Upper Respiratory Tract Infections
Pharyngitis (Tonsillopharyngitis)
Etiology
Viruses are responsible for most cases of pharyngitis in both children and adults. Group A beta-hemolytic Streptococcus (GABHS) is the most common bacterial cause of pharyngitis in children, with a peak incidence of 30%. As in adults, non–group A streptococci, Mycoplasma pneumoniae, and Chlamydia pneumoniae infections are on the rise in pediatric populations.1–4 In adults, sexually transmitted diseases should be considered, as well.1–8 Whereas immunization has led to a decline in diphtheria as a cause of pharyngitis, it can result in serious complications and needs to remain in any differential diagnosis.
Mixed aerobic and anaerobic bacteria often cause chronic or recurrent pharyngitis, especially those that produce β-lactamase. Epstein-Barr virus (EBV) and Actinomyces are also implicated in chronic or recurrent pharyngitis. Rare causes of bacterial pharyngitis include Francisella tularensis, Yersinia pestis, and Yersinia enterocolitica.1,2,5
Clinical Features
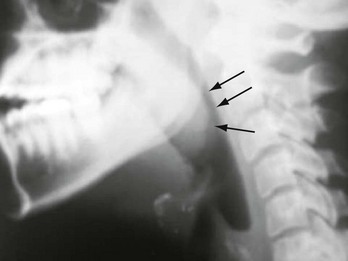
The most common symptom is pharyngeal pain that is aggravated by swallowing and may radiate to the ears. Examination usually reveals fever, pharyngeal erythema, pharyngeal or tonsillar exudate, and tonsillar enlargement (Fig. 75-1). The infection tends to localize to lymphatic tissue and produces suppuration and swelling of the tonsils, along with tender cervical adenopathy. Occlusion of the eustachian tubes may result in secondary otitis media. Clinical differentiation of the causative organisms is virtually impossible.1,2,5–7

Figure 75-1 Bilateral tonsillopharyngitis.
Viral pharyngitis usually occurs in conjunction with cough, rhinorrhea, myalgia, headache, stomatitis, conjunctivitis, exanthem, and odynophagia. Low-grade fever and pharyngeal exudates may be present. Cervical lymphadenopathy is generally absent.1,2 Mild pharyngeal edema and erythema associated with a “scratchy” throat are present in 50% of patients with the common cold. Systemic viral infections, including measles, cytomegalovirus (CMV), rubella, and human immunodeficiency virus (HIV), may initially manifest as mild pharyngitis.1,2,5 HIV and CMV pharyngitis may be clinically indistinguishable from infectious mononucleosis.1,2
Influenza occurs in epidemics and is associated with high fever, myalgia, and headache. Although 50 to 80% of patients with influenza experience pharyngeal discomfort, pharyngeal exudate and cervical lymphadenopathy are rare. Adenovirus may cause severe exudative pharyngitis with cervical adenitis similar to that in streptococcal pharyngitis. Thirty percent to 50% of cases of adenoviral pharyngitis are associated with a follicular, usually unilateral, conjunctivitis, and preauricular lymphadenopathy. Coxsackieviruses are the most frequent causes of hand-foot-and-mouth disease and herpangina.1,2
Pharyngitis is a common manifestation of infectious mononucleosis (caused by EBV) in young adults.1,2,5 Symptoms develop after an incubation period of 4 to 7 weeks. Fever and a tonsillar exudate or a membrane (that is cheesy or creamy white) is often present. Cervical as well as generalized lymphadenopathy (90-100%) and splenomegaly (50%) are usually noted, and palatal petechiae may be present. Hepatomegaly is present in 10 to 15% of cases. Periorbital edema and rash are rare findings. In up to 90% of patients with mononucleosis who are given ampicillin or amoxicillin, a diffuse macular rash develops that may be misdiagnosed as an allergic reaction.1,2
Patients with early (days to weeks) HIV infection can develop an acute retroviral syndrome. This is manifested by fever, sore throat, generalized nontender lymphadenopathy, a diffuse maculopapular rash, arthralgias, mucocutaneous ulcerations, and, commonly, diarrhea. Nonexudative pharyngitis is present in 50 to 70% of patients. Oral thrush and ulcers may be present. Acute HIV infection can be differentiated from infectious mononucleosis by a more acute presentation, the absence of tonsillar hypertrophy or exudates, the frequent occurrence of rash, and the presence of oral ulcerations.1
Herpes simplex infections, which typically affect young adults, also cause pharyngitis and are signaled by the presence of painful vesicles with erythematous bases. Ulcers may be present on the pharynx, lips, tongue, gums, and buccal mucosa. Pharyngeal erythema and exudate, fever, and tender lymphadenopathy are common for 1 to 2 weeks. In an immunocompromised host, large painful ulcers may be present. Herpes pharyngitis can be caused by primary infection or reactivation. Concomitant bacterial superinfection may occur.1,2
GABHS pharyngitis is primarily a disease of children 5 to 15 years old and, in temperate climates, occurs in winter and early spring.1,2 It is responsible for less than 15% of cases of pharyngitis in patients older than 15 years and is rare in patients younger than 3 years. In epidemics, the incidence may double.1,2 GABHS pharyngitis is associated with sudden-onset sore throat, temperature over 38.3° C (101° F), tonsillar erythema and exudates, palatal and uvular petechiae, uvular edema and erythema, and tender anterior cervical lymphadenopathy. Headache, nausea, vomiting, and abdominal pain may be present, especially in children. Cough, rhinorrhea, coryza, and other viral symptoms are usually absent. GABHS pharyngitis associated with a fine sandpaper erythematous rash that subsequently desquamates is termed scarlet fever. These findings, however, cannot be used to reliably diagnose or exclude streptococcal pharyngitis. Patients with recent exposure to others at risk for GABHS pharyngitis or in whom it has been diagnosed are more likely to become infected.1,2,5–7 Non-GABHS species can cause pharyngitis indistinguishable from GABHS.1
Diphtheria is a potentially lethal cause of pharyngitis that is uncommon where adequate vaccinations are administered. U.S. serologic surveys indicate that a large percentage of adults and adolescents lack immunity to diphtheria toxin.1 After a 2- to 4-day incubation period, patients develop malaise, sore throat, fever, and dysphagia. Examination early in the disease process may reveal pharyngeal erythema and isolated spots of gray or white exudate that later coalesce to form a pseudomembrane. This gray-green pseudomembrane is usually well demarcated and covers the nares, tonsils, soft palate, pharyngeal mucosa, and occasionally the uvula. The membrane may extend to involve the larynx and tracheobronchial tree, leading to hoarseness, cough, stridor, and airway obstruction. Painful cervical lymphadenopathy may be found. Severe inflammation and edema can produce dysphonia and a characteristic “bull neck” appearance. Some strains of Corynebacterium diphtheriae produce a systemic toxin that may cause myocarditis, polyneuritis (at first autonomic and then peripheral), vascular collapse, diffuse focal organ necrosis, and death. Asymptomatic carriers may transmit the disease.1,2 Corynebacterium ulcerans is an animal pathogen passed on by consumption of raw milk that can produce infection indistinguishable from that caused by C. diphtheriae.
