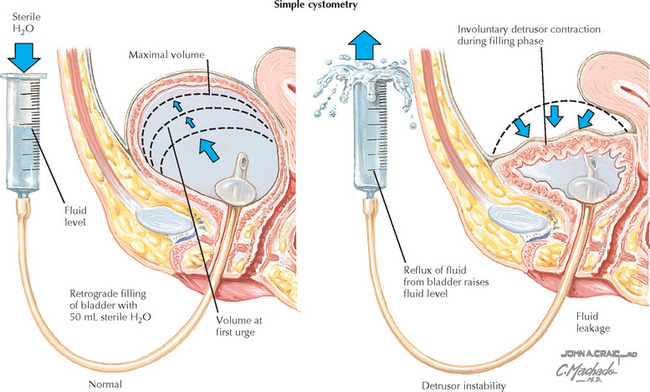
Chapter 253 Urodynamic Testing: Simple
REQUIRED EQUIPMENT
Sutherst JR, Brown MC. Comparison of single and multichannel cystometry in diagnosing bladder instability. Br Med J (Clin Res Ed). 1984;288:1720.
Thorp JM, Jones LH, Wells E, Ananth CV. Assessment of pelvic floor function: a series of simple tests in nulliparous women. Intl Urogynecol J. 1996;7:94.
Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardization of terminology of lower urinary tract function produced by the International Continence Society Committee on Standardization of Terminology. Scand J Urol Nephrol. 1988;114:5.
American College of Obstetricians and Gynecologists. Urinary incontinence in women. Obstet Gynecol. 2005;105:1533.
American College of Obstetricians and Gynecologists. Antibiotic prophylaxis for gynecologic procedures. ACOG Practice Bulletin 74. Obstet Gynecol. 2006;108:225.
Consensus Conference. Urinary incontinence in adults. JAMA. 1989;261:2685.
Lentz GM. Urogynecology. In: Katz VL, Lentz GM, Lobo RA, Gershenson DM, editors. Comprehensive Gynecology. 5th ed. Philadelphia: Mosby/Elsevier; 2007:545.
Massey A, Abrams P. Urodynamic of the female lower urinary tract. Urol Clin North Am. 1985;12:231.
Ouslander J, Leach G, Staskin D, et al. Prospective evaluation of an assessment strategy for geriatric urinary incontinence. J Am Geriatr Soc. 1989;37:715.
Ouslander JG. Diagnostic evaluation of geriatric urinary incontinence. Clin Geriatr Med. 1986;2:715.
Ouslander JG, Leach GE, Staskin DR. Simplified tests of lower urinary tract function in the evaluation of geriatric urinary incontinence. J Am Geriatr Soc. 1989;37:706.