitis’ with the production of a firm fibrous cord.143 Compression serves at least six purposes:
How much pressure is necessary for varicose veins?
Initial compression measurements taken during manual wrapping of the leg with Crevic crepe bandages by multiple surgeons using the technique of Fegan140 show an average between 20 and 100 mmHg with a mean of 54 mmHg at calf level.117 In addition, experimental varicose vein models have shown this level of compression to cause a reduction of the vessel lumina by 94%.117 Thus, the classic technique for compression sclerotherapy is theoretically sound.
The physician should consider the posture of the patient when prescribing compression stockings. If higher compression pressures are used (e.g. through the use of double stockings), care must be taken to inform patients to remove the outer stocking when not ambulatory. A sustained external pressure above 30 mmHg with elastic material applied to the leg of supine patients may impair peripheral blood circulation and skin temperature.100 Patients may perceive this as achiness in the ankle area that occurs during sleep and resolves with walking after 30- to 40-mmHg compression stockings have been worn to bed following sclerotherapy.
By having compression of 30 to 40 mmHg at the ankle, the compressive strength at other locations on the leg may be between 10 and 20 mmHg, depending on the site and amount of underlying bone, adipose tissue, and muscle.31 Experimental models have demonstrated that external pressures of 10 to 15 mmHg reduce the capacity of the underlying varicose vein only minimally.21,39,117 Therefore, with the use of this degree of compression, one does not attempt to completely empty intravascular blood from the treated veins.
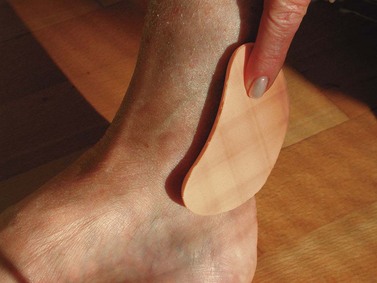
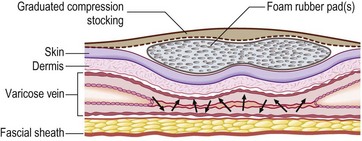
Local pads and rolls
In order to occlude a vein completely, the external pressure should exceed the intravenous pressure. In the standing position, the intravenous pressure is about 70 mmHg at the lower leg and about 30 mmHg at thigh level, depending on the body height. The pressure exerted by a compression stocking at thigh level is about 10 to 15 mmHg, which is too low to occlude the vein.21,110
By applying small rolls with different materials over the injected vein, this difficulty may be overcome, as demonstrated in Figure 6.30. When the injected vein is covered by a small rubber roll, a thigh-length compression stocking with a pressure of 15 to 20 mmHg may compress the vein even in the standing position.
The increase of pressure in a localized area by using narrow foam rubber pads under compression stockings has been described by several authors.151–156 Foam Sorbo pads (STD Pharmaceuticals, Hereford, England) (Fig. 6.31) are widely used in Great Britain.143 A new wedge-like rubber foam device (postop device, Medi, Bayreuth, Germany) has been developed specifically for compressing the great saphenous vein on the thigh (Fig. 6.33) and a very satisfying outcome after stripping operation was reported.45
Different types of pads do provide different pressures. A study by Hirai et al154 demonstrated pressure over the anterior tibia with a moderate-pressure stocking to be 20.3 mmHg without pads, 59.1 mmHg with a cotton pad or gauze pad, 73.5 mmHg with a foam rubber pad, and 76.5 mmHg with a hard rubber pad.
In addition to producing an increase in cutaneous pressure, their use, especially in the popliteal region, has decreased the incidence of abrasions from pressure stockings and tape, thereby improving patient comfort. In one physician’s practice,155 foam rubber pads have been noted to produce minor skin irritation (erythema) in up to 28% of patients. Another device for increasing local pressure is Molefoam (Scholl UK). This product comes in sheets of 7-mm thickness that may be cut easily to size. The adhesive side is covered with paper that is peeled away. Molefoam has a decreased incidence of local irritation (14% versus 28% for Sorbo pads). One study that compared the efficacy of sclerotherapy with Sorbo versus Molefoam showed no difference between the two groups.155
Another clever method for increasing local pressure is the use of rolls of cotton wool.156 The roll is secured with a nonelastic material. This method is advantageous for compressing long lengths of veins. A study of 100 patients (120 legs) with varicose veins treated with sclerotherapy, followed with long cotton wool rolls under compression stockings, found good results in all patients.156 Compression was given by a combination of European class I (daytime and night-time) and class II (daytime only) compression hosiery. Only three patients developed intravascular blood clots. The mean pressure under the pads was 84 mmHg (68–122 mmHg). In this study, cotton rolls and class I stockings were removed at 1 week and patients continued to wear class II stockings for an additional 3 weeks.
Local padding of the injected vein may considerably improve the emptying of the vein. Especially in the thigh region, a satisfactory compression of the veins by compression stockings may be a problem due to a markedly low pressure. In such cases, compression bandages with adhesive material applied over the local pressure rolls may be a good alternative.45,157
How long should compression be maintained?
In addition to the degree of compression needed to effect optimal sclerotherapy, the duration needed to maintain compression is also open for debate.158 The classic technique for sclerosis of varicose veins described by Fegan140,141 and used by Hobbs159 and Doran and White160 is to continue compression for 6 weeks. This period was not arrived at randomly but through multiple histologic examinations of sclerotherapy-treated varicose veins at intervals of 30 seconds; 1 and 5 minutes; 12, 24, and 36 hours; 6, 8, 12, and 14 days; 3, 4, 7, 10, 16, and 20 weeks; and 0.5, 1, and 5 years.161 Fegan concluded that organization of the fibrous occlusion required at least 6 weeks. However, a randomized study found no difference in clinical results at 2 years when compression was maintained for 3 weeks as compared with 6 weeks.162 Thus, many phlebologists recommend a maximum of 3 weeks of compression for varicose veins.
A review on RCTs regarding this question was recently published.133 Studies have shown that compression bandages maintain significant compression for only 6 to 8 hours while patients are ambulatory and lose up to 50% of their initial compression pressure in recumbent patients at 24 hours,151 thus questioning the rationale for prolonged use. After phlebectomy, bandaging for 1, 3, and 6 weeks did not show a difference in efficacy at 2 months postoperatively.163 However, in this study, compression with an elastic bandage was given to all groups for only 1 week, with the variable being a Tubigrip tube gauze (Seton Products, Montgomeryville, Pa., USA) applied only during the day, which provided minimal compression. Finally, a randomized study of the use of compressive bandages in the treatment of varicose veins with a 3-month follow-up was reported.164 The study demonstrated through both subjective and objective findings that 3 days of compression equaled the results at 6 weeks. This study used a Coban bandage dressing that may not maintain effective pressure beyond 8 hours.
A corollary to the amount of time necessary to effect adequate compression is whether it is necessary to continue compression while the patient is lying down or asleep. The authors recommend that some degree of compression be maintained at all times to ensure optimal contraction of the treated vein. In fact, studies have demonstrated that veins become more distensible during sleep.165 This has been postulated to occur as a result of respiratory factors or emotional factors during dream states. In addition, thrombogenesis after the sclerotherapy-induced injury to vascular endothelium is maximal 8 hours after treatment, which may be when the patient wishes to lie down (see Chapter 8). Compression here speeds deep venous blood flow to prevent thrombosis in the deep system after treatment. Finally, it may be impractical for patients to remove and reapply the stocking at night if they must get out of bed for any reason. Therefore, if a high degree of compression is required after treatment, the use of double stockings appears practical, since one of the stockings can be removed while the patient is lying down.
Some anatomic sites necessitate inventive measures to effect compression of the underlying varicose veins. Perhaps the most difficult area to compress on the leg is the vulvar region. The authors have found the ‘vulvar pad’ described by Nabatoff,166 as well as the V2-Supporter (Prenatal Cradle Inc, Hamburg, Mich.) described by Ninia,167 to be useful in this area.