Arcanobacterium haemolyticum typically affects the 10- to 30-year-old age group and can be indistinguishable from streptococcal pharyngitis. Most patients have an associated rash that may be scarlatiniform, urticarial, or erythema multiforme (occasionally, skin manifestations may be the only complaint). Patients report a moderately severe sore throat and are usually nontoxic and afebrile. A. haemolyticum may cause a membranous pharyngitis that strongly mimics diphtheria; it is also associated with chronic tonsillitis.1,2,5
Anaerobic pharyngitis, or Vincent’s angina, is characterized by superficial ulceration and necrosis that often results in the formation of a pseudomembrane. Foul-smelling breath, odynophagia, submandibular lymphadenopathy, and exudate are often present. Patients typically have poor oral hygiene.5
Gonococcal pharyngitis is a sexually transmitted disease that may occur independently of genital infection. Those at highest risk are persons who practice receptive oral sex, especially men who have sex with men (in whom the incidence is reported to be as high as 15%). Its severity is variable, and it may result in an exudative or nonexudative pharyngitis. These differing manifestations occur after a lack of symptoms during the latent period of infection. Asymptomatic carriers are described, as is chronic and recurrent pharyngitis. Gonococcal pharyngitis is an important source of gonococcemia.1,2,5 Syphilitic pharyngitis is a manifestation of primary or late (tertiary) syphilis and manifests with painless mucosal lesions. Chlamydia trachomatis pharyngitis is a sexually transmitted disease that manifests similarly to gonococcal pharyngitis and is associated with orogenital sex. Urogenital culturing is necessary, along with treatment of sexual contacts. Patients are usually asymptomatic or may have only mild symptoms.1,2
M. pneumoniae infection usually causes a mild pharyngitis. Mycoplasma infection occurs in epidemics and in crowded conditions and can be responsible for approximately 10% of cases of adult pharyngitis. Pharyngeal and tonsillar exudates, cervical lymphadenopathy, and hoarseness are common. Lower respiratory tract infection may also be present.1,2,5
C. pneumoniae pharyngitis resembles M. pneumoniae pharyngitis. It also occurs in epidemics or crowded conditions. Severe pharyngitis with laryngitis is suggestive of C. pneumoniae infection. Swelling and pain in the deep cervical lymph nodes may be prominent. Lower respiratory tract and concomitant sinusitis occur. The hallmarks of chlamydial pharyngitis are recurrence and persistence.2,5
Diagnostic Strategies
Monospot test results may be negative in up to 10% of patients with infectious mononucleosis, especially in the early stages of the illness. Immunoglobulin M (IgM) antibodies to EBV capsid antigen develop in 100% of cases. EBV nuclear antigens develop within 3 to 6 weeks and are useful if an initially negative test result becomes positive at a later date. Peripheral blood smears demonstrate atypical mononuclear cells in 75% of patients, with the peak incidence occurring in the second to third week of illness.1,2 Herpes pharyngitis may be diagnosed by culture, cytopathologic tests on scrapings of lesions, and serologic tests. Enzyme-linked immunosorbent assay testing for HIV can be falsely negative during the first 3 to 4 weeks of illness. During this period of time, quantitative assays for plasma RNA should be performed.1
Diagnosis of GABHS infection is important to prevent complications, particularly rheumatic fever. Even the most experienced practitioner has difficulty clinically diagnosing streptococcal pharyngitis.1,2,5–7 Several authors have proposed scoring systems based on clinical findings,2,5–7 but the only valid method of determining acute GABHS infection is by use of acute and convalescent antistreptolysin O titers, which is not practical in the emergency department (ED). A single throat culture has a sensitivity of 90 to 95% in detecting Streptococcus pyogenes in the pharynx. Variables that affect the accuracy of throat cultures include collection and culturing technique, as well as the recent use of antibiotics.1,5–7
Rapid diagnostic tests for GABHS detect streptococcal antigens. Rapid streptococcal tests (RSTs) have a reported specificity and sensitivity of up to 95%. Sensitivity and specificity in actual practice are lower than in controlled trials.1 Patients with positive cultures or RSTs may actually be carriers who may not need treatment and are at low risk for transmission and complications. The use of RSTs in patients without clinical findings consistent with GABHS increases false-positive results. A positive RST result seems to reliably indicate the presence of S. pyogenes in the pharynx. In contrast, RST results are often negative in the setting of pharyngitis with a low bacterial count (these patients are still at risk for complications, including rheumatic fever). It is recommended that a negative RST result in a child be followed by a confirmatory culture.1,5–7
Diagnosis and treatment of GABHS in adults is controversial and the subject of two expert panel recommendations.5–7 Use of clinical criteria in conjunction with RSTs improves the accuracy of RSTs, adults with negative RST results do not require confirmatory cultures (because of the lower incidence of GABHS infection and the extremely low risk for complications), and neither testing nor antibiotic treatment should be used in patients who are clinically at low risk for GABHS infection. Both panels agree that the most useful clinical criteria for determining GABHS pharyngitis are the Centor criteria (Box 75-1).5–7
The position of the Infectious Diseases Society of America is that a positive throat culture or RST result, in addition to clinical symptoms and signs, is needed to confirm the diagnosis of GABHS pharyngitis. The society stresses that clinical criteria alone are appropriate to determine which patients do not need testing but are insufficient, without bacterial confirmation, to diagnose GABHS pharyngitis.1
We recommend that any patient with none or only one Centor criterion not be tested or treated; patients with all four criteria should be treated without testing. Patients with two or three criteria should undergo RSTs and should be treated only if they have positive results (Box 75-2).6,7
These recommendations apply only to immunocompetent patients with no underlying comorbid conditions or a history of rheumatic fever. They do not apply in settings of outbreaks of GABHS infection or rheumatic fever, nor are they appropriate in situations in which the endemic rate of rheumatic fever is higher than that in the United States. It is important to consider local epidemics and be prepared to revise the approach to treatment if evidence of GABHS infection or complications exists.5–7 Non–group A streptococcal pharyngitis should also be treated, because the same suppurative complications occur as with group A streptococcal pharyngitis. Pharyngitis caused by other treatable organisms should also be considered and is associated with serious complications.1,2,6 Confirmation of diphtheria requires culturing on the proper media and immunologic testing (polymerase chain reaction). Toxigenicity testing should also be performed.1,2 The diagnosis of A. haemolyticum infection should be considered if rash, including erythema multiforme, accompanies pharyngitis. The diagnosis of Vincent’s angina is based on clinical findings and Gram’s stain. In cases of possible gonococcal infection, a sample should be plated on Thayer-Martin agar. Tuberculous pharyngitis is diagnosed by acid-fast staining. Syphilitic pharyngitis is diagnosed with darkfield microscopy, direct immunofluorescence, and serologic testing. Candidal pharyngitis is diagnosed by noting yeast on potassium hydroxide preparations of throat swabs or Sabouraud’s agar.2 The diagnosis of mycoplasmal pharyngitis can be confirmed serologically or by culture. Rapid antigen tests for Mycoplasma are available. Chlamydial pharyngitis can be diagnosed by serologic testing, by culture, or by antigen detection tests. Studies of patients with chronic pharyngitis find that surface cultures do not correlate well with the causal pathogens, which are often concealed within the tonsillar crypts.
Differential Diagnosis Considerations
The differential diagnosis of adult pharyngitis includes deep space infections, tumors, foreign bodies, pemphigus, Stevens-Johnson syndrome, drug reactions, allergic reactions, uvulitis, angioneuropathic edema, chemical and thermal burns, esophagitis, gastroesophageal reflux disease, cricoarytenoid arthritis, thyroiditis, and epiglottitis.7
Management
Patients with pharyngitis should be treated symptomatically with topical anesthetic rinses or lozenges and with acetaminophen or ibuprofen. Oral hydration and saltwater gargles are helpful. Most cases of pharyngitis are self-limited and follow a benign course.1,5–7 Antibiotics are overused in the treatment of pharyngitis and are not indicated in the vast majority of cases of pharyngitis diagnosed in the United States.
Treatment of infectious mononucleosis is supportive (see Chapter 130). Patients should avoid contact sports for 6 to 8 weeks to minimize the small risk of splenic rupture. Corticosteroids are indicated for patients with tonsillar hypertrophy that threatens airway patency, severe thrombocytopenia, or hemolytic anemia.1,2 Acyclovir, valacyclovir, or famciclovir is indicated in immunocompromised patients with herpetic pharyngitis and may be beneficial in the treatment of acute herpetic pharyngitis.1,7 The use of antiretrovirals is indicated in acute HIV infection.1
GABHS pharyngitis in children and adolescents should be treated adequately (within 9 days) to prevent rheumatic fever. The incidence of rheumatic fever parallels that of GABHS and has markedly diminished with the use of antibiotics. Patients with mild cases of GABHS pharyngitis may develop rheumatic fever. Rheumatic fever complicates 0.3% of cases of GABHS pharyngitis, but in epidemics the incidence increases to 3%. More troubling is an increase in sporadic outbreaks of rheumatic fever.5–7 The incidence and course of poststreptococcal glomerulonephritis caused by nephritogenic strains are unaffected by antibiotic therapy.1,5–7 Antibiotic therapy is extremely effective in eradicating GABHS and its other complications. Untreated, GABHS pharyngitis is a self-limited illness that lasts 3 to 4 days. Early antibiotic treatment of streptococcal pharyngitis leads to a 13% earlier resolution of symptoms and shortens the course of illness by about 1 day. Antibiotic therapy also decreases transmission, and patients are no longer infectious after 24 hours of antibiotic treatment.1,5–8
