Chapter 13 Unloading the Patellofemoral Joint for Cartilage Lesions
Introduction
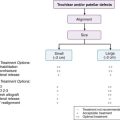
Successful outcomes in patellofemoral cartilage restoration procedures rest on the need to unload the patellofemoral joint. Initial patellofemoral cartilaginous procedures were predisposed to failure because of overload of the patellofemoral compartment or failure to address patellar malalignment. Malalignment is defined as abnormal tilt and or subluxation of the patella,1 and distal realignment (i.e., tibial tubercle osteotomy) is the most definitive method of either realigning a subluxated/tilted patella or offloading the patellofemoral compartment.
Anteromedialization of the tibial tubercle addresses patellar malalignment, patellar arthritis, or is used in conjunction with cartilage restoration procedures. The original technique, as described by Dr. Fulkerson in 1983,2 has been shown in long-term studies to provide long-term relief from instability and patellofemoral pain.3 The idea behind the osteotomy is to alleviate stress from the distal and lateral portions of the patella and trochlea to the proximal and medial patellar articular cartilage.2,4–7 By changing the angle of the osteotomy cut, one can customize the procedure to include more medialization for instability cases or more anteriorization for cartilaginous unloading guidelines. Typically, in most procedures done for cartilage restoration, there is some evidence of patellar malalignment, so a combination of both medialization and anteriorization is chosen.
Indications/Contraindications
Indications for anteromedialization of the tibial tubercle include patellofemoral pain with either lateral or distal patellar arthrosis or lateral subluxation/dislocation of the patella. Other indications include a failed lateral release8 and cartilage restoration procedures that need offloading of the newly regenerated or implanted cartilage cells. The ideal candidate is a patient with lateral patellar tilt (or subluxation) with grade III or IV articular cartilage degeneration localized to the lateral patellar or distal medial patellar facets. Not only should the patient be deemed psychologically mature to undergo the surgical procedure, but he or she should also have failed a course nonoperative management consisting of patellar taping, lateral retinacular mobilization, stretching of the extensor mechanism, bracing, and nonsteroidal anti-inflammatory medication.1,2,7
Preoperative Planning
Physical Examination
Specific tests for the evaluation of the patellofemoral joint include noting patellofemoral crepitance, joint effusion, lower extremity Q-angle, patellar J-sign, lateral retinacular tightness, patellar quadrant mobility, patellar apprehension test, patellar grind test, and stability/pain relief with a lateral to medial force on the patella (i.e., you are simulating holding the patella in an unloaded/reduced position).
Imaging Studies
Imaging studies should start with a complete set of knee x-rays consisting of bilateral anterior-posterior (AP) standing views, bilateral posterior-anterior (PA) 45 degrees; flexed views, a lateral view with the knee in 30 degrees; of knee flexion, and a Merchant view.9
