Chapter 23 Urticaria and angioedema
1. What percentage of the population experiences acute urticaria during their lifetime?
2. How is acute versus chronic urticaria defined?
Classification of urticaria begins with duration and frequency of the rash. Although arbitrary, 6 weeks of nearly daily symptoms has been chosen as the dividing point for differentiating between acute and chronic urticaria.
Ormerod AD: Urticaria: recognition, causes, and treatment, Drugs 48:717–730, 1994.
4. Are all urticarial reactions from medications allergic (IgE-mediated) in nature?
No. Some medication reactions may not be truly allergic but may be caused by nonspecific mast cell–releasing or anaphylactoid properties. Common drugs with this mechanism of action include opiates, vancomycin, radiocontrast media (especially, high-osmolar, ionic forms), and nonsteroidal antiinflammatory drugs.
7. How common are the physical urticarias?
Of 554 patients with urticaria seen in a university clinic in England, physical urticarias constituted 17.5% of the total; most of the remainder were idiopathic. The most frequent of the physical urticarias were dermographism (8.5%) (Fig. 23-2), cholinergic urticaria (5.1%), and acquired cold urticaria (2.5%).
8. What association has been described between autoantibodies and chronic urticaria?
In two studies, antithyroid microsomal antibodies have been reported in 12% to 14% of patients with chronic urticaria; however, thyroid status did not relate to the occurrence of urticaria and typically hives did not revert when a euthyroid state was achieved. A number of patients with chronic urticaria react to intradermal injection of their own serum by developing a wheal and flare that persists up to 8 hours. Many of these patients have IgG antibodies in their serum that react with the alpha subunit of the high-affinity IgE receptor on mast cells and basophils. In other patients, the IgG antibody appears to react with IgE itself. The frequency of these IgG autoantibodies in patients with chronic urticaria is not yet established but has been reported to be as high as 40% and 10%, respectively, in a referral clinic.
Tong LJ, Balakrishnan G, Kochan JP, et al: Assessment of autoimmunity in patients with chronic urticaria, J Allergy Clin Immunol 99:461–465, 1997.
9. What is the “triple response”? Name the components.
10. What is the mechanism of the axon reflex?
The axon reflex is produced by stimulation of cutaneous sensory nerve endings, with antidromic conduction of the impulse and release of the neurokinin substance P. Substance P is a vasodilator and it also causes the release of histamine and other mediators from cutaneous mast cells, thus augmenting the urticarial reaction.
11. List five mediators that are capable of directly causing vasodilatation and increased vascular permeability in the skin.
12. Name three mediators that may cause vasodilatation and increased vascular permeability indirectly through action on the mast cell.
16. How quickly after the application of cold does whealing develop in acquired cold urticaria?
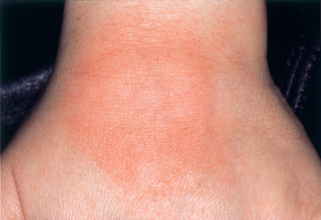
Whealing in cold urticaria does not develop during the exposure to the cold stimulus, but, rather, two minutes after rewarming, and a large hive appears by ten minutes (Fig. 23-3). The delay is probably due to the decrease in cutaneous blood flow during exposure to the cold.
17. Only one form of urticaria has whealing that is sufficiently characteristic to suggest a specific diagnosis. Which one?
The initial wheals in cholinergic urticaria are quite different from those in other forms of urticaria. They are small, punctate monomorphic (often referred to as pencil-eraser–sized, ∼0.5-cm diameter) with a prominent erythematous flare. Over time, they may become confluent, and form larger areas of whealing.
19. What are the precipitating events for cholinergic urticaria? By what mechanism do they produce the whealing?
20. How are the solar urticarias classified?


Figure 23-3. Positive ice cube test in a patient with acquired cold urticaria.
(Courtesy of James E. Fitzpatrick, MD.)
Key Points: Urticaria and Angioedema
1. Acute urticaria is usually from a secondary cause such as an allergic reaction to food, drugs, insect stings, or infection.
2. Chronic urticaria is most often idiopathic and not due to an allergic etiology but has an autoimmune basis in up to 50% of cases.
3. The most common physical urticaria is dermographism, but in chronic urticaria, screen for physical stimuli such as pressure, cold, and heat.
21. What is Darier’s sign?
Darier’s sign is a finding in urticaria pigmentosa. In urticaria pigmentosa, yellow-tan to red-brown macules containing increased numbers of mast cells are scattered over the body. Stroking the skin over the pigmented macules causes an urticarial wheal to form that is limited to the area of the pigmented lesion (Fig. 23-5).
22. How often does aspirin cause or exacerbate urticaria?
Aspirin is rarely a cause of urticaria in an otherwise asymptomatic patient, but many patients with chronic urticaria will have increased whealing if they take aspirin or nonsteroidal antiinflammatory drugs when their disease is active. These same patients are usually able to take aspirin with a much lower risk when their urticaria is inactive, indicating that aspirin is not the cause but a nonspecific exacerbating factor, presumably acting on a pharmacologic basis. Prospective and retrospective data suggest that aspirin administration will cause a flare in 20% to 40% of patients with active urticaria.
Moore-Robinson M, Warin RP: Effect of salicylates in urticaria, BMJ 4:262–264, 1967.