The antibiotic regimen of choice for adults with GABHS pharyngitis is either a single intramuscular injection of 1.2 million units of benzathine penicillin or a 10-day course of penicillin V, 500 mg orally twice a day. Less frequent administration is less effective in preventing rheumatic fever.1,5–7 Intramuscular penicillin may be more effective than oral penicillin and ensures compliance, but allergic reactions are more severe as a result of procaine allergy, and treatment is more expensive. Penicillin failure usually reflects noncompliance, reinfection, or the presence of β-lactamase–producing organisms. Erythromycin or azithromycin is recommended for patients who are allergic to penicillin. A 1-g total daily dose of erythromycin is given for 10 days, but administration intervals of two, three, and four times a day are equally effective in preventing rheumatic fever. A 5-day course of azithromycin is recommended.1,5–7 Use of cephalosporins or clindamycin is also acceptable for penicillin-allergic patients. Once-daily amoxicillin therapy may be effective in children.1,9 Oral cephalosporins or clindamycin should be reserved for patients not responding to penicillin or unable to tolerate either penicillin or erythromycin.1,5,8,9
Patients whose symptoms return within a few weeks of treatment may have been noncompliant with oral therapy or may have acquired a new infection (at times from asymptomatic close contacts). Evaluation and treatment should be similar to that of the first episode, with consideration given to treatment with intramuscular penicillin. Further recurrences require more extensive evaluation. Pharyngeal cultures should be obtained and consideration given to evaluating and treating close contacts for GABHS infection.5
Although many studies focus on GABHS pharyngitis, proper treatment of nonstreptococcal pharyngitis can also prevent serious complications. Because clinical judgment is insufficient and rapid diagnostic tests are not always accurate and diagnose only GABHS, this disease process is often treated empirically. The choice of antibiotic for the empirical treatment of adult bacterial pharyngitis is not fully elucidated. It is unclear how effective antibiotics are in uncomplicated cases of non-GABHS pharyngitis in adults. Antibiotics may modestly shorten the course of the disease process, but they are also associated with increased recurrence, increased bacterial drug resistance, decreased immune response, and patient expectations for antibiotics with subsequent episodes of pharyngitis.1,5–8
Successful treatment of diphtheria is inversely related to the duration of disease. When diphtheria is strongly suspected on the basis of clinical findings, treatment is begun empirically. Airway collapse may occur suddenly and without warning. The mainstay of therapy is antitoxin (a horse serum product), which should be administered immediately on clinical suggestion of diphtheria. The dose of antitoxin varies widely and depends on the site of infection and the duration of symptoms. Antibiotics have little effect on the resolution of systemic toxicity, but they are useful in eradicating C. diphtheriae infection and preventing transmission. Infected patients should remain in strict isolation to prevent transmission. The antibiotic of choice is penicillin G for 5 days, followed by penicillin VK for 5 days, or erythromycin 500 mg four times a day for 10 days. A small percentage of patients require an additional 10-day course of erythromycin for persistent infection. Rifampin 600 mg/day for 10 days is also effective in eradicating the carrier state of C. diphtheriae and treating erythromycin-resistant diphtheria. Diphtheria toxoid should be administered during convalescence and to unvaccinated close contacts.1,2,10
A. haemolyticum may be resistant to penicillin. Erythromycin 250 mg orally four times a day for 10 days is the treatment of choice.1,2 Vincent’s angina is treated with penicillin or clindamycin and rinses with an oral oxidizing agent (hydrogen peroxide).10 Gonococcal pharyngitis is often more difficult to eradicate than genital infections. Treatment is similar to that for gonococcal urethritis and consists of ceftriaxone (125 mg intramuscularly) with concomitant treatment of chlamydial infection with a single oral dose of 1 g of azithromycin or a course of doxycycline 100 mg orally twice a day for 7 days.2,10 Oral fluoroquinolones are no longer recommended owing to the high prevalence of gonococcal resistance. Tuberculous pharyngitis is seen with disseminated disease. Patients should be isolated and treated with a multidrug regimen. Pharyngitis caused by primary syphilis is treated with 2.4 million units of benzathine penicillin (long acting), with 14 days of tetracycline or doxycycline used as an alternative. Candidal pharyngitis is treated with systemic fluconazole or itraconazole. Alternative therapy includes nystatin (suspension or tablets) or oral clotrimazole for 14 days. Chronic suppression therapy with ketoconazole, clotrimazole, or fluconazole is usually required for HIV pharyngitis.10
M. pneumoniae is treated with erythromycin, tetracycline, or doxycycline for 7 to 14 days.2,10 Chlamydial pharyngitis is treated with doxycycline, trimethoprim-sulfamethoxazole, or a macrolide antibiotic. C. pneumoniae pharyngitis should be treated for 7 to 10 days to prevent treatment failure and recurrence. C. trachomatis pharyngitis may require prolonged or repeated courses of antibiotics.2,10
Treatment of recurrent or chronic tonsillitis should include β-lactamase–resistant antibiotics active against aerobic and anaerobic organisms. Choices include oral cephalosporins, amoxicillin-clavulanic acid, penicillin with rifampin or metronidazole, and clindamycin.2
Steroids given in conjunction with oral antibiotics in adults with acute pharyngitis may significantly shorten the duration of symptoms and provide a greater degree of pain relief without increasing complications. Oral (40-60 mg of prednisone per day for 1-5 days) or intramuscular (a single dose of 10 mg of dexamethasone) administration is equally effective.11,12
Disposition
Although most cases of pharyngitis follow a benign course, life-threatening complications can rarely occur. Airway compromise from tonsillar enlargement, local and distant spread of infection, deep neck abscesses, necrotizing fasciitis, sleep apnea, bacteremia, sepsis, and death have been reported but are very rare, given the prevalence of these diseases.1,5
Infectious mononucleosis may lead to hepatic dysfunction, splenic injury, neurologic disorders, pneumonitis, pericarditis, and hematologic disorders, including thrombocytopenia and hemolytic anemia.1,2 Complications of GABHS pharyngitis are both suppurative and nonsuppurative. Suppurative complications include peritonsillar abscess, deep space abscesses, suppurative cervical lymphadenitis, otitis media, sinusitis, mastoiditis, bacteremia, sepsis, osteomyelitis, empyema, meningitis, and soft tissue infections. Nonsuppurative complications include scarlet fever, rheumatic fever, poststreptococcal glomerulonephritis, nonrheumatic perimyocarditis, erythema nodosum, and streptococcal toxic shock syndrome. In contrast to rheumatic fever, other complications of GABHS pharyngitis are increasing in incidence and severity. A chronic carrier state of streptococcal infection exists and can persist for several months despite treatment. Affected patients are asymptomatic, at low risk for rheumatic fever, and not considered highly contagious. Non–group A streptococcal pharyngitis may be complicated by the same suppurative complications as group A infections. Scarlet fever and acute glomerulonephritis, but not rheumatic fever, are linked to group C and G pharyngitis.1,2,5–7
Lingual Tonsillitis
Lingual tonsillitis is a rarely diagnosed cause of pharyngitis that predominantly occurs in patients who have had palatine tonsils removed. The lingual tonsils are most commonly (size and location are highly variable) located symmetrically on either side of the midline just below the inferior pole of the palatine tonsils and anterior to the vallecula at the base of the tongue. This lymphoid tissue may enlarge after puberty, repeated infection, and tonsillectomy.13 Patients with lingual tonsillitis have a sore throat that worsens with movement of the tongue (including tongue depression) and phonation. The patient may have a classic “hot potato” voice (the muffled voice one has when eating very hot food) and report feeling a swelling in the throat. Dysphagia, fever, respiratory distress, and stridor may be present. Chronic or recurrent lingual tonsillitis may also cause a chronic cough or sleep apnea. Physical findings often include a normal-appearing pharynx with mild hyperemia. Direct or indirect laryngoscopy reveals an edematous lingual tonsil covered with a purulent exudate. Lateral soft tissue neck films aid in the diagnosis. These films demonstrate a normal-appearing epiglottis and arytenoepiglottic folds, with a scalloped appearance on the anterior surface of the vallecula caused by an enlarged lingual tonsil (Fig. 75-2).13
Management includes maintenance of airway patency, antibiotics, and supportive therapy. Rarely, acute lingual tonsillitis may be a life-threatening condition. Airway management includes warmed humidified oxygen, hydration, and corticosteroids. Nebulized epinephrine can relieve the acute respiratory distress and stridor. Antibiotics of choice are similar to those used for the treatment of pharyngitis.13
Laryngitis
Laryngitis is manifested as hoarseness and aphonia. It is usually caused by viral upper respiratory tract infections. In up to 10% of cases, bacterial infections (including streptococcal infection and diphtheria) may be responsible. Rare causative entities are tuberculosis, syphilis, leprosy, actinomycosis, and fungi. Noninfectious causes include tumors, caustic or thermal injuries, trauma, and esophageal reflux disease.14,15 Laryngitis generally is a benign viral illness with peak symptoms lasting 3 to 4 days. “Voice rest” often is recommended, but there is no evidence that this is of any benefit in terms of duration or severity of symptoms. Antibiotics are not indicated unless signs of bacterial infection are present.16 Steroids may hasten resolution of symptoms.17
Adult Epiglottitis
Adult epiglottitis can lead to rapid, unpredictable airway obstruction. The incidence of pediatric epiglottitis has diminished since the introduction of Haemophilus influenzae vaccine. At the same time, there has been an apparent increase in adult epiglottitis, possibly because of increased recognition.1,6,18,19
Principles of Disease
Adult epiglottitis is a localized cellulitis involving the supraglottic structures, including the base of the tongue, vallecula, aryepiglottic folds, arytenoid soft tissues, lingual tonsils, and epiglottis. Inflammation does not extend to the infraglottic regions. Some adults have a normal epiglottis in the setting of severe supraglottic involvement. The term supraglottitis is a more accurate description of this disease process. Adults with epiglottic involvement are prone to epiglottic abscesses.18,19
Adult epiglottitis can be caused by many viral, bacterial, or, rarely, fungal pathogens, but the most commonly isolated bacterial pathogen is H. influenzae type b.20 Although it is isolated from only a minority of affected patients, H. influenzae infection is associated with a more aggressive disease course. The predominant organisms isolated from epiglottic abscesses are Streptococcus and Staphylococcus species. Adult epiglottitis may also result from thermal injury.1,18,19