Especially in France, there are colleagues who do not perform any compression after sclerotherapy of large veins.168 Based on a comparative study the general recommendation of using compression after foam-sclerotherapy of the great saphenous vein as a routine has recently been questioned.169
Sclerotherapy of small veins
Rationale for the use of compression in the treatment of telangiectasias
Although compression sclerotherapy is now standard practice in the treatment of varicose veins, its use in the treatment of smaller abnormal leg veins and telangiectatic ‘spider’ veins has never been adopted uniformly. Many European colleagues do not use any kind of compression after sclerotherapy of small veins.168 However, the same justification for the use of compression in larger veins should hold true for its use in smaller veins. Convincing results from a randomized controlled study are favouring the use of compression 23 to 32 mmHg hosiery for 3 weeks after sclerotherapy of small veins.170
Duffy171 has classified unwanted leg veins into six types based on clinical (and possibly functional) appearance (see Box 2.6). Types 1, 1A, and 1B are probably dilated venules, possibly with intimate and direct communication to underlying larger veins from which they are direct tributaries.172 Both Bodian173 and de Faria and Moraes174 have found on biopsy examination that such ‘telangiectasias’ are actually ectatic veins. Therefore, because a significant percentage of smaller spider veins occur in direct communication with larger varicose or reticular superficial veins, compression of the ‘feeder’ vein should decrease, if not eliminate, the blood flow to the smaller connected vessels. Thus, in addition to the effects of compression on the treated vessels themselves, compression of the entire leg should lead to a relatively stagnant blood flow in the feeder veins, which should allow for more effective endosclerosis of the treated vessel and a subsequent decreased risk of recanalization.
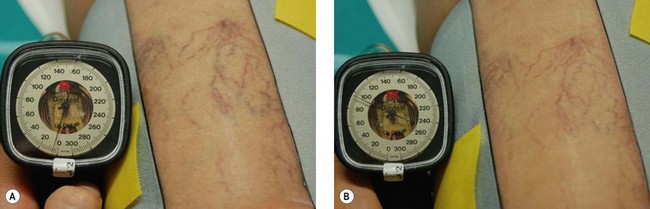
How much pressure is necessary to compress telangiectasias?
The only reported study measuring the pressure necessary to empty superficial ‘capillaries’ (telangiectasias) on the leg demonstrated that a sudden emptying of superficial cutaneous capillaries occurred between 40 and 60 mmHg at a point 5 cm above the medial malleolus while the patient was recumbent.175 However, 80 mmHg was required to produce a complete emptying of blood with the patient in a standing position. This degree of pressure can be obtained with a bandage wrapped over a local pad but not with graduated compression stockings on areas of the leg above the ankle.
One limitation to the use of compression stockings in treating leg telangiectasias is the lack of complete emptying of the treated telangiectasias when only one stocking is used. Theoretically, the incorporation of foam pads directly over the injected vessels and a double layer of compression stockings for daytime use, with one stocking removed on recumbency, should produce a more complete vascular occlusion (Fig. 6.34).
As shown in Figure 6.35 even very high pressure applied by a circular compression device is not able to compress small skin veins.
Based on serial biopsies performed by L. Wenner after sclerotherapy of small veins, Staubesand and Seydewitz were able to demonstrate by electron microscopy less thrombus formation using powerful local compression.176
A multicenter, bilateral comparative study through the North American Society of Phlebology (now the American College of Phlebology) examined the necessity for the use of a class II (30- to 40-mmHg) single stocking when treating leg telangiectasias.177 Thirty-seven women with bilaterally symmetric telangiectatic leg veins of less than 1 mm in diameter were evaluated. One set of vessels was compressed for 3 days with a 30- to 40-mmHg compression stocking (MediUSA, Arlington Heights, Ill.) over a cotton ball dressing. The alternate set of vessels had a cotton ball dressing applied for 2 hours with paper tape without an overlying compression stocking. With the stocking, a greater clinical resolution occurred after treatment with one sclerotherapy injection on vessels located on the distal leg, or when vessels were greater than 0.5 mm in diameter. Vessels located elsewhere or less than 0.5 mm in diameter showed no significant difference when this form of compression was used.
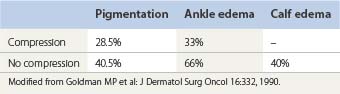
The main benefit of compression treatment was noted in the evaluation of adverse sequelae (Table 6.7).177 The most significant finding in this study was that 20 to 30 mmHg compression produced a relative decrease in postsclerotherapy hyperpigmentation, which fell from an incidence of 40.5% to 28.5% with the use of compression. In addition, ankle and calf edema were lessened if a graduated compression stocking was worn immediately after sclerotherapy.
How long should compression be maintained after sclerotherapy of small veins?
Formal studies on the use of compression in the treatment of leg telangiectasias are rare. A 3-day period for compression of leg telangiectasias is common based on the empirical report of Ouvry and Davy,147 who advised a minimum of 3 days to limit the development of peripheral inflammation and intravascular thrombosis. Without supporting information, Harridge178 recommended a 1-week period of compression for spider veins, using a local pressure band of elastic adhesive only.
A review concerning compression and its effects on compression sclerotherapy of reticular and telangiectatic legs veins has been reported.179 Forty patients were treated with sclerotherapy in three centers, followed by no compression or compression with 20- to 30-mmHg graduated stocking for 3 days, 1 week, or 3 weeks. A statistically significant improvement in hyperpigmentation and resolution was seen in patients treated with 3 weeks of compression. Patients treated with compression for 3 days or 1 week also had a greater degree of improvement than patients not treated with compression. Patients treated with compression for 1 or 3 weeks had the least amount of postsclerotherapy hyperpigmentation. The full benefits of compression were seen when patients were examined 6 months after a single treatment. The authors concluded that patients are best treated with either 1 or 3 weeks of compression after sclerotherapy, but that even 3 days of compression offers some improvement over no compression.
In another randomized controlled trial, the outcome of sclerotherapy with subsequent Elastoplast bandages was compared with the results after 35- to 40-mmHg stockings.180 After 3 to 6 weeks, the stocking group showed a higher success rate, less thrombosis, and less pigmentation.