23. What is the prognosis of chronic urticaria?
Champion followed 554 patients with urticaria seen at a hospital clinic in England. After 6 months, 50% still had active disease. Of these patients, 40% continued to have at least intermittent symptoms 10 years later. The prognosis was somewhat worse in patients with only angioedema and even poorer if both urticaria and angioedema were present.
24. Much has been discovered in recent years regarding the histopathology of chronic idiopathic urticaria. What three major types of cells may be encountered in increased numbers in these biopsies?
The characteristic histopathologic finding of nonvasculitic chronic urticaria is a subtle to modest perivascular and interstitial infiltrate. There are increased numbers of lymphocytes. Mast cells are increased some 10-fold, while there is a fourfold increase in mononuclear cells. There is increased histamine in blisters suctioned from chronic urticaria patients. Although eosinophils are often not prominent, increased deposition of the major basic protein of the eosinophil is present in the tissue in 50% of patients, indicating eosinophil involvement in the inflammatory process, although only a fraction of these had evidence of eosinophilic accumulation.
25. In contrast to chronic idiopathic urticaria, what are the typical histologic features of urticarial vasculitis?
Biopsy specimens from patients with urticarial vasculitis typically reveal necrotizing vasculitis of the small venules with deposition of immunoglobulin and complement. In those with low serum complement (hypocomplementemic urticarial vasculitis), polymorphonuclear leukocytes commonly predominate, while in those with normal serum complement, a lymphocytic infiltrate is more typical.
26. Can clinical findings suggest the presence of urticarial vasculitis?
The individual lesions of vasculitis may resemble those of idiopathic urticaria; however, they may feel firmer, tend to persist for greater than 24 hours, and, on clearing, they tend to leave an ecchymotic area due to leakage of red blood cells into the perivascular tissue (Fig. 23-6). Associated systemic symptoms, such as arthralgias and myalgias, are also common. The erythrocyte sedimentation rate is often increased, autoantibodies may be present, and there may be evidence of renal disease.
27. A number of clues in the patient’s history may suggest that a patient with recurrent angioedema has the hereditary form. Name some.
Between 75% and 85% of patients with hereditary angioedema (HAE) give a positive family history of similar attacks. The attacks of angioedema themselves are characterized by absence of urticaria and pruritus, both common with idiopathic angioedema. In HAE, episodes of angioedema are often triggered by trauma such as surgery. However, such a triggering event may not be evident. Significant upper airway obstruction is seen almost exclusively in HAE, as opposed to ordinary idiopathic angioedema. Attacks of severe abdominal pain are common in HAE, representing edema of the bowel wall. Finally, attacks of HAE typically progress for several days and respond poorly to treatment with antihistamines or epinephrine.
29. Name the recommended screening laboratory test for hereditary angioedema.
Serum C4. C2 is usually within normal limits when the patient is between attacks. In 80% of individuals with HAE, the C1 esterase inhibitor is low; however, the enzyme level can be normal but nonfunctional in 15% to 20% of patients. The normal immunoassay will not detect these patients; a functional assay is required but is usually not readily available and is more expensive than a determination of C4 level.
30. What is the treatment of choice for HAE? How does it work?
HAE is inherited in an autosomal dominant pattern. Attenuated androgens, such as danazol, induce synthesis of normal C1 esterase inhibitor by the liver in these patients. Patients with the functionally abnormal C1 esterase inhibitor also respond, since they too have one normal gene. Pooled C1 inhibitor (prophylaxis) and kallikrien inhibitors for acute attacks are available.
32. A 60-year-old patient presents with a new onset of attacks of nonpruritic angioedema and a depressed C4 level. What is the first diagnosis you consider?
Acquired C1 esterase inhibitor deficiency. This situation is usually encountered in patients with lymphoma who have a circulating low-molecular-weight IgM, decreased C1 esterase inhibitor level, and low levels of the C1–C4. The mechanism of C1 activation is by reaction with immune complexes or by binding of the C1 to antiidiotypic antibody bound to the immunoglobulin on the surface of the tumor cells. Acquired C1 esterase deficiency has also been reported with connective tissue disorders such as systemic lupus erythematosus, with carcinoma, and with an IgG antibody directed toward C1 esterase inhibitor. In the latter circumstance, the C1 levels are usually normal. Androgen therapy benefits patients with acquired C1 esterase inhibitor deficiency by increasing C1 esterase inhibitor production by the liver.
33. Certain drugs have been identified as being particularly effective for a subset of patients with chronic urticaria or angioedema. What are these drugs, and when is a trial with them indicated?
• Cyproheptadine has been reported to be particularly effective in controlling acquired cold urticaria.
• Corticosteroids and nonsteroidal antiinflammatory drugs prevent the lesions of delayed pressure urticaria, whereas antihistamines are completely without benefit.
34. What three mediator antagonists have been reported to be useful in symptomatic control of urticaria?
Competitive antagonists of the H1 and H2 histamine receptor and antagonists of leukotriene D4 receptor have been reported to be useful in treating urticaria. The latter two are usually used in conjunction with an H1 antagonist. Recent studies suggest that the nonsedating H1 antagonists are just as effective in treating urticaria as the classic, sedating antagonists.