Clinical Features
Adult epiglottitis has no age or seasonal prevalence. Males and smokers are more commonly affected. Adults with epiglottitis typically experience a prodrome resembling that of a benign upper respiratory tract infection. The duration of the prodrome is usually 1 to 2 days but may be as long as 7 days or as short as several hours. Patients who have a rapid onset of the disease as well as those with comorbid conditions (especially diabetes) are more likely to require airway intervention.1,18,19
Patients typically have dysphagia, odynophagia, and a sore throat. Pain may be severe, and suspicion of epiglottitis is raised when the patient reports severe symptoms of pharyngitis and has obvious odynophagia or dysphagia but examination of the oral pharynx and tonsils shows only minimal or no signs of inflammation or exudate. Ear pain may also be a manifestation of adult epiglottitis. Dysphonia and a muffled voice are common, whereas hoarseness is unusual. Fever is absent in up to 50% of cases and may develop only in the later stages of the disease. Tachycardia disproportionate to fever correlates with severe disease. Tenderness to palpation of the anterior aspect of the neck in the region of the hyoid and when the larynx is moved side to side is a suggestive finding in epiglottitis.21
Concomitant uvulitis, pharyngitis, tonsillitis, Ludwig’s angina, peritonsillar abscess, and parotitis can occur. Symptoms and signs of imminent airway obstruction may not appear until immediately before complete obstruction occurs. Patients who are unable to swallow their own saliva and are spitting into a cup or drooling should be considered to have impending airway compromise. Patients who assume a classic sniffing position are at imminent risk for rapid airway obstruction. These patients should not be laid flat, and immediate preparations made to rapidly secure the airway (see Chapter 1).1,18,19
Diagnostic Strategies
Although severe cases of adult epiglottitis are easily recognized, a large number of less severe cases are initially misdiagnosed.6
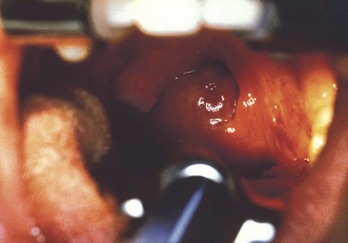
When epiglottitis is suspected, visualization of the epiglottis is indicated. Although indirect laryngoscopy can be used to assess the epiglottis, it provides a much more limited examination of the upper airway structures than is accomplished via flexible or rigid laryngoscopy, either with a conventional laryngoscope or a videolaryngoscope. Depending on the perceived urgency of the airway examination, preparations should include a drying agent, preferably glycopyrrolate 0.2 mg intravenously (IV), topical anesthesia, such as 4% lidocaine by atomizer (after the glycopyrrolate has reduced secretions), and light sedation (such as midazolam in 1-mg increments, often with small doses [50-µg increments] of fentanyl). Necessary equipment to provide bag-mask ventilation, intubation, or cricothyrotomy must be immediately available. Laryngospasm and complete obstruction can occur during instrumentation of the inflamed airway. Flexible laryngoscopy is the preferred approach as it provides direct, minimally invasive examination of the upper airway and because intubation, if necessary, can be completed over the scope if this was planned in advance. Laryngoscopy reveals a swollen epiglottis and surrounding structures (Fig. 75-3). The epiglottis may appear “cherry red” but is often pale and edematous. In patients with respiratory distress, drooling, aphonia, or stridor, the patient is maintained in his or her chosen position to preserve remaining airway patency. Airway examination is undertaken as soon as equipment has been obtained and requires a “double setup” with the ability to proceed immediately to cricothyrotomy.1,19
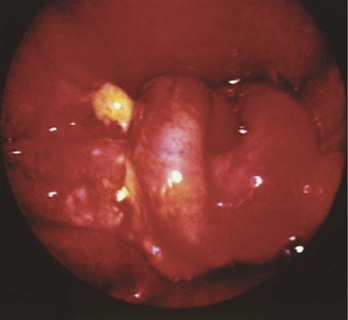
Figure 75-3 Epiglottitis.
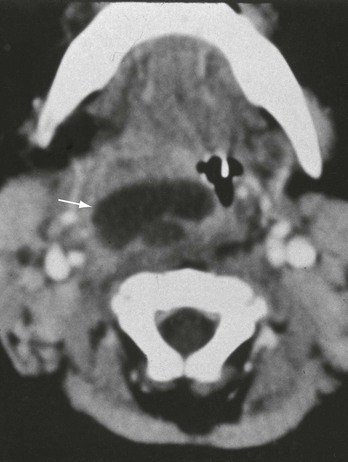
The primary diagnostic technique for adult epiglottitis is laryngoscopy, as described previously. Although lateral cervical soft tissue radiographic films have a sensitivity of up to 90% when compared with the gold standard of laryngoscopy, radiographs are not a substitute for visualization of the upper airway structures by flexible or rigid laryngoscopy. Patients with severe pain, altered voice, complaints of dyspnea, or inability to swallow secretions should undergo prompt upper airway examination and should not be sent to radiology for x-ray examination. Radiologic findings, when present, include obliteration of the vallecula, swelling of the arytenoids and aryepiglottic folds, edema of the prevertebral and retropharyngeal soft tissues, and “ballooning” of the hypopharynx and mesopharynx. The edematous epiglottis appears enlarged and thumb shaped (Fig. 75-4). An epiglottic width greater than 8 mm or an aryepiglottic fold width greater than 7 mm is suggestive of epiglottitis. Adults with possible epiglottitis and normal soft tissue radiographic films should undergo laryngoscopy, because normal soft tissue plain films do not exclude the presence of adult epiglottitis. Similarly, patients determined to have epiglottitis by radiograph also require upper airway examination by laryngoscopy to determine the extent of airway compromise and the need for intubation.
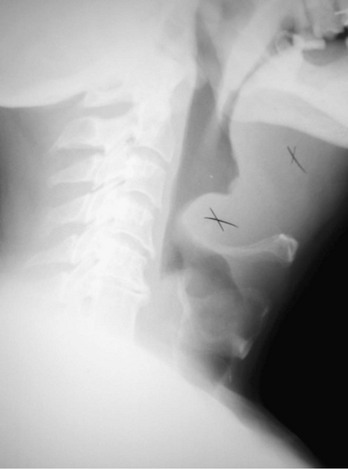
Figure 75-4 Radiograph of epiglottitis.
Management
Most adults with epiglottitis do not require intubation, but all patients with epiglottitis should be treated with extreme care because of the possibility of unpredictable sudden airway obstruction. Endotracheal intubation should be performed under direct visualization. Awake flexible endoscopic intubation is the optimal method, but awake orotracheal intubation by direct laryngoscopy or videolaryngoscopy also can be done.1,19 Blind nasotracheal intubation can lead to airway obstruction and is contraindicated in the setting of epiglottitis.
Antibiotics should be initiated against H. influenzae and other likely bacterial pathogens. First-line agents pending culture and sensitivity results are cefotaxime and ceftriaxone. Alternative antibiotics include ampicillin-sulbactam and trimethoprim-sulfamethoxazole.1,10,11 The role of steroids is unresolved, but racemic epinephrine is used only as a temporizing measure while preparations are made to secure the airway, because short-term use can produce improvement, only to be followed by a “rebound” effect in which the symptoms and signs revert to their pretreatment level of severity or become even worse.20
Disposition
If upper airway endoscopy shows mild or moderate disease with preservation of a widely patent airway, and the patient’s symptoms have developed gradually over a long period of time (i.e., 24 hours), treatment with intravenous antibiotics, parenteral opioid analgesia, and humidified oxygen in a monitored inpatient unit (often the intensive care unit [ICU]) or an ED observation unit is appropriate, providing the patient is without dyspnea and is handling his or her secretions. Laryngoscopy is repeated in 6 to 12 hours to ensure that the patient’s condition is improving and to determine readiness for discharge. Even with only moderate laryngoscopic findings, in patients with a rapidly progressive course, such as those whose symptoms have increased greatly in severity over 4 to 6 hours, preventative intubation is indicated, as progression of swelling and airway compromise can occur rapidly and with little warning. Intubation also is undertaken despite only moderate findings on laryngoscopy for patients who are immunocompromised or diabetic or who have an epiglottic abscess.1,18,19 For patients admitted to the hospital, consultation with an otolaryngologist should be arranged.
Deep Space Infections of the Lower Part of the Face and Neck
Patients with deep space infections of the head and neck (Fig. 75-5) can decompensate rapidly. The incidences and complications of deep space infections have decreased dramatically because of improved dental hygiene and antibiotics.22
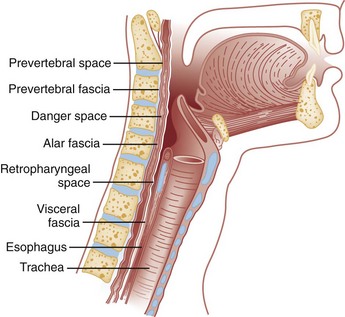
The submandibular space comprises two spaces: the sublingual and submaxillary spaces. The submandibular space is involved in Ludwig’s angina.23 Five potential communicating spaces in the neck are clinically relevant. The parapharyngeal space contains the carotid artery, the jugular vein, the cervical sympathetic chain, and cranial nerves IX through XII. The retropharyngeal space lies in the midline (medial to the parapharyngeal space) and extends from the base of the skull to the superior mediastinum (at about the level of T2). Retropharyngeal abscesses tend to occur lateral to the midline. Posterior to the retropharyngeal space lies the “danger” space, which extends from the base of the skull to the diaphragm. The prevertebral space extends from the base of the skull to the coccyx. Danger space and prevertebral abscesses are located in the midline. Infections in the retropharyngeal, danger, and prevertebral spaces easily access the mediastinum. There is little anatomic resistance to spread of infection within the fascial planes and spaces, which allows rapid spread of infection and life-threatening complications.22,24
The primary pathologic process of deep space infection is regional cellulitis. The fasciae may confine infections within their boundaries, thereby leading to abscess formation. Infections are most commonly caused by polymicrobial mixed aerobic-anaerobic oral bacteria. The most frequently isolated organisms are streptococci, staphylococci, and Bacteroides species. β-Lactamase–producing organisms are isolated in up to two thirds of cases. Other organisms include H. influenzae, Pseudomonas aeruginosa, Klebsiella species, and Candida albicans.22,23,25
Ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) can help distinguish cellulitis from abscess formation and guide therapy. Patients with cellulitis usually respond well to high-dose antibiotic therapy. Patients with small abscesses can be successfully treated with high-dose intravenous antibiotics or needle aspiration. The presence of a larger abscess, however, usually requires surgical incision and drainage. With the exception of patients with uncomplicated peritonsillar abscesses, patients with deep space abscess usually require admission and intravenous antibiotics, and consultation with otolaryngologists for possible surgical intervention is usually necessary.26
Airway distortion and trismus may complicate intubation attempts. Neuromuscular blockade is generally ill-advised, unless as part of a double setup with the ability to proceed directly to cricothyrotomy, because both intubation and bag-mask ventilation may be difficult or impossible. Neuromuscular blockade may not resolve trismus, so use of a neuromuscular blocking agent must be part of a double setup intubation. Awake, flexible endoscopy intubation techniques are preferable.22,23,27 Blind nasotracheal intubation is contraindicated.23,27 Should it be necessary to secure an airway surgically, cricothyroidotomy is the procedure of choice, except in some cases of Ludwig’s angina, in which anatomic distortion may necessitate tracheostomy.