Compression therapy after venous surgery and endovenous catheter procedures
Compression therapy is routinely performed after surgery of large varicose veins.181,182 According to M. Perrin, the possible short-term benefits of compression after surgery include prevention of superficial thrombophlebitis and DVT, improvement of wound healing, and reduction of pain, bruising, and hematoma. The level of activity, namely ambulation, is improved and early return to work can be accelerated.183
It could be demonstrated that high local compression achieved by using rubber foam pads on the thigh after surgery, and after laser abolition of the great saphenous vein, is able to reduce pain and hematoma (see Fig 6.33).45,184
Pregnancy
One randomized controlled trial came to the conclusion that compression stockings may be ineffective in preventing the development of small varicose veins and side branches during pregnancy but they alleviate leg symptoms and reduce the incidence of great saphenous vein reflux at the saphenofemoral junction.185
At the first indication of pregnancy, patients should be fitted with a 10- to 30-mmHg graduated pantyhose. In multiparous women, or in those with a history of varicose veins, a stronger (30- to 40-mmHg) pantyhose should be worn. In women with large legs, or in patients who are too uncomfortable with a 30- to 40-mmHg pantyhose, a calf-length, 20- to 30-mmHg compression stocking can be worn over a 20- to 30-mmHg pantyhose. One study comparing venous emptying between 13- and 25-mmHg ankle compression stockings used during pregnancy found no significant difference between the two compression levels. Patient compliance between the two classes of stockings was the same, with 82% of the 50 women continuing to wear the stocking throughout their pregnancy.186 Another study showed an improvement in maternal and fetal circulation, with best effects in the range of a 40-mmHg compression.187
Even for women in their 35th week of pregnancy, graduated compression stockings are able to increase expelled venous volume, whereas the refilling rate is influenced to a lesser degree, thus minimizing venous congestion in the leg.188 This has been demonstrated to decrease postural changes in heart rate, preventing the uterovascular syndrome.187,189 Using these guidelines, compression stockings worn during pregnancy can prevent or lessen the development of venous insufficiency. At the very least, the use of 25-mmHg graduated compression stockings decreased subjective discomfort from 82% to 13% in pregnant women between 30 and 40 weeks’ gestation and decreased edema from 75% to 14% in these pregnant women.189
Edema due to sitting and standing, occupational edema
The rationale described in the previous section also applies to most other forms of venous stasis disease. Graduated-compression stockings are helpful to patients in occupations that necessitate standing for long periods. Light-compression stockings may be effective.190–192 By measuring the physiologic swelling of the legs after a working day using water-displacement volumetry, it could be demonstrated that light support stockings were able to significantly reduce evening edema. Compression stockings with an interface pressure of 18 mmHg on the distal leg were able to prevent the swelling after a working day completely.6
Light-compression stockings may also improve subjective symptoms of heaviness that occur after long sitting or standing.7,34,35 A long flight or a car or bus drive for several hours is a typical situation in which leg swelling is a common sign, frequently also connected with subjective symptoms.193–196 Considerable fluid accumulation in the legs of about 250 mL was measured after long-haul flights. The increase of skin thickness over the shin was even maintained for some days after the flight.195
The clinical benefits of lightweight compression stockings were shown in flight attendants.35 A crossover prospective study of 19 flight attendants wearing 8- to 15-mmHg and/or 15- to 20-mmHg graduated stockings demonstrated a statistically significant reduction in leg discomfort, ankle swelling, aching, and tiredness in the leg. Interestingly, in this population in which almost all patients had leg telangiectasia (with one person having varicose veins), wearing 15- to 20-mmHg stockings did not significantly improve symptoms over the lighter-strength stockings. Light stockings have been reported to reduce the incidence of flight thrombosis.197
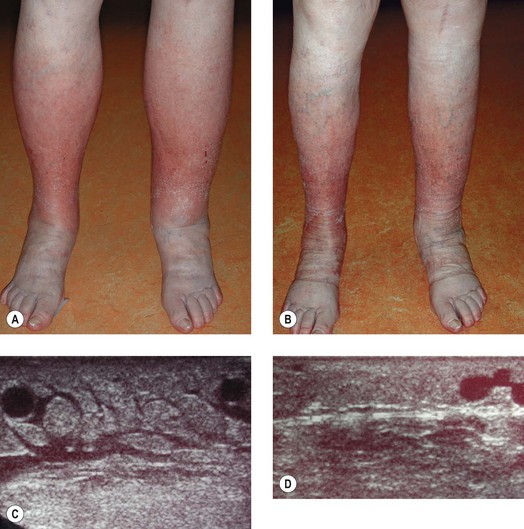
Severe stages of edema can be dramatically improved by compression bandages (Fig. 6.36). In chronic edema leading to lipodermatosclerosis on the distal leg the lymphatics ultimately decompensate. Consequent compression therapy is able to reverse the skin changes and restore normal lymphatic drainage (see Fig. 6.2). For patients who have difficulty donning and doffing compression stockings or compression bandages, the CircAid legging is a viable option and may aid in patient compliance and comfort.
Additional intermittent pneumatic compression can further help to reduce edema in these patients.198
Prevention of deep vein thrombosis and post-thrombotic syndrome
Several RCTs and systematic reviews have shown the beneficial effects of compression in preventing venous thromboembolic diseases in bedridden patients. More studies have been performed with intermittent pneumatic compression than with stockings.183,199–201 Recent guidelines recommend combined pharmacologic and mechanical prophylaxis, assuming that mechanical methods may increase efficacy and reduce death and morbidity rates without increasing bleeding risk, and suggest that mobile patients with DVT should remain ambulant.202
Signs and symptoms of a post-thrombotic syndrome after proximal DVT may be dramatically reduced if compression stockings are worn in the following years.203–206 Immediate compression and mobilization in the acute stage of DVT seems to further reduce the incidence and severity of post-thrombotic syndrome.127 Based on this evidence, it would be unethical to withhold compression stockings to a patient after DVT. We recommend to wear the stockings for 2 years, and to continue when there are still signs and symptoms like swelling and pain. However, one randomized crossover trial could not show a pain-relief effect of 30-mmHg knee-length compression stockings during walking in patients after DVT.207 It would be worthwhile to repeat these experiments with bandages or stockings exerting higher pressure and higher stiffness.
Treatment of superficial phlebitis, deep vein thrombosis, and post-thrombotic syndrome
Acute superficial phlebitis is an excellent indication for strong compression, preferably by adhesive bandages, especially when thigh veins are also involved. The same is true for phlebitic reactions after sclerotherapy. The patient should be encouraged to walk (see Fig. 6.16). This regimen is completely based on experience. Up to now there are no RCTs available demonstrating the beneficial effects of compression therapy in this important indication.
In acute DVT of mobile outpatients, good compression and immediate ambulation is able to reduce pain and swelling and to prevent thrombus growth.208,209 This adjunctive treatment always has to be accompanied by exact anticoagulation, preferably with therapeutic doses of low-molecular-weight heparin (LMWH). Firmly applied Fischer bandages in addition to an adhesive thigh bandage exerting a pressure of 40 mmHg showed better results than a thigh-length European class II compression stocking (Sigvaris 503, Ganzoni, Switzerland). Both methods, bandage or stocking, were much better than bed rest.208,209 However, for those centers which are not familiar with applying appropriately strong short-stretch bandages, good compression stockings may be a valuable alternative. In 1289 consecutive patients with DVT treated by compression bandages, walking exercises, and LMWH, the complication rate of symptomatic pulmonary embolism and of fatal events was much lower than in reports from the literature regarding immobilizing the patients.210 Our recommendation of immediate walking exercises with good compression is in contrast to the clinical routine in many countries. A survey from Canada reported that compression stockings were prescribed in the acute stage of DVT only by 26% of physicians, and that 68% prescribed stockings only if venous signs and symptoms were present.126
Immediate mobilization of the patient with acute DVT with good compression is also able to reduce the incidence of post-thrombotic syndrome.127 However, reports on the treatment of patients with a manifest post-thrombotic syndrome are scarce.211
Venous ulcers
There is no other indication for which the clinical efficacy of compression treatment has been so well established by numerous randomized controlled trials.96,97,183 However, the different compression devices in use require more work in conjunction with measurement of interface pressure and stiffness in the individual patients who are enrolled in comparative trials, in order to achieve reliable comparisons between various products.
Most studies have been undertaken using compression bandages. The following conclusions may be derived from several RCTs and systematic reviews:96,97
Compared with local therapy alone, compression achieves significantly faster healing rates of venous ulcers. The augmentation of sustained compression with sequential pneumatic compression promotes ulcer healing.212 With adequate compression therapy, 70% of consecutive outpatients with venous ulcers should be healed after 12 weeks. Reports with healing rates lower than 50% raise the suspicion that the technique used was inadequate.1 This is also true for randomized studies comparing different compression regimens or trying to demonstrate the supplementary effect of drugs. In future studies comparing different materials, it is highly recommended that the sub-bandage pressure be measured, since this parameter is of deciding importance for the healing of venous ulcers.96,97,183 With optimal compression therapy, baseline ulcer area and ulcer duration are significant predictors of ulcer healing.213
If the ulcers are not too large and not too longstanding, favorable results can also be achieved with compression stockings.99,214–218 Some stockings were developed specifically for treating venous ulcers: ‘two-layer stockings’ with a basic liner to keep the ulcer dressing in place and a second outer stocking, thereby enhancing pressure and stiffness, e.g. UlcerCARE coming with a zip (Beiersdorf-Jobst, Charlotte, N.C.), Mediven ulcer kit (Medi, Bayreuth, Germany), Venotrain ulcertec (Bauerfeind, Zeulenroda, Germany) with a specifically designed kitting pattern in order to increase the stiffness in the gaiter area,217 and Tubulcus (Innothera, Paris, France), which is a ready-made tubular compression device.219,220
It can be more difficult to keep a venous ulcer closed than to heal it. Noncompliance of the patient regarding wearing compression stockings is associated with a higher recurrence rate.221 Recurrence after healing of leg ulcers was shown to be significantly lower if compression stockings with higher pressure were used.222 For the insurance companies, it would be much cheaper to reimburse for compression stockings after the ulcers are healed than to pay the costs for ulcer recurrences.223
Lymphedema
Multilayer short-stretch bandages are essential to achieve optimal edema reduction.90,224 Bandaging and subsequent elastic hosiery is more effective than elastic hosiery alone in reducing lymphedema.224,225 Due to the fast diminution of limb volume, the bandages will loosen rapidly89 and should be reapplied in the initial phase at least once a day. To maintain the effect and to prevent refilling of the extremity with edema, lifelong wearing of compression hosiery, preferably made-to-measure, is essential.
