CHAPTER 16 Urology
Congenital disorders of the urinary tract
Kidney and ureter
Haematuria
Haematuria is the passage of red blood cells in the urine. This may vary from a few red cells detected on ‘stix’ testing to the passage of frank blood. Haematuria may be noted at the beginning of micturition, throughout micturition or at the end of micturition. Care must be taken to avoid menstrual bleeding being mistaken for haematuria. Other causes of red urine include excessive beetroot ingestion, rifampicin, porphyria, haemoglobinuria and myoglobinuria. (For causes of haematuria → Table 16.1.)
| Kidney | Glomerular disease |
| Polycystic kidneys | |
| Carcinoma | |
| Stone | |
| Trauma (including renal biopsy) | |
| Tuberculosis | |
| Embolism | |
| Renal vein thrombosis | |
| Vascular malformation | |
| Ureter | Stone |
| Neoplasm | |
| Bladder | Carcinoma |
| Stone | |
| Trauma | |
| Inflammatory – cystitis, tuberculosis, bilharzia | |
| Prostate | Benign prostatic hypertrophy |
| Neoplasm | |
| Urethra | Trauma |
| Stone | |
| Urethritis | |
| Neoplasm | |
| General | Anticoagulants |
| Thrombocytopenia | |
| Haemophilia | |
| Sickle cell disease | |
| Malaria |
Obstructive uropathy
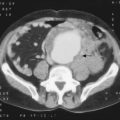
Hydronephrosis is the distension of the calyces and pelvis of the kidney owing to obstruction to the outflow of urine. It may be bilateral or unilateral. (For causes of hydronephrosis → Table 16.2.)
| Unilateral | Pelviureteric junction obstruction
Ureteric obstruction |
Investigations
Calculous disease
Types of calculi
Investigations
Emergency for severe renal pain or ureteric colic:
Following acute attack or routine for urinary symptoms or incidental finding of stone:
Treatment
Acute symptoms – ureteric colic:
Tumours of the renal tract
Bladder
Treatment of transitional cell carcinoma
Urinary tract infections (UTIs)
Urinary tract tuberculosis
Investigation
Prostate
Urinary retention
The retention of urine may be acute, chronic or acute-on-chronic. Patients with acute retention present as surgical emergencies. (For causes of urinary retention → Table 16.3.)
| Local | |
| Urethral lumen or bladder neck | Urethral valves |
| Tumours | |
| Stones | |
| Blood clot | |
| Meatal ulcer or stenosis | |
| Urethral or bladder wall | Urethral trauma |
| Urethral stricture | |
| Urethral tumour | |
| Outside the wall | Prostatic enlargement |
| Faecal impaction | |
| Pelvic tumour | |
| Pregnant uterus | |
| Phimosis | |
| General | |
| Postoperative | |
| Neurogenic | Spinal cord injuries |
| Spinal cord disease, e.g. tabes dorsalis, spinal tumour, multiple sclerosis, diabetic autonomic neuropathy | |
| Drugs | Anticholinergics, antidepressants, alcohol |
Testes and epididymis
Varicocele
These are varicosities of the pampiniform plexus. More common on the left side.
Penis
Conditions of the foreskin
Circumcision
| Religious |
| Phimosis |
| Paraphimosis |
| Recurrent balanoposthitis |
| Diagnosis of underlying penile tumours |
| Trauma and tumour of foreskin |