Peritonsillitis (Peritonsillar Cellulitis and Peritonsillar Abscess)
Principles of Disease
Peritonsillitis may occur as a result of acute tonsillitis. Infection in either Weber’s glands or the tonsillar crypts invades the peritonsillar tissues and thereby leads to cellulitis and abscess formation. Fibrous fascial septae divide the peritonsillar space into compartments and direct the infection anteriorly and superiorly.1,22
Most peritonsillar abscesses are polymicrobial. β-Lactamase–producing organisms are isolated more commonly in patients who have received prior antibiotics.1,22
Clinical Features
The examination of the pharynx can be limited by trismus. Physical findings of peritonsillitis include inflamed and erythematous oral mucosa, purulent tonsillar exudates that obscure the tonsil, and tender cervical lymphadenopathy. Peritonsillar cellulitis mimics peritonsillar abscess. Peritonsillar abscess is characterized by a greater frequency of drooling, trismus, and dysphagia, whereas peritonsillar cellulitis is more commonly bilateral. The distinguishing feature of peritonsillar abscess is inferior medial displacement of the infected tonsil (at times involving the soft palate), with contralateral deviation of the uvula (Fig. 75-6). The abscess is generally unilateral and located in the superior pole of the tonsil. Bilateral peritonsillar abscesses occur occasionally.1,22
Diagnostic Strategies
Aspiration of pus establishes the diagnosis of peritonsillar abscess. Because patients with peritonsillar abscess have a 20% incidence of mononucleosis, laboratory testing for mononucleosis should be considered when systemic symptoms or findings of mononucleosis are present (see Chapter 130.)
Radiographs are of no value when clinical examination identifies peritonsillar abscess. Although contrast-enhanced CT and ultrasonography (both intraoral and transcutaneous) aid in differentiating peritonsillar abscess from cellulitis, especially when patients are unable to cooperate with needle aspiration, these rarely, if ever, are required. Ultrasound, if available, may be useful in guiding needle aspiration.22,26,28
Management
Needle aspiration is indicated when abscess is present or suspected. Antibiotics alone may suffice with peritonsillar cellulitis. Regimens include high-dose penicillin plus metronidazole, cefoxitin, ampicillin-sulbactam, and clindamycin. Alternative antimicrobial agents include a carbapenem, high-dose penicillin and rifampin, ticarcillin-clavulanate, or piperacillin-tazobactam.1,10,22 The use of steroids may also be beneficial.29
Drainage of an abscess is usually curative. Needle aspiration of abscesses by both emergency physicians and otolaryngologists is diagnostic (although false-negative aspirations occur in approximately 10% of cases, and another 10% may require repeated aspirations) and therapeutic. This immediately relieves symptoms and is more cost-effective, less painful, and easier to perform than incision and drainage.1,22,28,29 Intraoral ultrasound-guided needle aspiration is a useful adjunct in the presence of trismus.28,29
Disposition
Hospital admission rarely is indicated but is considered for patients who have significant comorbidity, appear toxic, or are unable to tolerate oral fluids or whose pain is not managed by oral analgesics. Most patients can be observed for 4 to 6 hours after aspiration in the ED observation unit or the ED, receiving antibiotics, intravenous hydration, and analgesia. The most dangerous immediate complication of peritonsillitis is pharyngeal obstruction with upper airway compromise. Other complications include sepsis, abscess rupture and pulmonary aspiration leading to pneumonia, empyema, and pulmonary abscess formation. Infection can spread contiguously to the parapharyngeal and retropharyngeal spaces. Ludwig’s angina, mediastinal involvement (including mediastinitis, pneumonia, empyema, and pericarditis), myocarditis, carotid artery erosion, jugular vein thrombophlebitis, septic embolization, abscess formation, Lemierre’s syndrome (see discussion in parapharyngeal abscess section), and cervicothoracic necrotizing fasciitis can complicate peritonsillitis. Intracranial extension of peritonsillitis may result in meningitis, cavernous sinus thrombosis, and cerebral abscess.22
Ludwig’s Angina
Perspective and Principles of Disease
Ludwig’s angina is a potentially fulminant disease process that can lead to death within hours.23,25,30 This is a progressive cellulitis of the connective tissues of the floor of the mouth and neck that begins in the submandibular space. Dental disease is the most common cause of Ludwig’s angina. An infected or recently extracted lower molar is noted in most affected patients.23,25,30 Other causes of Ludwig’s angina include a fractured mandible, a foreign body or laceration in the floor of the mouth, tongue piercing, traumatic intubation and bronchoscopy, secondary infections of an oral malignancy, osteomyelitis, otitis media, submandibular sialadenitis, a peritonsillar abscess, a furuncle, an infected thyroglossal cyst, and sepsis.23,25
Clinical Features
Infection of the sublingual and submaxillary spaces leads to edema and soft tissue displacement, which may result in airway obstruction. The most common presentation in patients with Ludwig’s angina includes dysphagia, odynophagia, neck swelling, and neck pain. Other symptoms and signs include dysphonia, a hot potato voice, dysarthria, drooling, tongue swelling, pain in the floor of the mouth, restricted neck movement, and sore throat. Patients should be questioned regarding recent dental extraction and disease. Rapid development of crepitus and unilateral pharyngitis in patients with recent dental extractions should suggest the diagnosis of Ludwig’s angina.23,25,30
The most common physical findings in Ludwig’s angina are bilateral submandibular swelling and elevation or protrusion of the tongue. Other findings include elevation of the floor of the mouth, posterior displacement of the tongue, and a “woody” consistency of the floor of the mouth. The combination of tense edema and brawny induration of the neck above the hyoid may be present and is described as a “bull neck.” Marked tenderness to palpation of the neck and subcutaneous emphysema may be noted. Usually trismus and fever are present, but there is no palpable fluctuance or cervical lymphadenopathy. Tenderness to percussion may be elicited over the involved teeth.23,25,30
Diagnostic Strategies
The diagnosis is made clinically. Soft tissue plain films of the neck may confirm the diagnosis by identifying swelling of the affected area and airway narrowing and gas collections but in general are not of value. CT and MRI can identify deep space neck infections and airway compromise. Ultrasonography is also useful in diagnosing abscesses and edema in the setting of Ludwig’s angina.23,25,30
Management
Sudden asphyxiation is the most common cause of death in patients with Ludwig’s angina.25 Stridor, tachypnea, dyspnea, inability to handle secretions, and agitation all suggest impending airway compromise. Flexible endoscopically guided oral or nasal intubation under sedation with topical anesthesia is the preferred method of airway control. Direct laryngoscopy can be particularly difficult because of inability to retract the tongue into the submandibular space, and posterior and cephalad displacement of the tongue by the infection.25 There is no literature reporting the use of video laryngoscopes in this condition. Cricothyrotomy may be difficult and opens tissue planes that increase the risk of spreading infection into the mediastinum but is the procedure of choice if flexible endoscopic intubation cannot be accomplished.27
Emergent high-dose intravenous antibiotic regimens are used as for peritonsillar abscess.10,25,30 The value of corticosteroids in the setting of Ludwig’s angina is unclear. With the exception of dental extractions, surgery is reserved for patients who do not respond to medical therapy and those with crepitus and purulent collections.23,25,30
Disposition
The mortality rate associated with Ludwig’s angina is less than 10% with early aggressive antibiotic therapy and adequate protection of the airway. Infection can easily spread into other deep spaces of the neck and into the thoracic cavity and cause empyema, mediastinitis, mediastinal abscess, and pericarditis. Aspiration may lead to pneumonia and the formation of lung abscesses. Other complications include internal jugular vein thrombosis, carotid artery infection and erosion, bacteremia and sepsis, pneumoperitoneum, subphrenic abscess, cervicothoracic necrotizing fasciitis, and spontaneous pneumothorax.23,25,30
Retropharyngeal Abscess
Perspective and Principles of Disease
Retropharyngeal abscess is an uncommon condition that previously was a disease of childhood, with 96% of cases occurring in patients younger than 6 years. Adults are now increasingly affected.10,26,31 In adult patients, cellulitis develops in the retropharyngeal area.26 Once the retropharyngeal space is involved, the infection spreads rapidly and an abscess may form. Nasopharyngitis, otitis media, parotitis, tonsillitis, peritonsillar abscess, dental infections and procedures, upper airway instrumentation, endoscopy, lateral pharyngeal space infection, and Ludwig’s angina are all implicated in the development of retropharyngeal abscess. Other causes include blunt and penetrating trauma (usually from foreign bodies, commonly fish bones), ingestion of caustic substances, vertebral fractures, and hematologic spread from distant infection.22,31 Vertebral osteomyelitis and diskitis may lead to infection of the prevertebral space. Danger space infections are caused by extension of infection from either the retropharyngeal or prevertebral space. Underlying systemic disorders (e.g., diabetes and depressed immune system) may predispose individuals to retropharyngeal infections.22,31
Retropharyngeal abscesses are most commonly polymicrobial, with a mixture of aerobes and anaerobes. β-Lactamase–producing organisms are present in two thirds of the cases. Tuberculosis is rarely reported in the United States as a cause of retropharyngeal abscess. Staphylococcus is the most common cause of pyogenic vertebral osteomyelitis, leading to the formation of retropharyngeal abscess. Disseminated coccidioidomycosis may also cause retropharyngeal abscess.22,26,31,32
Clinical Features