1 Partsch H, Rabe E, Stemmer R. Compression therapy of the extremities. Paris: Editions Phlébologiques Francaises; 1999.
2 Orbach EJ. Compression therapy of vein and lymph vessel diseases of the lower extremities. Angiology. 1979;30:95.
3 Hohlbaum GG. Die Geschichte der Kompressionstherapie. Phlebol Proktol. 1988;17:24.
4 Fischer H. Eine neue Therapie der Phlebitis. Med Klin. 1910;14:1172.
5 Watson J. Observations on the nature and treatment of telangiectasis or that morbid state of the blood-vessels which gives rise to naevus and aneurism from anastomosis. Presented at the New York Medical and Surgical Society, March 2, 1839.
6 Partsch H, Winiger J, Lun B. Compression stockings reduce occupational swelling. Dermatol Surg.. 2004;30:737.
7 Vayssairat M, Ziani E, Houot B. Placebo controlled efficacy of class 1 elastic stockings in chronic venous insufficiency of the lower limbs. J Mal Vasc. 2000;25:256.
8 Pierson S, Pierson D, Swallow R, Johnson GJr. Efficacy of graded elastic compression in the lower leg. JAMA. 1983;249:242.
9 Gniadecka M, Karlsmark T, Bertram A. Removal of dermal edema with class I and II compression stockings in patients with lipodermatosclerosis. J Am Acad Dermatol. 1998;39:966.
10 Partsch H. Understanding the pathophysiological effects of compression. In: Position document EWMA: Understanding compression therapy. London: MEP; 2003.
11 Arpaia G, Mastrogiacomo O, Peliccioni E, et al. Compression therapy improves the quality of life in patients with venous insufficiency. Acta Phlebol. 2003;3:125.
12 Földi E, Jünger M, Partsch H. The science of lymphoedema bandaging. In: Position document EWMA: Lymphoedema bandaging in practice. London: MEP; 2005.
13 Földi E, Sauerwald A, Hennig B. Effect of complex decongestive physiotherapy on gene expression for the inflammatory response in peripheral lymphedema. Lymphology. 2000;33:19.
14 Fagrell B. Vital microscopy in the pathophysiology of deep venous insufficiency. In: Eklof B, Gjöres JE, Thulesius O, Bergqvist D, editors. Controversies in the management of venous disorders. London: Butterworth, 1989.
15 Partsch H, Mostbeck A, Leitner G. Experimentelle Untersuchungen zur Wirkung einer Druckwellenmassage (Lymphapress) beim Lymphödem. Z Lymphol. 1981;5:35.
16 Olszewski WL. Lymph pressure and flow in limbs. In: Olszewski WG, editor. Lymph stasis: pathophysiology, diagnosis and treatment. Boca Raton: CRC Press, 1991.
17 Olszewski WL. Contractility patterns of human leg lymphatics in various stages of obstructive lymphedema. Ann N Y Acad Sci. 2008;1131:110.
18 Franzeck UK, Spiegel I, Fischer M, et al. Combined physical therapy for lymphedema evaluated by fluorescence microlymphography and lymph capillary pressure measurements. J Vasc Res. 1997;34:306.
19 Haid H, Lofferer O, Mostbeck A, Partsch H. Die Lymphkinetik beim postthrombotischen Syndrom unter Kompressionsverbänden. Med Klin. 1968;63:754.
20 Partsch H. Compression therapy of the legs. Dermatol Surg Oncol. 1991;17:799.
21 Partsch B, Partsch H. Calf compression pressure required to achieve venous closure from supine to standing position. J Vasc Surg. 2005;42:734.
22 Partsch H, Kahn P. Venöse Strömungsbeschleunigung in Bein und Becken durch ‘Anti-Thrombosestrümpfe’. Klinikarzt. 1982;11:609.
23 Sigel B, Edelstein AL, Savitch L, et al. Type of compression for reducing venous stasis: a study of lower extremities during inactive recumbency. Arch Surg. 1975;110:171.
24 Arcelus JI, Caprini JA, Traverso CI, et al. The role of elastic compression stockings in prevention of venous dilatation induced by a reverse Trendelenburg position. Phlebology. 1993;8:111.
25 Christopoulos DG, Nicolaides AN, Szendro G, et al. Air-plethysmography and the effect of elastic compression on venous hemodynamics of the leg. J Vasc Surg. 1987;5:148.
26 Christopoulos D, Nicolaides AN, Belcaro G. The long-term effect of elastic compression on the venous haemodynamics of the leg. Phlebology. 1991;6:85.
27 Gjores JE, Thulesius O. Compression treatment in venous insufficiency evaluated with foot volumetry. Vasa. 1977;6:364.
28 Gronbaek K, et al. The effect of the Lastosheer stocking on venous insufficiency. Phlebology. 1991;6:198.
29 Zajkowski PJ, Proctor MC, Wakefield TW, et al. Compression stockings and venous function. Arch Surg. 2002;137:1064.
30 Ibegbuna V, Delis KT, Nicolaides AN, Aina O. Effect of elastic compression stockings on venous hemodynamics during walking. J Vasc Surg. 2003;37:420.
31 Partsch H. Do we need firm compression stockings exerting high pressure? Vasa. 1984;13:52.
32 Norgren L. Elastic compression stockings – an evaluation with foot volumetry, strain-gauge plethysmography and photoplethysmography. Acta Chir Scand. 1988;154:505.
33 Chauvean M, Agbomson F. Force de compression et symptomologie de l’insuffisance veineuse fonctionnelle des members inferieurs: efficacite comparee de six degrees de contention. Phlebologie. 1997;50:731.
34 Benigni JP, Sadoun S, Allaert FA, Vin F. Comparative study of the effectiveness of class 1 compression stockings on the symptomatology of early chronic venous disease. Phlebologie. 2003;56:117.
35 Weiss RA, Duffy D. Clinical benefits of lightweight compression: reduction of venous-related symptoms by ready-to-wear lightweight gradient compression hosiery. Dermatol Surg. 1999;25:701.
36 O’Donnell TFJr, Rosenthal DA, Callow AD, et al. Effect of elastic compression on venous hemodynamics in postphlebitic limbs. JAMA. 1979;242:2766.
37 Partsch H. Improvement of venous pumping function in chronic venous insufficiency by compression depending on pressure and material. Vasa. 1984;13:58.
38 Sarin S, Scurr JH, Coleridge Smith PD. Mechanism of action of external compression on venous function. Br J Surg. 1992;79:498.
39 Partsch H, Menzinger G, Borst-Krafek B, Groiss E. Does thigh compression improve venous hemodynamics in chronic venous insufficiency? J Vasc Surg. 2002;36:948.
40 Partsch B, Mayer W, Partsch H. Improvement of ambulatory venous hypertension by narrowing of the femoral vein in congenital absence of venous valves. Phlebology. 1992;7:101.
41 Mosti G, Mattaliano V, Partsch H. Inelastic compression increases venous ejection fraction more than elastic bandages in patients with superficial venous reflux. Phlebology. 2008;23:287.
42 Mayberry JC, Moneta G, De Frang RD, Porter JM. The influence of elastic stockings on deep venous hemodynamics. J Vasc Surg. 1991;13:91.
43 Partsch H, Menzinger G, Mostbeck A. Inelastic leg compression is more effective to reduce deep venous refluxes than elastic bandages. Dermatol Surg. 1999;25:695.