The Merchant view is needed rather than the skyline view because as the knee is hyperflexed in the skyline view, the patella is captured by the bony anatomy of the trochlea, and subtle variations of patellar tilt or subluxation are lost at knee angles greater than 30 degrees;.1
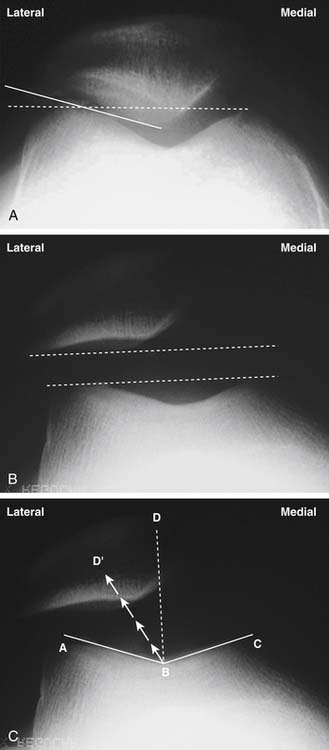
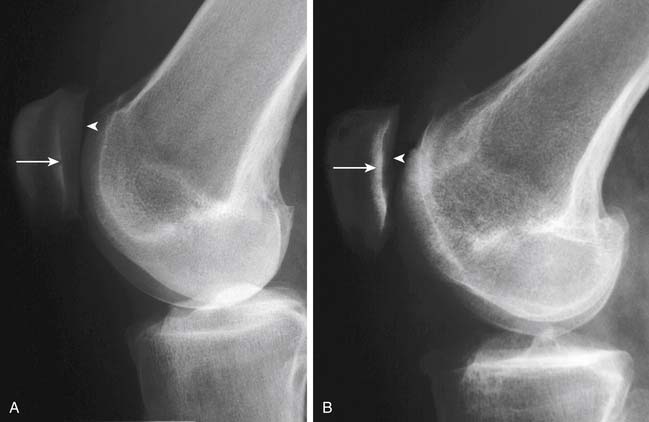
The Merchant view allows the evaluation of patellar tilt (patellofemoral angle of Laurin),10 trochlear dysplasia, and patellar subluxation (congruence angle)9 (Fig. 13-1, A–C). The lateral view allows the evaluation of patellar joint space, trochlear dysplasia, patellar alta/baja, and patellar tilt (Fig. 13-2, A–B). One can also use MRI or CT scans to measure similar angles of patellar subluxation and tilt.3,11–16
Another important measurement for malalignment of the extensor mechanism is the tibial tubercle-trochlear groove (TT-TG) measurement (Fig. 13-3). This relates how far lateral the tibial tubercle is in relation to the central portion of the trochlea.17 Normal TT-TG values are less than 10 mm, and grossly abnormal values are between 18 to 20 mm. The TT-TG can be easily measured on CT or MRI scans and should be thought of as a guide as to how far to move the tubercle during the osteotomy procedure. The final amount of anteromedialization is based on the intraoperative assessment of patellar stability.
Surgical Technique
Holding Area
Any pain blocks can be done at this time by the anesthesia service, although in order to monitor for postoperative function and the possibility of a postoperative compartment syndrome, we do not routinely use nerve blocks for this operation.
Patient Positioning
The patient is brought back to the operating room and placed supine on the operating room table.
For the arthroscopy portion of the procedure, we use a lateral post.
A tourniquet is placed at the upper thigh area, and the lower extremity is prepped and draped in the standard fashion. To avoid capturing the quadriceps with tourniquet inflation and thus altering the normal patellar tracking, the knee is hyperflexed for tourniquet inflation.
Arthroscopy
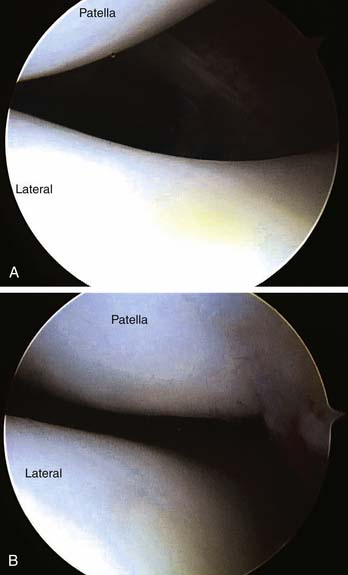
Patellar tilt and subluxation should be documented early in knee flexion (i.e., <15–20 degrees) because at greater knee flexion angles the patella is constrained by the trochlear bony anatomy, thus obscuring the patellar tilt and subluxation (Fig. 13-4, A). The other knee compartments are visualized, and any other concomitant arthroscopic surgery is performed at this time (Fig. 13-4, B).
Incision/Superficial Dissection
The arthroscope is removed but still kept sterile on the field in order to assess the postanteromedialization tibial tracking.
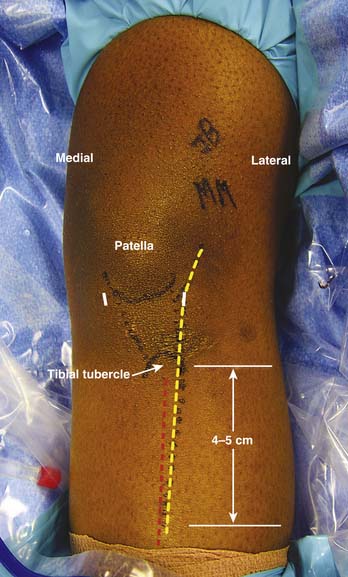
An 8 to 10 cm incision is made incorporating the inferolateral arthroscopy portal proximally and distally extending toward the tibial tubercle. The incision is kept just lateral to the anterior tibial crest to avoid having the incision over the subcutaneous bony skin. In addition, the line of the incision avoids placement of the hardware (tibial fixation screws) directly underneath the skin incision itself (Fig. 13-5). The incision is deepened down to the level of the patellar paratenon and just above the periosteum of the anteromedial tibia.