Patients typically have a sore throat, dysphagia, odynophagia, drooling, a muffled voice, neck stiffness, neck pain, and fever. Dysphonia is usually present and is described as a duck “quack” (cri du canard). Patients may report feeling a lump in the throat. Patients with a retropharyngeal abscess may appear quite ill and generally prefer to hold their necks extended and remain in the supine position. This position keeps the swollen posterior pharynx from compressing the upper airway. Forcing the patient to sit may lead to increased dyspnea.22,30
Physical examination may reveal tender cervical lymphadenopathy and cervical musculature, neck swelling, torticollis, and a high fever. Trismus may be present and make visualization of the pharynx difficult. With retropharyngeal cellulitis, diffuse edema and erythema of the posterior pharynx are present.22,30 Once an abscess has developed, palpation of the pharynx may demonstrate a unilateral mass if the retropharyngeal space is affected and a midline mass if the abscess is in the prevertebral or danger space. Palpation of a fluctuant mass is unreliable and carries a risk of inadvertent rupture. Tenderness on moving the larynx and trachea side to side (tracheal “rock” sign) is commonly present. A retropharyngeal abscess may also cause pain in the back of the neck or shoulder that is precipitated by swallowing. Cold abscesses (caused by tuberculosis) are characterized by insidious onset, chronicity, constitutional symptoms, and a lower fever. Symptoms disproportionate to the findings should prompt further evaluation.32
Diagnostic Strategies
Plain films may not be sufficiently sensitive to diagnose retropharyngeal abscess. CT or MRI should be performed when doubt persists after plain x-ray examination. These studies not only aid in the diagnosis and differentiation between cellulitis and abscess but also determine the extent of the disease process and the presence of complications (Fig. 75-7).24,26,32 Ultrasonography is useful for differentiating retropharyngeal cellulitis from retropharyngeal abscess.
Differential Diagnosis Considerations
The differential diagnosis includes retropharyngeal tumors, foreign bodies, inflammation, hematoma, aneurysms, hemorrhage, lymphadenopathy, and edema. Other considerations include tendinitis of the longus colli muscle and retropharyngeal thyroid tissue.24
Management
Patients with retropharyngeal cellulitis are best treated with high-dose intravenous antibiotics. Appropriate regimens are similar to those used for peritonsillar abscess. Tuberculosis and fungal infections also are considered. Resolution of retropharyngeal cellulitis is possible without surgical intervention.10,22,26,30,32
In general, retropharyngeal abscesses are treated with antibiotics, in conjunction with operative incision and drainage by an otolaryngologist. In selected cases, retropharyngeal abscesses can be treated successfully with antibiotics alone or in combination with needle aspiration. Tuberculous (cold) abscesses should be drained only extraorally, unless the patient is in acute respiratory distress. Ear, nose, and throat (ENT) and infectious disease consultation is advised when TB is suspected as the causative agent.26,30,32
Disposition
Airway compromise can be caused by anterior displacement of the pharyngeal tissues. Pulmonary complications include abscess rupture with aspiration and subsequent pneumonia, empyema, and asphyxiation. Extension of the infection along tissue planes and through other deep spaces may lead to mediastinitis and mediastinal abscess formation, pericarditis, pleuritis, and empyema. In addition, abscesses may track into the back of the neck and into the axillae. Vascular complications occur from the extension of the retropharyngeal abscess into the lateral pharyngeal space. Atraumatic atlantoaxial separation is caused by damage to the transverse ligament of the atlas from the abscess. These patients may have neurologic symptoms and a widened predental space on plain films, CT scans, or MRI images. Acute transverse myelitis and epidural abscesses also occur, and both can result in quadriplegia. Other complications include internal carotid pseudoaneurysm, erosion into the esophagus and auditory canal, necrotizing fasciitis of the neck, acute respiratory distress syndrome, sepsis, and death.22,32
Parapharyngeal Abscess
The parapharyngeal space, also known as the lateral pharyngeal and pharyngomaxillary space, is divided into two compartments by the styloid process. The anterior compartment contains connective tissue, muscle, and lymph nodes. The carotid sheath (which contains the carotid artery, the internal jugular vein, the vagus nerve, cranial nerves IX through XII, and the cervical sympathetic chain) runs in the posterior compartment.22
Principles of Disease
Parapharyngeal abscesses are most often polymicrobial infections. Odontogenic and pharyngotonsillar infections are the most common causes of parapharyngeal space abscesses. Parapharyngeal space infections can also arise by contiguous spread from other surrounding deep neck space infections. Other causes include parotitis, sinusitis, spread from infected neck tumors, infected branchial cleft cysts, suppuration of local lymphadenitis, iatrogenic introduction of organisms during a mandibular nerve block or anesthesia for tonsillectomy, nasal intubation, dental extraction, chronic otitis with cholesteatoma, and mastoiditis.22
Clinical Findings
Pain and swelling of the neck are the most common complaints. Odynophagia is present in most patients. A history of an antecedent sore throat may be elicited in some patients. Torticollis caused by irritation of the sternocleidomastoid muscle is also reported.22
The classic physical findings of infection involving the anterior compartment of the parapharyngeal space are medial tonsillar displacement and posterolateral pharyngeal wall bulging. Other findings include fever, trismus (caused by irritation of the muscles of mastication), edema, and swelling at the angle of the jaw. An erythematous, tender, nonfluctuant swelling at the angle of the mandible is a consistent finding in patients with an anterior parapharyngeal abscess.22
Involvement of the posterior space is associated with many of these same signs. If the anterior compartment is spared, however, little or no trismus occurs. Instead, posterior displacement of the tonsillar pillar and retropharyngeal swelling may be present.22
Diagnostic Strategies and Differential Diagnosis Considerations
The diagnosis of parapharyngeal abscess is suggested by the presence of a severe sore throat with the characteristic physical findings. Jugular vein thrombophlebitis that complicates parapharyngeal space infection may be suggested by positive blood cultures. Ultrasonography, CT, and MRI are more useful than lateral radiographs in diagnosing parapharyngeal abscess and its complications. Angiography, Doppler flow studies, and magnetic resonance angiography may also be helpful in evaluating vascular complications.22,26,33
Management
Treatment includes high-dose intravenous antibiotics and consultation with an otolaryngologist for surgical drainage. Appropriate antibiotic regimens are those used for peritonsillar abscess. Intravenous antibiotics alone will cure parapharyngeal space infections in patients without abscess.10,22,26,33,34 Successful resolution of parapharyngeal abscesses with intravenous antibiotics and needle aspiration has been reported.26,33
Disposition
Complications of a parapharyngeal abscess include airway obstruction and abscess rupture with subsequent aspiration, pneumonia, and empyema. Infection can spread to surrounding spaces and into the mediastinum and pericardium. Such spread may lead to mediastinitis, mediastinal abscess, pericarditis, myocardial abscess, and empyema. Other complications include osteomyelitis of the mandible, cervicothoracic necrotizing fasciitis, parotid abscess, cavernous sinus thrombosis, and meningitis.22
Posterior parapharyngeal space infections are particularly dangerous. These infections may affect the cervical sympathetic chain, carotid artery, or internal jugular vein. Ipsilateral Horner’s syndrome and neuropathies of cranial nerves IX through XII may occur. Carotid artery erosion may lead to hemorrhage and the formation of aneurysms. Oral, nasal, and aural warning bleeding is common with carotid artery erosion, with aural bleeding being particularly ominous. Any unexplained bleeding associated with parapharyngeal or other deep neck space infection should be investigated thoroughly. Persistent peritonsillar swelling, despite resolution of the parapharyngeal abscess or a tender unilateral pulsatile mass, may indicate an arterial aneurysm. Aspiration or incision of a carotid artery aneurysm thought to be a parapharyngeal abscess may have disastrous complications.22
Involvement of the internal jugular vein may lead to septic thrombosis and Lemierre’s syndrome.1,35 This entity, also called postanginal septicemia, affects primarily young healthy patients and is easily confused with right-sided endocarditis or aspiration pneumonia. The manifestation is one of a pharyngitis that initially improves but is then followed by severe sepsis. It is thought that the pharyngeal infection spreads to the parapharyngeal space and causes septic thrombophlebitis of the jugular vein. Patients usually appear ill and are febrile. Metastatic infections involve primarily the lung and are manifested by bilateral nodular infiltrates, pleural effusion, and pneumothorax. Septic arthritis, osteomyelitis, soft tissue cellulitis and abscesses, meningitis, and a vesiculopustular rash are also reported as a result of septic embolization. Leukocytosis and elevated bilirubin and liver function test values, with and without hepatomegaly and jaundice, are often present. Albuminuria, hematuria, and elevations in serum creatinine and blood urea nitrogen are reported. Septic shock rarely develops, although acute respiratory distress syndrome, transient coagulopathies, and hypotension commonly occur. The most frequent cause of this entity is Fusobacterium (primarily Fusobacterium necrophorum), although Staphylococcus aureus is the most common pathogen in intravenous drug users. Treatment consists of parenteral antibiotics (high-dose penicillin or clindamycin) and incision and drainage of abscesses. Jugular vein ligation and resection are necessary in patients with uncontrolled sepsis and respiratory failure caused by repeated septic pulmonary emboli. The value of anticoagulation is unknown.1,35
Rhinosinusitis
Perspective and Principles of Disease
As sinusitis usually involves the nasal cavity, the term rhinosinusitis is preferred. These terms will be used interchangeably in this section.36,37