44 Stöberl C, Gabler S, Partsch H. Indikationsgerechte Bestrumpfung – Messung der venösen Pumpfunktion. Vasa. 1989;18:35.
45 Mosti G, Mattaliano V, Arleo S, Partsch H. Thigh compression after great saphenous surgery is more effective with high pressure. Int Angiol. 2009;28:274.
46 Allegra C, Oliva E, Sarcinella R. Hemodynamic modifications induced by compression therapy in CVI evaluated by microlymphography. Phlebology. 1995;10(Suppl 1):1138.
47 Onorati D, Rossi GG, Idiazabal G. Effect of elastic stockings on edema related to chronic venous insufficiency: videocapillaroscopic assessment. J Mal Vasc. 2003;28:21.
48 Klopp R, Schippel W, Niemer W. Compression therapy and microcirculation: vital microscope investigations in patients suffering from chronic venous insufficiency before and after compression therapy. Phlebology. 1996;11(Suppl 1):19.
49 Abu-Own A, Scurr JH, Coleridge Smith PD. Effect of compression on the skin microcirculation in chronic venous insufficiency. Phlebology. 1995;10:5.
50 Abu-Own A, Shami SK, Chittenden SJ, et al. Microangiopathy of the skin and the effect of leg compression in patients with chronic venous insufficiency. J Vasc Surg. 1994;19:1074.
51 Belcaro G, Gaspari L, Legnini M, et al. Evaluation of the effects of elastic compression in patients with chronic venous hypertension by laser-Doppler flowmetry. Acta Chir Belg. 1988;88:163.
52 Galler S, Klyscz T, Jung MF, et al. Clinical efficacy of compression therapy and its influence on cutaneous microcirculation. Phlebology. 1995;10(Suppl 1):907.
53 Hammersen F, Hesse G. Strukturelle Veränderungen der varikösen Venenwand nach Kompressionsbehandlung. Phlebol Proktol. 1990;19:193.
54 Kahle B, Idzko M, Norgauer J, et al. Tightening tight junctions with compression therapy. J Invest Dermatol. 2003;121:1228.
55 Partsch Horakova MA, Mayer W, Partsch H. Paramètres microcirculatoires, prédiction de la tendance à la cicatrisation des ulcères de jambe. Phlébologie. 1996;49:461.
56 Dai G, Tsukurov O, Chen M, et al. Endothelial nitric oxide production during in vitro simulation of external limb compression. Am J Physiol Heart Circ Physiol. 2002;282:H2066.
57 Herouy Y, Kahle B, Idzko M, et al. Tight junctions and compression therapy in chronic venous insufficiency. Int J Mol Med. 2006;18:215.
58 Beidler SK, Douillet CD, Berndt DF, et al. Inflammatory cytokine levels in chronic venous insufficiency ulcer tissue before and after compression therapy. J Vasc Surg. 2009;49:1013.
59 Oduncu H, Clark M, Williams RJ. Effect of compression on blood flow in lower limb wounds. Int Wound J. 2004;1:107.
60 Mayrovitz HN, Larsen PB. Effects of compression bandaging on leg pulsatile blood flow. Clin Physiol. 1997;17:105.
61 Mayrovitz HN, Delgado M, Smith J. Compression bandaging effects on lower extremity peripheral and sub-bandage skin blood perfusion. Ostomy Wound Manage. 1998;44:56.
62 Mayrovitz HN, Sims N. Effects of ankle-to-knee external pressures on skin blood perfusion under and distal to compression. Adv Skin Wound Care. 2003;16:198.
63 Van Bemmelen PS, Weiss-Olmanni J, Ricotta JJ. Rapid intermittent compression increases skin circulation in chronically ischemic legs with infra-popliteal arterial obstruction. Vasa. 2000;29:47.
64 Delis KT, Labropoulos N, Nicolaides AN, et al. Effect of intermittent pneumatic foot compression on popliteal artery haemodynamics. Eur J Vasc Endovasc Surg. 2000;19:270.
65 Delis KT, Nicolaides AN, Wolf JH, Stansby G. Improving walking ability and ankle brachial pressure indices in symptomatic peripheral vascular disease with intermittent pneumatic foot compression: a prospective controlled study with one-year follow-up. J Vasc Surg. 2000;31:650.
66 Delis KT, Nicolaides AN. Effect of intermittent pneumatic compression of foot and calf on walking distance, hemodynamics, and quality of life in patients with arterial claudication: a prospective randomized controlled study with 1-year follow-up. Ann Surg. 2005;241:431.
67 Morris RJ, Woodcock JP. Intermittent venous compression and the duration of hyperemia in the common femoral artery. Clin Physiol Funct Imaging. 2004;24:237.
68 Ramaswami G, D’Ayala M, Hollier LH, et al. Rapid foot and calf compression increases walking distance in patients with intermittent claudication: results of a randomized study. J Vasc Surg. 2005;41:794.
69 European Committee for Standardization (CEN). Adopted European Prestandard: Medical compression hosiery, ENV 12718. Brussels: CEN; 2001.
70 Partsch H, Clark M, Mosti G, et al. Classification of compression bandages: practical aspects. Dermatol Surg. 2008;34:600.
71 Benigni JP, Uhl JF, Cornu-Thénard A, Blin E. Compression bandages: influence of techniques of use on their clinical efficiency and tolerance. Int Angiol. 2008;27:68.
72 British Standards Institution (BSI). Medical compression hosiery, BS 6612, BS 7505. London: BSI; 1995.
73 Medizinische Kompressionsstrümpfe, Gütesicherung RAL-GZ 387. Berlin: Beuth Verlag, 2000.
74 Neumann HAM. Compression therapy with medical elastic stockings for venous disease. Dermatol Surg. 1998;24:765.
75 Thomas S. Bandages and bandaging: the science behind the art. Care Science and Practice. 1990;8:56.
76 Vin F, Benigni JP. Compression therapy. International Consensus Document Guidelines according to scientific evidence. Int Angiol. 2004;23:317.
77 Wienert V. Die medizinische Kompressionstherapie. Berlin: Blackwell; 1999.
78 Fentem PH, Goddard M, Gooden BA. The pressure exerted on superficial veins by support hosiery. J Physiol. 1976;263:151P.
79 Partsch H. The static stiffness index (SSI) – a simple method to assess the elastic property of compression material in vivo. Dermatol Surg. 2005;31:625.
80 Stolk R, Wegen van der-Franken CPM, Neumann HAM. A method for measuring the dynamic behaviour of medical compression hosiery during walking. Dermatol Surg. 2004;30:729.
81 Partsch H, Clark M, Bassez S, et al. Measurement of lower leg compression in vivo: recommendations for the performance of measurements of interface pressure and stiffness: a consensus statement. Dermatol Surg. 2006;32:229.
82 Van Geest AJ, Veraart JC, Nelemans P, Neumann HA. The effect of medical elastic compression stockings with different slope values on edema. Measurements underneath three different types of stockings. Dermatol Surg. 2000;26:244.
83 Murthy G, Ballard RE, Breit GA, et al. Intramuscular pressures beneath elastic and inelastic leggings. Ann Vasc Surg. 1994;8:543.
84 Mosti G, Mattaliano V, Partsch H. Influence of different materials in multicomponent bandages on pressure and stiffness of the final bandage. Dermatol Surg. 2008;34:631.
85 Partsch H. The use of pressure change on standing as a surrogate measure of the stiffness of a compression bandage. Eur J Vasc Endovasc Surg. 2005;30:415.
86 Callam MJ, et al. Effect of posture on pressure profiles obtained by three different types of compression. Phlebology. 1991;6:79.
87 Veraart JC, Daamen E, Neumann HA. Short stretch versus elastic bandages: effect of time and walking. Phlebologie. 1997;26:19.
88 Hirai M. Changes in interface pressure under elastic and short-stretch bandages during posture changes and exercise. Phlebology. 1998;13:25.
89 Damstra RJ, Brouwer ER, Partsch H. Controlled, comparative study of relation between volume changes and interface pressure under short-stretch bandages in leg lymphedema patients. Dermatol Surg. 2008;34:773.