The medial and lateral borders of the patella are identified, in addition to the tibial tubercle and the anterior tibial muscular compartment.
Lateral Release
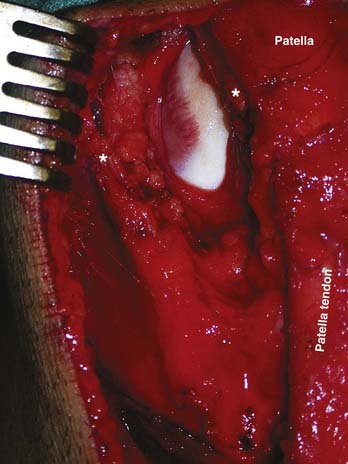
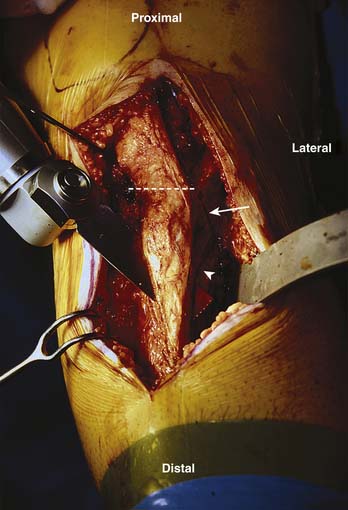
The edges of the lateral release are cauterized to avoid a postoperative hematoma. Distally, the release is taken down to the level of the tibial tubercle, staying lateral to the patellar tendon (Fig. 13-6).
Deep Dissection
The medial border of the patellar tendon is identified at the level of the tibial tubercle, and a hemostat is placed behind the patellar tendon. This ensures that the tendon has been freed from the proximal tibia but is still attached to the tibial tubercle (Fig. 13-7). Occasionally there is scar tissue tethering the distal pole of the patella to the fat pad. This should be released, as it could potentially prevent the proper anteromedialization of the patella.
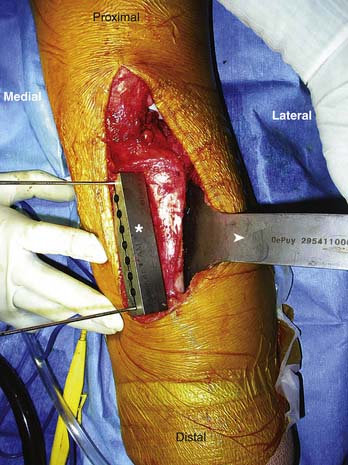
Posteriorly, the muscle is freed down to the posterolateral tibial border and a special retractor (Tracker AMZ Guide System [TRACKER System] Depuy Mitek, Norwood, Mass.) is used to hold the anterior tibial muscle out of the way (Fig. 13-8).
The osteotomy cut is not only an oblique cut when looking at the tibia in the axial plane, but it also tapers distally toward the tibial crest in the coronal plane (Fig. 13-8).
Osteotomy
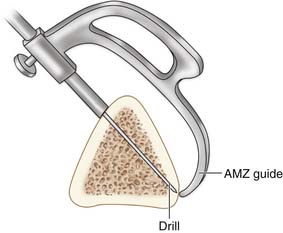
The preferred instrument system, the TRACKER System, was developed by Dr. Jack Farr and is a simple, reproducible way of performing the osteotomy.
The TRACKER System cutting block is fashioned on the anteromedial tibial cortex along the line marked on the periosteum. The cutting block should taper from proximal to distal (Fig. 13-8).