The paranasal sinuses (frontal, maxillary, ethmoid, and sphenoid) are named for the facial bones with which they are associated. Pneumatization may involve other bones but represents extension from the main sinus. The maxillary, anterior ethmoid, and frontal sinuses drain into the medial meatus, located between the inferior and middle nasal turbinates. This area is named the ostiomeatal complex and is the focal point of sinus disease. The posterior ethmoid sinus drains into the superior meatus and the sphenoid sinus just above the superior turbinate.36,37
A healthy sinus is sterile, depends on a patent ostium with free air exchange, and is reliant on appropriate mucus drainage. Many different processes can result in ostial obstruction and rhinosinusitis, but the most common are viral upper respiratory tract infections and allergic rhinitis. Ciliary abnormality or immobility also inhibits drainage, resulting in sinusitis. Bacteria are introduced into the sinus by coughing and vigorous nose blowing, leading to increased inflammation and bacterial overgrowth. Other factors predisposing to rhinosinusitis include immunocompromised status, nasal septal deviation and other structural abnormalities, nasal polyps, tumors, trauma and fractures, rhinitis medicamentosa, rhinitis secondary to toxic mucosal exposure, barotrauma, foreign bodies, nasal cocaine abuse, and instrumentation (including nasogastric and nasotracheal intubation).36,37
Sinusitis can be classified into acute viral, acute bacterial, chronic, and recurrent acute variations. Approximately 90% of patients with colds have an element of the acute viral form. Acute viral sinusitis may lead to the development of the acute bacterial variety. Streptococcus pneumoniae, nontypable H. influenzae, and M. catarrhalis are the primary pathogens responsible for acute bacterial and recurrent acute sinusitis. P. aeruginosa is associated with sinusitis in the setting of HIV infection and cystic fibrosis. Anaerobic bacteria, streptococcal species, and S. aureus are more prominent causes of chronic sinusitis. Fungi also have a role in chronic sinusitis. Rhizopus, Aspergillus, Candida, Histoplasma, Blastomyces, Coccidioides, and Cryptococcus species, as well as other fungi, may cause sinusitis, primarily in immunocompromised hosts. It is important to distinguish infectious from allergic sinusitis. Allergic sinusitis is associated with sneezing, itchy eyes, allergen exposure, and previous episodes.36–39
Clinical Features
Frontal sinusitis can cause severe headache localized to the forehead and orbit. Sphenoid sinusitis may cause vague headaches and focal pain almost anywhere in the head. Maxillary sinusitis may be seen with pain over the zygoma, in the canine or bicuspid teeth, or periorbitally. Ethmoid sinusitis can cause medial canthal pain and periorbital or temporal headaches.36,37,40
The cardinal findings of acute rhinosinusitis are mucopurulent nasal discharge, nasal obstruction or congestion, and facial pain, fullness, or pressure lasting less than 4 weeks. Other symptoms and signs include postnasal drip (which may lead to coughing), pressure over the involved sinus, malaise, hyposmia, anosmia, fever, maxillary dental pain, and ear fullness or pressure. Acute sinusitis typically progresses over a period of 7 to 10 days and resolves spontaneously. During the first 3 to 5 days of illness, it may be difficult to differentiate acute viral from acute bacterial sinusitis, and antibiotics are not indicated in this phase, as most cases are viral and will resolve without treatment. When symptoms persist beyond 10 days, bacterial sinusitis is more likely, and treatment is indicated. Bacterial origin also is suggested by “double sickening,” which refers to patients who improve initially, only to have worsening sinus congestion and discomfort.36,37,40
Chronic sinusitis is slow in onset, prolonged in duration (greater than 12 weeks), and recurrent in frequency. Symptoms can be nonspecific but are generally similar to those of acute disease. Symptoms of chronic disease may also include chronic cough, fetid breath, laryngitis, bronchitis, and worsening asthma. Recurrent acute sinusitis is diagnosed when four or more episodes of acute bacterial infection, without its symptoms or signs between episodes, occur per year. The presentation and treatment of recurrent acute disease is similar to that for acute bacterial sinusitis.36,37,40 Invasive fungal sinusitis (mucormycosis) is an aggressive opportunistic rhinocerebral infection that affects immunocompromised hosts. Mucormycosis (Rhizopus) is generally associated with fever, localized nasal pain, and cloudy rhinorrhea. On examination, the affected tissue (usually the turbinates) appears gray, friable, anesthetic, and nonbleeding because of infarction caused by mucormycotic angioinvasion. In advanced cases the affected tissues are necrotic and black, and the infection spreads beyond the sinus.38,39
Diagnostic Strategies
Physical examination is best performed after the application of a topical decongestant. Mucosal erythema and edema are usually present. Purulent discharge from the nasal meatus may be observed if the sinus ostia are not completely obstructed. In the setting of acute sinusitis, nasal and nasopharyngeal cultures do not differentiate between acute viral and acute bacterial infections. Culture and biopsy are indicated in suggested chronic, recurrent acute, and fungal sinusitis.36,37
For suspected acute sinusitis, routine radiographic examination is not recommended and should be limited to diagnosis of chronic or recurrent acute sinusitis, cases of questionable diagnoses, patients with unresponsive disease, or investigation of complications. Axial and coronal CT is the imaging modality of choice. CT findings suggestive of sinusitis include air-fluid levels, sinus opacification, sinus wall displacement, and mucosal thickening. CT is sensitive, though not specific. Incidental sinus mucosal thickening is seen in 40% of asymptomatic patients, and abnormal CT findings can also be noted in just half of patients with seasonal allergies. CT with intravenous contrast or MRI may be required to evaluate complications of rhinosinusitis and are helpful in determining alternative diagnoses. Sinus endoscopy is another option.36,37
Management
Decongestant therapy, available in topical and systemic preparations, can be used to reduce tissue edema, facilitate drainage, and maintain patency of the sinus ostia.31,36 Topical agents provide more relief than systemic decongestants. Longer-acting agents, such as 0.05% oxymetazoline hydrochloride, which is available in generic forms, are easy to use and highly effective. Topical agents should be used for up to 5 days, as extended use results in rebound vasodilation and nasal obstruction, a condition termed rhinitis medicamentosa. Systemic oral adrenergic agonists (e.g., phenylpropanolamine or pseudoephedrine) reduce nasal blood flow and congestion. These medications have no advantage over topical agents and have significant systemic effect, so they should not be used unless the patient is not willing to use topical decongestants. They should not be used in patients with poorly controlled hypertension or patients who are taking tricyclic antidepressants, monoamine oxidase inhibitors, or nonselective beta-adrenergic blockers.36,37 Topical, but not systemic, steroids are indicated for chronic and allergic sinusitis. Systemic steroids may be indicated in allergic and chronic sinusitis with nasal polyps.36,38,41
Saline nasal irrigation is beneficial for treatment of acute bacterial, recurrent acute, and chronic sinusitis and even may be efficacious for the prevention of sinusitis. Hypertonic saline preparations have superior anti-inflammatory properties and may be more effective than normal saline.36,37
The choice of antibiotics should consider β-lactamase production and multidrug-resistant pneumococci. High-dose amoxicillin, 1 g three times a day administered for 7 to 10 days, is still the first-line agent, but benefits are limited, and treatment failures occur in areas with a high percentage of β-lactamase–producing bacteria.10,36,37 High-dose amoxicillin should be considered for patients who have a child in daycare in the household. Penicillin-allergic patients may be treated with trimethoprim-sulfamethoxazole or a macrolide antibiotic. A 3-day course of trimethoprim-sulfamethoxazole or azithromycin and decongestants may be as effective as the standard 10-day antibiotic course.36,37
Failure of symptoms to resolve after 7 days of therapy, or antibiotic usage in the previous 4 to 6 weeks, necessitates a change to a broader-spectrum antibiotic, reassessment of the patient to confirm the diagnosis of acute bacterial sinusitis, and referral to an otolaryngologist. Appropriate management includes a 10- to 14-day course of high-dose amoxicillin-clavulanate, cefuroxime axetil, other second- or third-generation cephalosporins, clindamycin alone or in combination with ciprofloxacin, sulfamethoxazole, azithromycin, clarithromycin, or one of the respiratory fluoroquinolones (levofloxacin, moxifloxacin, gemifloxacin). Metronidazole may be added to any of these regimens to increase activity against anaerobic organisms. Treatment of life-threatening complications requires consultation and high-dose intravenous antibiotics, including cefuroxime, ceftriaxone, one of the respiratory fluoroquinolones, or ampicillin-sulbactam.10,36,37,42 Patients with chronic sinusitis should be referred to an otolaryngologist. Antibiotics for chronic sinusitis should be effective against anaerobic and β-lactamase–producing bacteria. Antifungals may be beneficial in the treatment of chronic sinusitis.38,39
Complications
Infectious processes of the sinuses can spread to the orbit or central nervous system and can be fulminant. Sinusitis may extend to involve the bones and soft tissues of the face and orbit. Facial and periorbital cellulitis, periorbital abscess, optic neuritis, blindness, and orbital abscess may develop. Patients with orbital complications may have marked swelling, proptosis, decreased ocular motility, and decreased visual acuity. Sinusitis may also lead to intracranial complications. Meningitis, cavernous sinus thrombosis, epidural or subdural empyema, and brain abscess occur. Intracranial involvement may result in headache, decreased sensorium, or focal neurologic deficits and has a rapidly progressive course. Acute fulminant fungal sinusitis requires intravenous antifungal therapy and aggressive surgical débridement.36,37,39 Complications of mucormycosis are directly related to delay in diagnosis and treatment. This opportunistic fungal infection rapidly progresses to involve the central nervous system and is associated with high morbidity and mortality rates. Sinusitis is associated with an increased incidence of bronchitis and asthma.
