UPPER RESPIRATORY DISORDERS
COMMON COLD
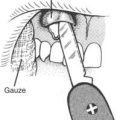
Keep the victim warm and dry. For persons ages 6 years and older, treat nasal congestion with an oral decongestant and nasal spray (use the latter for 3 days maximum). Be aware that an oral decongestant can make a child hyperactive. For an infant, use saline nose drops (¼ tsp, or 1.3 mL, of table salt in 1 cup, or 237 mL, of water) in a dose of two to three drops in each nostril a few times a day; the child will sneeze, or the drops can drain via gravity or be sucked out with a “baby bulb” syringe.
Do not attempt to “sweat out” a cold with vigorous exercise. Such harmful behavior causes worsened fever, debilitation, and dehydration. It is a method guaranteed to convert a common cold into pneumonia. A person with a cold should see a doctor if he is ill for more than 3 weeks, his temperature elevation becomes extreme (see page 167), he develops a cough productive of yellow-green or darkened phlegm (see pages 48 and 205), or he develops chest pain associated with breathing, shaking chills, a severe earache, or a headache with a stiff neck (see page 174). Since colds are spread by contact, take particular care to wash your hands after contact with an infected person.
The most common complication of a cold in a child is a middle ear infection. If a child with a runny nose and cough begins to pull at his ear(s) or if a fever returns near the end of the course of a cold, consider treating the child for otitis media (see page 175). Pneumonia can also be a complication (see page 48). It should be suspected in a child who appears short of breath (respiratory rate above 30 per minute in a child, or 40 per minute in an infant).
INFLUENZA
Elderly or infirm individuals are at greatest risk for becoming severely debilitated or developing complications, such as pneumonia. General therapy is the same as that for a cold: rest, adequate nutrition, increased fluid intake, and medicine for fever. Vaccines are prepared each year that are somewhat effective in the prevention of types A and B influenza (see page 456). Oseltamivir phosphate (Tamiflu) is a drug that is used for treatment of influenza types A and B in adults who have been ill for no more than 2 days. It is given in an adult oral dose of 75 mg twice daily for 5 days. The pediatric dose is based on age and weight. For a child age 1 to 12 years: weight less than 15 kg, 30 mg twice daily for 5 days; 15 to 23 kg, 45 mg twice daily for 5 days; 23 to 40 kg, 60 mg twice daily for 5 days; weight greater than 40 kg or age greater than 12 years, 75 mg twice daily for 5 days. An alternative is zanamivir (Relenza) 10 mg inhaled twice a day for 5 days for all ages.
Avian influenza A (H5N1, which exists in at least 8 subgroups, or “clades”) may be resistant to the adamantane drugs (rimantadine and amantadine), so would be treated with zanamivir or oseltamivir, the former in a dose of 75 mg and the latter in a dose of 150 mg by mouth twice a day for 10 days. This form of influenza is carried and spread by birds, notably poultry and perhaps wild birds. It has been found in other species, such as cats, tigers, leopards, pigs, ferrets, rabbits, rats, and emus, from where it might more rapidly mutate to a form more infectious to humans. Avian flu has a very aggressive profile, with a high (up to 60%) overall mortality rate in human victims. Infected humans show “typical” flu symptoms, followed rapidly by respiratory and multiorgan failure. There is little evidence for mild or asymptomatic human infections. With regard to protective masks, an N95 respirator mask is supposed to have at least a 95% filtration capability at filtering a 0.3 micron droplet, which carries the virus, but not the virus particles individually.
BRONCHITIS
Treatment is controversial, since in the absence of a documented infection, no particular therapy has been shown to shorten the duration of bronchitis. If a persistent (more than 10 to 14 days) infection is suspected, therapy may include administration of an oral antibiotic (first choice azithromycin, levofloxacin, or amoxicillin-clavulanate; others include moxifloxacin, amoxicillin, trimethoprim-sulfamethoxazole, doxycycline, cefixime, cefpodixime, cefproxil, or erythromycin). With or without antibiotics, copious fluid intake, inhalation of humidified warm air (taking care to avoid steam burns) in order to loosen secretions and ease coughing, a drug to loosen secretions (e.g., guaifenesin [Mucinex] 600 mg by mouth every 12 hours), and acetaminophen or aspirin (the latter not for children under age 17 years) for fever may diminish symptoms. It is best to allow the victim to cough up secretions; however, if coughing fits become intolerable, a cough medicine (see page 503) may be used. Dextromethorphan is more effective than guaifenesin, which does not control cough. A 7-day course of inhaled or oral corticosteroids may help. If wheezing and shortness of breath are problematic, an inhaled bronchodilator, such as albuterol, may be used. If pneumonia is suspected (see page 48), treat appropriately and seek immediate medical attention.
HAY FEVER
Hay fever (“rose fever,” “catarrh”) is an allergic reaction, often seasonal (hence the term “seasonal allergies”) to dust, animal dander, plant (usually ragweed, sage, trees, and grasses) pollens, or other compounds found in the air. The victim suffers from red, itchy, and watery (from excessive tearing) eyes; swelling of the eyelids; white, ropey mucus discharge from the eyes; a runny nose with large amounts of clear mucus (allergic rhinitis); sneezing; and general misery. In a severe case, a victim may suffer asthma, sinusitis, loss of smell, and fatigue. In most cases, the symptoms can be relieved by taking an antihistamine medication—although some of these have side effects, the most troublesome of which is drowsiness. Antihistamines that cause drowsiness include triprolidine (Actifed), diphenhydramine (Benadryl), and chlorpheniramine (Chlor-Trimeton). Nonsedating antihistamines, such as fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec), cause much less or no drowsiness. A nasal decongestant (such as oxymetazoline [Afrin]) will clear out the nose, but does not halt the allergic reaction. Furthermore, a nasal decongestant should not be used for more than 5 consecutive days, to avoid “rebound” nasal congestion from drug-induced inflammation. An allergy doctor can use skin tests to evaluate a victim for desensitization injections. If allergies are debilitating and a change in environment is impossible, the victim will almost certainly benefit from a tapering dose of prednisone (see page 492). Nasal steroid sprays (such as fluticasone propionate 0.05% [Flonase], budesonide 32 mcg nasal spray [Rhinocort Aqua], or beclomethasone dipropionate [Beconase]) are a method for treating nasal irritation (blockage, runny nose, itching, and sneezing) from allergies, but usually require approximately 3 days of continual use before a beneficial effect is noted. Cromolyn sodium nasal spray (Nasalcrom), as recommended by some allergists, is another useful adjunct. This requires administration of up to four to six doses per day, and it may be 1 to 4 weeks before any benefit is noted.
PLEURITIS
The lining of the lung, or pleura, is two layers of tissue separated by a thin film of lubricating fluid, which allows the lung to expand with a gliding motion when the chest wall moves outward during inhalation. When the pleura is irritated by an infection, most often caused by a virus, the inflammation may allow fluid to accumulate in this space and cause pain with breathing, localized to the area of irritation. The pain is sharp and worsened by a cough or deep breath. The treatment for viral pleuritis is rest and aspirin. Encourage the victim to breathe deeply. If he is weak or has a high fever, suspect deterioration into pneumonia (see page 48).