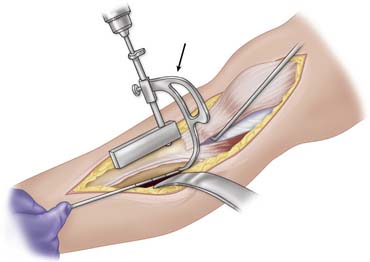
The TRACKER System tracker guide is then inserted into the second or third drill hole from the top of the TRACKER System cutting block. The tracker guide helps one to visualize where the osteotomy will exit along the posterolateral tibia (Fig. 13-9). It is imperative that the osteotomy not exit the posterior tibial cortex.
The angle of the osteotomy cut is now chosen. As previously stated, the steeper the cut, the more anteriorization you will have. Usually the goal is to have the osteotomy exit just anterior to the posterior lateral cortical surface, just before the flare of the metaphysis (Fig. 13-10).
The cutting block is held using two pins that are predrilled. The distal pin should just skirt the anterior tibial cortex to allow for the distal taper of the osteotomy.
A sagittal saw is used to begin the osteotomy cut (Fig. 13-11). The osteotomy is started anteromedially on the tibial cortex, and it exits posterolaterally. As the osteotomy nears the proximal lateral junction between the tibial diaphysis and metaphysis (i.e., metaphyseal flare), care should be taken to avoid penetration of the posterior tibial cortex.

FIGURE 13-11 With the cutting block held in place, a sagittal saw is used to begin the osteotomy cut.
(Reprinted from Operative Techniques in Orthopaedics, vol. 17, issue 4, James Bicos and John P. Fulkerson, Indications and Technique of Distal Tibial Tubercle Anteromedialization, p. 228. Copyright 2007, with permission from Elsevier.)
At this area (i.e., under the tibial tubercle), the saw blade cut should be entirely within the bone. The lateral extent of the cut at this proximal location should be just lateral to the tibial tubercle. Distally, the last 1 to 2 mm of tibial crest bone is left intact (hinging on the periosteum) to create a hinge on which to rotate the osteotomy.
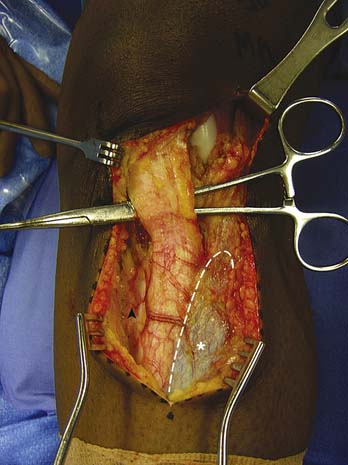
The cutting block is now removed and the anteromedial tibial crest cut is carried more proximally with the saw to clear the medial attachment of the patellar tendon on the tibial tubercle. A 1-inch osteotome is used to make a back cut, starting from the most proximal location of the posterolateral tibial cut (i.e., at the metaphyseal/diaphyseal flare) proximally and anteriorly to just above the patellar tendon attachment on the lateral tibial tubercle (Fig. 13-12). A half-inch osteotome is used to make the back cut underneath the patellar tendon from lateral to medial. This should be done just proximal to the patellar tendon.
Tubercle Fixation
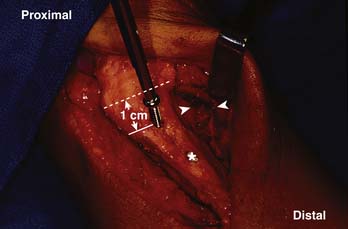
With the osteotomy hinged distally, the proximal portion is anteromedialized along the slope of the osteotomy cut to the desired location. This location depends on your preoperative plan, but typically a 1-cm medialization is created (Fig. 13-13).
The osteotomy is held in place with two 3.2-mm drill bits placed in an anterior to posterior direction just medial to the tibial crest on the osteotomy and starting 1 cm distal to the attachment of the patellar tendon on the tibial tubercle (Fig. 13-13).
The arthroscope is now reinserted, and the knee is taken through a range of motion to document the proper patellar tracking and the anatomic lateral to medial engagement of the trochlea. Any medial subluxation of the patella should be corrected by decreasing the medialization of the osteotomy cut and replacing the 3.2-mm drill bits with screws.