90 Moffatt CJ, Morgan P, Doherty P. The lymphedema framework: a consensus on lymphedema bandaging. In: Position Document EWMA: Lymphoedema bandaging in practice. London: MEP; 2005.
91 Dale JJ, Ruckley CV, Gibson B, et al. Multi-layer compression: comparison of four different four-layer bandage systems applied to the leg. Eur J Vasc Endovasc Surg. 2004;27:94.
92 Hafner J, Botonakis I, Burg G. A comparison of multilayer bandage systems during rest, exercise, and over 2 days of wear time. Arch Dermatol. 2000;136:857.
93 Blair SD, Wright DD, Backhouse CM, et al. Sustained compression and healing of chronic venous ulcers. Br Med J. 1988;297:1159.
94 Partsch H, Damstra RJ, Tazelaar DJ, et al. Multicentre, randomised controlled trial of four-layer bandaging versus short-stretch bandaging in the treatment of venous leg ulcers. Vasa. 2001;30:108.
95 Franks PJ, Moody M, Moffatt CJ, et al. Randomized trial of cohesive short-stretch versus four-layer bandaging in the management of venous ulceration. Wound Repair Regen. 2004;12:157.
96 O’Meara S, Cullum NA, Nelson EA Compression for venous leg ulcers. Cochrane Database Syst Rev 2009 Jan 21;(1):CD000265
97 Fletcher A, Cullum N, Sheldon TA. A systematic review of compression treatment for venous leg ulcers. Br Med J. 1997;315:576.
98 Cornu-Thenard A, Boivin P, Carpentier PH, et al. Superimposed elastic stockings: pressure measurements. Dermatol Surg. 2007;33:269.
99 Horakova MA, Partsch H. Ulcères de jambe d’origine veineuse: indications pour les bas de compression? Phlébologie. 1994;47:53.
100 Yamaguchi K, Gans H, Yamaguchi Y, Hagisawa S. External compression with elastic bandages: its effect on the peripheral blood circulation during skin traction. Arch Phys Med Rehabil. 1986;67:326.
101 Keller A, Müller ML, Calow T, et al. Bandage pressure measurement and training: simple interventions to improve efficacy in compression bandaging. Int Wound J. 2009;6:324.
102 Lorgren RA, Thomas S, Harding EF, et al. A comparison of sub-bandage pressures produced by experienced and inexperienced bandagers. J Wound Care. 1992;1:23.
103 Nelson EA, Ruckley CV, Barbenel JC. Improvements in bandaging technique following training. J Wound Care. 1995;4:181.
104 Nelson EA, Brown DA, Gibson B, et al. A study of nurses bandaging techniques using elastic and inelastic bandages [1]. Negas D, editor. Phlebology ’95. 1995, 883.
105 Moore Z. Compression bandaging: are practitioners achieving the ideal sub-bandage pressures? J Wound Care. 2002;11:265.
106 Hirai M. Interface pressure under elastic stockings with compression pads during posture changes and exercise. Phlebology. 1999;14:71.
107 Hafner J, Luthi W, Hanssle H, et al. Instruction of compression therapy by means of interface pressure measurement. Dermatol Surg. 2000;26:481.
108 Buhs CL, Bendick PJ, Glover JL. The effect of graded compression elastic stockings on the lower leg venous system during daily activity. J Vasc Surg. 1999;30:380.
109 Abdelmoumene Y, Chevallier P, Barghouth G, et al. Optimization of multidetector CT venography performed with elastic stockings on patients’ lower extremities: a preliminary study of nonthrombosed veins. AJR Am J Roentgenol. 2003;180:1093.
110 Lord RS, Hamilton D. Graduated compression stockings (20–30 mmHg) do not compress leg veins in the standing position. Aust N Z J Surg. 2004;74:581.
111 Aryal K, Dodds SR, Chukwulobelu R. Effect of posture on the pressure exerted by below-knee class II compression stockings on normal subjects. Phlebology. 2002;17:32.
112 Jones NAG, Webb PJ, Rees RI, Kakkar VV. A physiological study of elastic compression stockings in venous disorders of the leg. Br J Surg. 1980;67:569.
113 Arpaia G, Mastrogiacomo O, Pelicioni E, et al. Influence of elastic compression on venous return in athletes. Acta Phlebol. 2002;3:69.
114 Dinn E, Henry M. Treatment of venous ulceration by injection sclerotherapy and compression hosiery: a 5-year study. Phlebology. 1992;7:23.
115 Johnson GJr, Kupper C, Farrar DJ, et al. Graded compression stockings: custom vs noncustom. Arch Surg. 1982;117:69.
116 Partsch H, Partsch B, Braun W. Interface pressure and stiffness of ready made compression stockings: comparison of in vivo and in vitro measurements. J Vasc Surg. 2006;44:809.
117 Fentem PH, Goddard M, Gooden BA, et al. Control of distension of varicose veins achieved by leg bandages, as used after injection sclerotherapy. Br Med J. 1976;25:725.
118 Horner J, Lowth LC, Nicolaides AN. A pressure profile for elastic stockings. Br Med J. 1980;280:818.
119 Van den Berg E, Borgnis FE, Bolliger AA, et al. A new method for measuring the effective compression of medical stockings. Vasa. 1982;11:117.
120 Liu R, Kwok YL, Li Y, et al. Objective evaluation of skin pressure distribution of graduated elastic compression stockings. Dermatol Surg. 2005;31:615.
121 Garreau C, Pibourdin JM, Nguyen Le C, Boisseau MR. Elastic compression in golf competition. J Mal Vasc. 2008;33:250.
122 Couzan S, Assante C, Laporte S, et al. Booster study: comparative evaluation of a new concept of elastic stockings in mild venous insufficiency. Presse Med. 2009;38:355.
123 Raju S, Hollis K, Neglen P. Use of compression stockings in chronic venous disease: patient compliance and efficacy. Ann Vasc Surg. 2007;21:790.
124 Motykie GD, Caprini JA, Arcelus JI, et al. Evaluation of therapeutic compression stockings in the treatment of chronic venous insufficiency. Dermatol Surg. 1999;25:116.
125 Jungbeck C, Thulin I, Darenheim C, Norgren L. Graduated compression treatment in patients with chronic venous insufficiency: a study comparing low and medium grade compression stockings. Phlebology. 1997;12:142.
126 Kahn SR, Elman E, Rodger MA, Wells PS. Use of elastic compression stockings after deep venous thrombosis: a comparison of practices and perceptions of thrombosis physicians and patients. J Thromb Haemost. 2003;1:500.
127 Partsch H, Kaulich M, Mayer W. Immediate mobilisation in acute vein thrombosis reduces post-thrombotic syndrome. Int Angiol. 2004;23:206.
128 Veraart JC, Daamen E, de Vet HC, Neumann HA. Elastic compression stockings: durability of pressure in daily practice. Vasa. 1997;26:282.
129 Callam MJ, Harper DR, Dale JJ, Ruckley CV. Arterial disease in chronic leg ulceration: an underestimated hazard? Lothian and Forth Valley leg ulcer study. Br Med J (Clin Res Ed). 1987;294:929.
130 Cornwall JV, Dore CJ, Lewis JD. Leg ulcers: epidemiology and aetiology. Br J Surg. 1986;73:693.
131 Callam MJ, Ruckley CV, Dale JJ, Harper DR. Hazards of compression treatment of the leg: an estimate from Scottish surgeons. Br Med J (Clin Res Ed). 1987;295:1382.
132 Humphreys ML, Stewart AH, Gohel MS, et al. Management of mixed arterial and venous leg ulcers. Br J Surg. 2007;94:1104.
133 Marston WA, Davies SW, Armstrong B, et al. Natural history of limbs with arterial insufficiency and chronic ulceration treated without revascularization. J Vasc Surg. 2006;44:108.
134 Mostbeck A, Partsch H, Peschl L. Änderungen der Blutvolumenverteilung im Ganzkörper unter physikalischen und pharmakologischen Maßnahmen. Vasa. 1977;6:137.