References
1. Alcaide, ML, Bisno, AL. Pharyngitis and epiglottitis. Infect Dis Clin North Am. 2007;21:449.
2. Bisno, AL. Acute pharyngitis. N Engl J Med. 2001;344:205.
3. Esposito, S, et al. Acute tonsillopharyngitis associated with atypical bacterial infection in children: Natural history and impact of macrolide therapy. Clin Infect Dis. 2006;43:206.
4. Tiemstra, J, Miranda, RL. Role of non–group A streptococci in acute pharyngitis. J Am Board Fam Med. 2009;22:663.
5. Bisno, AL, et al. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Clin Infect Dis. 2002;35:113.
6. Snow, V, et al. Principles of appropriate antibiotic use for acute pharyngitis in adults. Ann Intern Med. 2001;134:506.
7. Cooper, RJ, et al. Principles of appropriate antibiotic use for acute pharyngitis in adults: Background. Ann Intern Med. 2001;134:509.
8. Del Mar, CB, Glasziou, PP, Spinks, AB. Antibiotics for sore throat. Cochrane Database Syst Rev. 2006;4:CD000023.
9. Casey, JR, Pichichero, ME. The evidence base for cephalosporin superiority over penicillin in streptococcal pharyngitis. Diagn Microbiol Infect Dis. 2007;57(Suppl 3):39S.
10. Gilbert DN, Moellering RC, Eliopoulos GM, Chambers HF, Saag MS, eds. The Sanford Guide to Antimicrobial Therapy, 40th ed, Sperryville, Va: Antimicrobial Therapy Inc, 2010.
11. Marvez-Valls, EG, Stuckey, A, Ernst, AA. A randomized clinical trial of oral versus intramuscular delivery of steroids in acute exudative pharyngitis. Acad Emerg Med. 2002;9:9.
12. Bulloch, B, Kabani, A, Tenenbein, M. Oral dexamethasone for the treatment of pain in children with acute pharyngitis: A randomized, double-blind, placebo-controlled trial. Ann Emerg Med. 2003;41:601.
13. Allen, DM, Hall, KN, Barkman, HW. Lingual tonsillitis: An uncommon cause of airway compromise responsive to epinephrine [letter]. Am J Emerg Med. 1991;9:622.
14. Napierkowski, J, Wong, RK. Extraesophageal manifestations of GERD. Am J Med Sci. 2003;326:285.
15. Joniau, S, et al. Reflux and laryngitis: A systematic review. Otolaryngol Head Neck Surg. 2007;136:686.
16. Reveiz, L, Cardona, AF, Ospina, EG, Antibiotics for acute laryngitis in adults. Cochrane Database Syst Rev. 2007;(2):CD004783.
17. Colton RH, Casper JK, eds. Understanding Voice Problems. A Physiological Perspective for Diagnosis and Treatment, 2nd ed, Baltimore: Williams & Wilkins, 1996.
18. Berger, G, et al. The rising incidence of adult acute epiglottitis and epiglottic abscess. Am J Otolaryngol. 2003;24:374.
19. Chang, YL, Lo, SH, Wang, PC, Shu, YH. Adult acute epiglottitis: Experiences in Taiwanese setting. Otolaryngol Head Neck Surg. 2005;132:689.
20. Sack, JL, Brock, CD. Identifying acute epiglottitis in adults. High degree of awareness, close monitoring are key. Postgrad Med. 2002;112:81.
21. Ehara, H. Tenderness over the hyoid bone can indicate epiglottitis in adults. J Am Board Fam Med. 2006;19:517.
22. Brook, I. Microbiology and management of peritonsillar, retropharyngeal and parapharyngeal abscesses. J Oral Maxillofac Surg. 2004;62:1545.
23. Bansal, A, Miskoff, J, Lis, RJ. Otolaryngologic critical care. Crit Care Clin. 2003;19:55.
24. Chong, VF, Fan, YF. Radiology of the retropharyngeal space. Clin Radiol. 2000;55:740.
25. Barakate, MS, Jensen, MJ, Hemli, JM, Graham, AR. Ludwig’s angina: Report of a case and review of management issues. Ann Otol Rhinol Laryngol. 2001;110:453.
26. McClay, JE, Murray, AD, Booth, T. Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography. Arch Otolaryngol Head Neck Surg. 2003;129:1207.
27. Ovassapian, A, Tuncbilek, M, Weitzel, EK, Joshi, CW. Airway management in adult patients with deep neck infections: A case series and review of the literature. Anesth Analg. 2005;100:585.
28. Blaivas, M, Theodoro, D, Duggal, S. Ultrasound-guided drainage of peritonsillar abscess by the emergency physician. Am J Emerg Med. 2003;21:155.
29. Johnson, RF, Stewart, MG. The contemporary approach to diagnosis and management of peritonsillar abscess. Curr Opin Otolaryngol Head Neck Surg. 2005;13:157.
30. Srirompotong, S, Art-Smart, T. Ludwig’s angina: A clinical review. Eur Arch Otorhinolaryngol. 2003;260:401.
31. Craig, FW, Schunk, JE. Retropharyngeal abscess in children: Clinical presentation, utility of imaging, and current management. Pediatrics. 2003;111:1394.
32. Kamath, MP, Bhojwani, KM, Kamath, SU, Mahabala, C, Agarwal, S. Tuberculous retropharyngeal abscess. Ear Nose Throat J. 2007;86:236.
33. Oh, JH, Kim, Y, Kim, CH. Parapharyngeal abscess: Comprehensive management protocol. ORL J Otorhinolaryngol Relat Spec. 2006;69:37.
34. Sichel, JY, Dano, I, Hocwald, E, Biron, A, Eliashar, R. Nonsurgical management of parapharyngeal space infections: A prospective study. Laryngoscope. 2002;112:906.
35. Wang, D, et al. Lemierre’s syndrome with septic shock caused by Fusobacterium necrophorum. Anaesth Intensive Care. 2007;35:796.
36. Rosenfeld, RM, et al. Clinical practice guideline: Adult sinusitis. Otolaryngol Head Neck Surg. 2007;137(Suppl 3):S1.
37. Brook, I. Acute and chronic bacterial sinusitis. Infect Dis Clin North Am. 2007;21:427.
38. Ponikau, JU, Sherris, DA, Kita, H, Kern, EB. Intranasal antifungal treatment in 51 patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2002;110:862.
39. Thrasher, RD, Kingdom, TT. Fungal infections of the head and neck: An update. Otolaryngol Clin North Am. 2003;36:577.
40. Young, J, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet. 2008;371:908.
41. Landsberg, R, et al. Systemic corticosteroids for allergic fungal rhinosinusitis and chronic rhinosinusitis with nasal polyposis: A comparative study. Otolaryngol Head Neck Surg. 2007;136:252.
42. Snow, V, et al. Principles of appropriate antibiotic use for acute sinusitis in adults. Ann Intern Med. 2001;134:495.