Using proper lag screw technique, two anterior to posterior 4.5-mm fully threaded cortical screws are placed in the proper fashion. They should be countersunk below the anterior tibial cortex of the osteotomy wedge to minimize the postoperative irritation of the hardware on the subcutaneous tissues. Not only should the depth measurement of the screws be made after the countersink bore is done, but the more proximal screw (i.e., the first screw placed) should be downsized 2 mm from its depth gauge reading to allow for the compression of the osteotomy site with the lag screw technique.
Once the necessary cartilage procedure is done, the wedge is brought back down to its predetermined location and the screws are reinserted. This minimizes the need for any drilling to be done after the cartilage procedure, which can jeopardize the cartilage repair. While the osteotomy wedge is retracted proximally, it should be wrapped in a moist sponge (Fig. 13-14).
Closure
Key areas to look for hemorrhage include the anterior tibial muscular compartment or posterolateral tibia (i.e., anterior tibial artery) and the lateral retinacular release (i.e., proximal lateral geniculate artery). The wound is irrigated and a drain is placed deep to the anterior tibial muscular compartment, exiting proximal lateral to the skin incision.
Postoperative Course
The therapist also works on active knee flexion exercises to 90 degrees (or the parameters set intraoperatively) and passive knee extension. Usually for patellofemoral cartilage procedures, knee motion is not started for 6 hours postoperatively and is limited to passive knee flexion of 30 degrees. No straight leg raises are permitted.
Rehabilitation
The rehabilitation protocol can be found in Box 13-1. Important concepts about the rehabilitation protocol can be divided into weight-bearing status and range-of-motion goals.
BOX 13-1 Distal Realignment Rehabilitation
Reprinted from Operative Techniques in Orthopaedics, Vol 17, Issue 4, James Bicos and John P. Fulkerson, Indications and Technique of Distal Tibial Tubercle Anteromedialization, page 228, Copyright 2007, with permission from Elsevier.
Complications
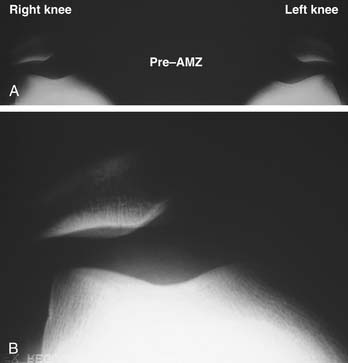
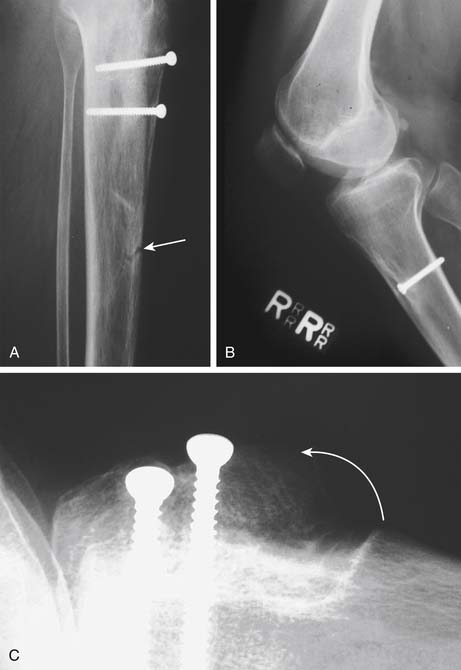
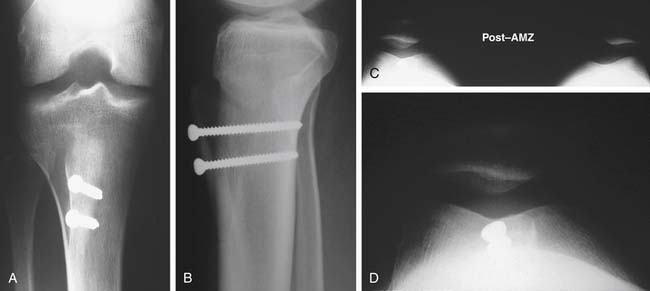
FIGURE 13-16 A, Bilateral patellar tilt and subluxation seen on Merchant view. B, Close-up view of right knee preosteotomy.