135 Partsch H, Flour M, Smith PC. International compression club: indications for compression therapy in venous and lymphatic disease consensus based on experimental data and scientific evidence. Under the auspices of the IUP. Int Angiol. 2008;27:193.
136 Volkmann E, Falk A, Holm J, et al. Effect of varicose vein surgery on venous reflux scoring and plethysmographic assessment of venous function. Eur J Vasc Endovasc Surg. 2008;36:731.
137 Rooke TW, Hollier LH, Hallett JW, Osmundson PJ. The effect of elastic compression on TcPO2 in limbs with venous stasis. Phlebology. 1987;2:23.
138 Thaler E, Huch R, Huch A, Zimmermann R. Compression stockings prophylaxis of emergent varicose veins in pregnancy: a prospective randomised controlled study. Swiss Med Wkly. 2001;131:659.
139 Palfreyman SJ, Michaels JA. A systematic review of compression hosiery for uncomplicated varicose veins. Phlebology. 2009;24(Suppl1):13.
140 Fegan WG. Continuing uninterrupted compression technique of injecting varicose veins. Proc R Soc Med. 1960;53:837.
141 Fegan WG. Continuous compression technique of injecting varicose veins. Lancet. 1963;282:109.
142 Goldman MP. How to utilize compression after sclerotherapy. Dermatol Surg. 2002;28:860.
143 Reid RG, Rothnie NG. Treatment of varicose veins by compression sclerotherapy. Br J Surg. 1968;55:889.
144 Orbach EJ. A new approach to the sclerotherapy of varicose veins. Angiology. 1950;1:302.
145 Wenner L. Sind endovariköse hämatische Ansammlungen eine Normalerscheinung bei Sklerotherapie? Vasa. 1981;10:174.
146 Goldman MP, Kaplan RP, Oki LN, et al. Sclerosing agents in the treatment of telangiectasia: comparison of the clinical and histologic effects of intravascular polidocanol, sodium tetradecyl sulfate, and hypertonic saline in the dorsal rabbit ear vein model. Arch Dermatol. 1987;123:1196.
147 Ouvry PA, Davy A. The sclerotherapy of telangiectasia. Phlébologie. 1982;35:349.
148 Goldman MP, Bennett RG. Treatment of telangiectasia: a review. J Am Acad Dermatol. 1987;17:167.
149 Goldman MP, Kaplan RP, Duffy DM. Postsclerotherapy hyperpigmentation: a histologic evaluation. J Dermatol Surg Oncol. 1987;13:547.
150 Struckmann J, Christensen SJ, Lendorf A, Mathiesen F. Venous muscle pump improvement by low compression elastic stockings. Phlebology. 1986;1:97.
151 Raj TB, Goddard M, Makin GS. How long do compression bandages maintain their pressure during ambulatory treatment of varicose veins? Br J Surg. 1980;67:122.
152 Smith SL, Belmont JM, Casparian JM. Analysis of pressure achieved by various materials used for pressure dressings. Dermatol Surg. 1999;25:931.
153 Coleridge-Smith PD, Scurr JH, Robinson KP. Optimum methods of limb compression following varicose vein surgery. Phlebology. 1987;2:165.
154 Hirai M, Maki A, Yamamoto K. Compression pads in sclerotherapy for leg varicose veins. J Jpn Coll Angiol. 1996;36:305.
155 Stanley PRW, Brickerton DR, Campbell WB. Injection sclerotherapy for varicose veins – a comparison of materials for applying local compression. Phlebology. 1990;6:37.
156 Tazelaar DJ, Neumann HAM, Roos de KP. Long cotton wool rolls as compression enhancers in macrosclerotherapy for varicose veins. Dermatol Surg. 1999;25:38.
157 Partsch B, Partsch H. Which pressure do we need to compress the great saphenous vein on the thigh? Dermatol Surg. 2008;34:1726.
158 Nootheti PK, Cadag KM, Magpantay A. Goldman MP Efficacy of graduated compression stockings for an additional 3 weeks after sclerotherapy treatment of reticular and telangiectatic leg veins. Dermatol Surg. 2009;35:53.
159 Hobbs JT. Surgery and sclerotherapy in the treatment of varicose veins. Arch Surg. 1974;109:793.
160 Doran FSA, White M. A clinical trial designed to discover if the primary treatment of varicose veins should be by Fegan’s method or by an operation. Br J Surg. 1975;62:72.
161 Fegan WG. Varicose veins: compression sclerotherapy. London: Heinemann; 1967.
162 Batch AJ, Wickremesinghe SS, Gannon ME, Dormandy JA. Randomized trial of bandaging after sclerotherapy for varicose veins. Br Med J. 1980;281:423.
163 Rodrigus I, Bleyn J. For how long do we have to advise elastic support after varicose vein surgery? A prospective randomized study. Phlebology. 1991;6:95.
164 Fraser IA, Perry EP, Hatton M, Watkin DF. Prolonged bandaging is not required following sclerotherapy of varicose veins. Br J Surg. 1985;72:488.
165 Shepard JT. Reflex control of the venous system. In: Bergan JJ, Yao JST, editors. Venous problems. Chicago: Year Book, 1978.
166 Nabatoff RA. Vulvar varicose veins during pregnancy: new support for effective compression. JAMA. 1960;173:1932.
167 Ninia JG. Treatment of vulvar varicosities by injection compression sclerotherapy. Dermatol Surg. 1997;23:573.
168 Partsch H, Baccaglini U, Stemmer R. Questionnaire regarding the practice of sclerotherapy. Phlebology. 1997;12:43.
169 Hamel-Desnos CM, Guias BJ, Desnos PR, Mesgard A. Foam sclerotherapy of the saphenous veins: randomised controlled trial with or without compression. Eur J Vasc Endovasc Surg. 2010;39:500.
170 Kern P, Ramelet AA, Wütschert R, Hayoz D. Compression after sclerotherapy for telangiectasias and reticular leg veins: a randomized controlled study. J Vasc Surg. 2007;45:1212.
171 Duffy DM. Small vessel sclerotherapy: an overview. In: Callen JP, et al, editors. Advances in dermatology, vol. 3. Chicago: Year Book; 1988.
172 Bean WB. Vascular spiders and related lesions of the skin. Springfield: Thomas; 1958.
173 Bodian EL. Techniques of sclerotherapy for sunburst venous blemishes. J Dermatol Surg Oncol. 1985;11:696.
174 De Faria JL, Moraes IN. Histopathology of telangiectasias associated with varicose veins. Dermatologica. 1963;127:321.
175 Allan JC. The micro-circulation of the skin of the normal leg, in varicose veins and in the postthrombotic syndrome. S Afr J Surg. 1972;10:29.
176 Staubesand J, Seydewitz V. An ultrastructural study of sclerosed veins. Phlebologie. 1991;44:16.
177 Goldman MP, Beaudoing D, Marley W, et al. Compression in the treatment of leg telangiectasia. J Dermatol Surg Oncol. 1990;16:322.
178 Harridge H. The treatment of primary varicose veins. Surg Clin North Am. 1960;40:191.
179 Weiss RA, Sadick NS, Goldman MP, Weiss MA. Post-sclerotherapy compression: controlled comparative study of duration of compression and its effects on clinical outcome. Dermatol Surg. 1999;25:105.
180 Scurr JH, Coleridge-Smith P, Cutting P. Varicose veins: optimum compression following sclerotherapy. Ann R Coll Surg Engl. 1985;67:109.
181 Menezes A. Compression élastique dans la chirurgie des varices primitives: réflexions auprès de 67 chirurgiens portugais. In: Raymond-Martimbeau P, Prescott R, Zummo M, editors. Phlébologie ’92. Paris: John Libbey Eurotext, 1992.
182 Rastel D, Perrin M, Guidicelli H. Résultats d’une enquête sur les techniques compressives et contensives utilisées dans le traitement chirurgical des varices. J Mal Vasc. 2004;29:27.
