197 Urticaria
Salient features
History
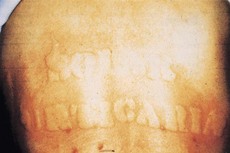
• Determine physical causes that could have precipitated this response: cold urticaria, dermatographism (Fig. 197.1), pressure, sunlight, exercise, hot shower
• Drug history: aspirin, NSAIDs, morphine, codeine, penicillin, sulphonamides
• Whether any foods precipitate the rash such as strawberries, seafood, nuts, chocolate
• Blood products causing these lesions.
• Viral infections and febrile illnesses
Diagnosis
• SLE and Sjögren’s sydrome may present with urticarial lesions, which are usually urticarial vasculitis.
• Chronic urticaria is the occurrence of daily or almost daily widespread itchy wheals for at least six weeks (N Engl J Med 1995;332:1767–72). This includes urticarial vaculitis and physical urticaria.
Advanced-level questions
How would you investigate a patient with chronic urticaria?
• FBC and white count; if eosinophilia is present
• Examination of the stool for ova and parasites
• Physical urticaria must be assessed by appropriate challenge testing
• Peanut-specific Ig-E when peanut allergy is suspected
• Serum complement C4 when there is a history of repeated cutaneous or mucosal angioedema
• Thyroid function tests because of diagnostic overlap between chronic urticaria and thyroid disease. The percentage of patients with chronic urticaria who have antithyroglobulin antibody, antimicrosomal antibody or both is 27%; 19% have abnormal thyroid function.
How would you manage patients with chronic urticaria?
• Identify avoidable cause such as food additives. Challenge testing for food additives should be avoided in patients with a history of severe angioedema, asthma or episodes of anaphylaxis.
• Antihistamines: about 85% of cutaneous histamine receptors are of the H1 subtype, and the remaining 15% are H2 receptors. The addition of an H2-receptor antagonist to an H1-receptor antagonist augments the inhibition of a histamine-induced wheal-and-flare reaction once H1-receptor blockade has been maximized. H1 antihistamines (terfenadine, doxepin) with a low potential for sedation are first-line treatment; 2% ephedrine spray is useful for oropharyngeal oedema. Non-sedating antihistamines such as loratadine, fexofenadine and cetirizine alleviate pruritus and decrease the incidence of hives.
• Leukotriene antagonists (zafirlukast and montelukast) have been shown to be superior to placebo.
• Calcium channel blockers can be used.
• A tepid shower temporarily alleviates itching.
• Corticosteroids merits consideration in patients who have little response to even a combination of H1-receptor blockers, H2-receptor blockers, and leukotriene-receptor blockade.
• Ciclosporin is the best studied immunosuppressive therapy for chronic urticaria.
• All patients should be advised to avoid aspirin and other NSAIDs, ACE inhibitors, macrolide antibiotics and imidazole antifungal agents.