(Reprinted from Operative Techniques in Orthopaedics, vol. 17, issue 4, James Bicos and John P. Fulkerson, Indications and Technique of Distal Tibial Tubercle Anteromedialization, p. 230. Copyright 2007, with permission from Elsevier.)
Illustrative Case
Figure 13-16, (A and B) show a 23-year-old male with a long-standing history of patellar dislocations (>15–20 in each knee) who failed a conservative course of treatment consisting of physical therapy, bracing, and activity modification. Patellar taping helped stabilize his patellae, but this was unacceptable to him as a long-term solution to the dislocations. Preoperative Merchant views show bilateral patellar subluxation and tilt. An intraoperative arthroscopy image is shown in Figure 13-4, A. He subsequently underwent an anteromedialization of the tibial tubercle with anatomic alignment of his patella (Figs. 13-4, B and 13-7, A–D).
1. Fulkerson J. Disorders of the patellofemoral joint, 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2004.
2. Fulkerson J.P., Anteromedialization of the tibial tuberosity for patellofemoral malalignment Clin Orthop Relat Res 1983(177):176-181.
3. Post W.R., Fulkerson J.P. Distal realignment of the patellofemoral joint. Indications, effects, results, and recommendations. Orthop Clin North Am. 1992;23(4):631-643.
4. Farr J., Schepsis A., Cole B., Fulkerson J., Lewis P. Anteromedialization: review and technique. J Knee Surg. 2007;20(2):120-128.
5. Schepsis A.A., Wagner C., Leach R.E. Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. Am J Sports Med. 1994;22(5):611-619.
6. Shea K.P., Fulkerson J.P. Preoperative computed tomography scanning and arthroscopy in predicting outcome after lateral retinacular release. Arthroscopy. 1992;8(3):327-334.
7. Fulkerson J.P., Becker G.J., Meaney J.A., Miranda M., Folcik M.A. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18(5):490-496. discussion 496-7
8. Fulkerson J.P. Anteromedial tibial tubercle transfer. In: Jackson D.W., editor. Master techniques in orthopaedic surgery: reconstructive knee surgery. Philadelphia: Lippincott Williams & Wilkins; 2003:13-25.
9. Merchant A.C., Mercer R.L., Jacobsen R.H., Cool C.R. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56(7):1391-1396.
10. Laurin C.A., Dussault R., Levesque H.P., The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation Clin Orthop Relat Res 1979(144) Oct;:16-26.
11. Cohen Z.A., Henry J.H., McCarthy D.M., Mow V.C., Ateshian G.A. Computer simulations of patellofemoral joint surgery. Patient-specific models for tuberosity transfer. Am J Sports Med. 2003;31(1):87-98.
12. Jones R.B., Barlett E.C., Vainright J.R., Carroll R.G. CT determination of tibial tubercle lateralization in patients presenting with anterior knee pain. Skeletal Radiol. 1995;24(7):505-509.
13. Muneta T., Yamamoto H., Ishibashi T., Asahina S., Furuya K. Computerized tomographic analysis of tibial tubercle position in the painful female patellofemoral joint. Am J Sports Med. 1994;22(1):67-71.
14. Guzzanti V., Gigante A., Di Lazzaro A., Fabbriciani C. Patellofemoral malalignment in adolescents. Computerized tomographic assessment with or without quadriceps contraction. Am J Sports Med. 1994;22(1):55-60.
15. Schutzer S.F., Ramsby G.R., Fulkerson J.P., The evaluation of patellofemoral pain using computerized tomography. A preliminary study Clin Orthop Relat Res 1986(204):286-293.
16. Schutzer S.F., Ramsby G.R., Fulkerson J.P. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am. 1986 Apr;17(2):235-248.
17. Goutallier D., Bernageau J., Lecudonnec B. The measurement of the tibial tuberosity. Patella groove distance technique and results. Rev Chir Orthop Reparatrice Appar Mot. 1978;64:423-428.
18. Kline A.J., Gonzales J., Beach W.R., Miller M.D. Vascular risk associated with bicortical tibial drilling during anteromedial tibial tubercle transfer. Am J Orthop. 2006;35(1):30-32.