183 Partsch H. Evidence based compression therapy. An initiative of the International Union of Phlebology. editor. Vasa 2003;32(Suppl 63):. Electronically available http://verlag.hanshuber.com/ezm/index.php?ezm=VAS&la=d&ShowIssue=1469
184 Lugli M, Cogo A, Guerzoni S, et al. Effects of eccentric compression by a crossed-tape technique after endovenous laser ablation of the great saphenous vein: a randomized study. Phlebology. 2009;24:151.
185 Thaler E, Huch A, Zimmermann R. Compression stockings prophylaxis of emergent varicose veins in pregnancy: a prospective randomized controlled study. Swiss Medical Weekly. 2001;131:659.
186 Austrell C, Thulin I, Norgren L. The effects of long-term graduated compression treatment on venous function during pregnancy. Phlebology. 1995;10:165.
187 Weber S, Schneider KT, Bung P, et al. Effects of compression stockings on blood circulation in late pregnancy. Geburtshilfe Frauenheilkd. 1987;47:396.
188 Norgren L, Austrell C, Nilsson L. The effect of graduated compression hosiery on femoral blood flow during late pregnancy. Presented at the Sixth Annual Meeting of the American Venous Forum, Maui, February 23–25, 1994.
189 Austrell C, Nilsson L, Norgren L. Maternal and fetal haemodynamics during late pregnancy: effect of compression hosiery treatment. Phlebology. 1993;8:155.
190 Krijnen RM, de Boer EM, Ader HJ, Bruynzeel DP. Venous insufficiency in male workers with a standing profession. Part 2: Diurnal volume changes of the lower legs. Dermatology. 1997;194:121.
191 Jonker MJ, deBoer EM, Adèr HJ, Bezemer PD. The oedema-protective effect of Lycra support stockings. Dermatology. 2001;203:294.
192 Jungbeck C, Peterson K, Danielsson G, Norgren L. Effects of compression hosiery in female workers with a standing profession. Phlebology. 2002;16:117.
193 Landgraf H, Vanselow B, Schulte-Huermann D, et al. Economy class syndrome: rheology, fluid balance, and lower leg edema during a simulated 12-hour long distance flight. Aviat Space Environ Med. 1994;65:930.
194 Schobersberger W, Mittermayer M, Innerhofer P, et al. Coagulation changes and edema formation during long-distance bus travel. Blood Coagul Fibrinolysis. 2004;15:419.
195 Mittermayr M, Fries D, Innerhofer P, et al. Formation of edema and fluid shifts during a long-haul flight. J Travel Med. 2003;10:334.
196 Iwama H, Furuta S, Ohmizo H. Graduated compression stocking manages to prevent economy class syndrome. Am J Emerg Med. 2002;20:378.
197 Scurr JH, Machin SJ, Bailey-King S, et al. Frequency and prevention of symptomless deep-vein thrombosis in long-haul flights: a randomised trial. Lancet. 2001;357:1485.
198 Partsch H. Intermittent pneumatic compression in immobile patients. Int Wound J. 2008;5:389.
199 Amaragiri SV, Lees TA. Elastic compression stockings for prevention of deep vein thrombosis (Cochrane Review). Cochrane Database Syst Rev 2000;(3):CD001484.
200 Kakkos SK, Caprini JA, Geroulakos G, et al. Combined intermittent pneumatic leg compression and pharmacological prophylaxis of venous thromboembolism in high risk patients. Cochrane Database Syst Rev 2008 Oct 8;(4):CD005258.
201 Morris RJ, Woodcock JP. Evidence-based compression: prevention of stasis and deep vein thrombosis. Ann Surg. 2004;239:162.
202 Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease. American College of Chest Physicians evidence-based clinical practice guidelines, 8th edn. Chest. 2008;133:454S.
203 Brandjes DPM, Büller H, Hejboer H, et al. Incidence of the postthrombotic syndrome and the effects of compression stockings in patients with proximal venous thrombosis. Lancet. 1997;349:759.
204 Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249.
205 Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105.
206 Kolbach DN, Sandbrink MWC, Hamulyak K, et al. Non-pharmaceutical measures for prevention of post-thrombotic syndrome (Cochrane Review). Issue 2. The Cochrane Library. John Wiley, Chichester, UK, 2004..
207 Kahn SR, Azoulay L, Hirsch A, et al. Effect of graduated elastic compression stockings on leg symptoms and signs during exercise in patients with deep venous thrombosis: a randomized cross-over trial. J Thromb Haemost. 2003;1:494.
208 Partsch H, Blättler W. Compression and walking versus bed rest in the treatment of proximal deep venous thrombosis with low molecular weight heparin. J Vasc Surg. 2000;32:861.
209 Blättler W, Partsch H. Leg compression and ambulation is better than bed rest for treatment of acute deep venous thrombosis. Int Angiol. 2003;22:393.
210 Partsch H. Therapy of deep vein thrombosis with low molecular weight heparin, leg compression and immediate ambulation. Vasa. 2001;30:195.
211 Kolbach DN, Sandbrink MWC, Neumann HAM, Prins MH. Compression therapy for treating stage I and II (Widmer) post-thrombotic syndrome (Cochrane Review). Issue 2. The Cochrane Library. John Wiley, Chichester, UK, 2004..
212 Mani R, Vowden K, Nelson EA. Intermittent pneumatic compression for treating venous leg ulcers (Cochrane Review). Issue 3. The Cochrane Library. John Wiley, Chichester, UK, 2004..
213 Phillips TJ, Machado F, Trout R, et al. Prognostic indicators in venous ulcers. J Am Acad Dermatol. 2000;43:627.
214 Hendricks WM, Swallow RT, Asheboro BA. Management of stasis leg ulcers with Unna’s boots versus elastic support stockings. J Am Acad Dermatol. 1985;12:90.
215 Koksal C, Bozkurt AK. Combination of hydrocolloid dressings and medical compression stockings versus Unna’s boot for the treatment of venous leg ulcers. Swiss Med Weekly. 2003;133:364.
216 Jünger M, Wollina U, Kohnen R, Rabe E. Efficacy and tolerability of an ulcer compression stocking for therapy of chronic venous ulcer compared with a below-knee compression bandage: results from a prospective, randomized, multicentre trial. Curr Med Res Opin. 2004;20:1613.
217 Jünger M, Hafner HM. Interface pressure under a ready made compression stocking developed for the treatment of venous ulcers over a period of six weeks. Vasa. 2003;32:87.
218 Amsler F, Willenberg T, Blättler W. In search of optimal compression therapy for venous leg ulcers: a meta-analysis of studies comparing divers bandages with specifically designed stockings. J Vasc Surg. 2009;50:668.
219 Jünger M, Partsch H, Ramelet AA, Zuccarelli F. Efficacy of a ready made tubular compression device versus short-stretch compression bandages in the treatment of venous leg ulcers. Wounds. 2004;16:313.
220 Milic DJ, Zivic SS, Bogdanovic DC, Perisic ZD, et al. A randomized trial of the Tubulcus multilayer bandaging system in the treatment of extensive venous ulcers. J Vasc Surg. 2007;46:750.
221 Nelson EA, Bell-Syer SE, Cullum NA. Compression for preventing recurrence of venous ulcers (Cochrane Review). Cochrane Database Syst Rev 2000;(4):CD002303.
222 Nelson EA, Harper DR, Prescott RJ, et al. Prevention of recurrence of venous ulceration: randomized controlled trial of class 2 and class 3 elastic compression. J Vasc Surg. 2006;44:803.
223 Korn P, Patel ST, Heller JA, et al. Why insurers should reimburse for compression stockings in patients with chronic venous stasis. J Vasc Surg. 2002;35:950.
224 Badger CM, Peacock JL, Mortimer PS. A randomized, controlled, parallel-group clinical trial comparing multilayer bandaging followed by hosiery versus hosiery alone in the treatment of patients with lymphedema of the limb. Cancer. 2000;88:2832.
225 Mason M. Bandaging and subsequent elastic hosiery is more effective than elastic hosiery alone in reducing lymphoedema. Aust J Physiother. 2001;47:153.