Chapter 12 Unloading Osteotomies
Effect on Cartilage and Cartilage Repair
Introduction
Good clinical short- and mid-term results have been reported.1–8 However, favorable results seem to be strongly dependent on a precise correction of the loading axis.9 Under-correction with persisting varus usually leads to poor results; overcorrection into large valgus may result in medial joint opening and rapid development of lateral osteoarthritis.10 Various recommendations on the precise amount of the valgus alignment achieved postoperatively have been published. Some authors refer to the anatomical axes of the femur and tibia and recommend a postoperative alignment of 8 to 10 degrees valgus.1–14 Others focus on the mechanical axes of the femur and tibia and suggest a postoperative alignment of 3 to 5 degrees valgus.5,10,15,16 However, these suggestions are based on individual clinical experiences and a few retrospective studies.
Probably the most commonly applied concept in preoperative planning is based on the work of Fujisawa et al.14 In this retrospective clinical study, preoperative and postoperative arthroscopy with a follow-up for 4 months to 6 years was performed on 54 knee joints before closing-wedge HTO, and the tibiofemoral joint cartilage was evaluated. The postoperative weight-bearing axis was correlated with changes in cartilage findings. The correction achieved postoperatively was measured with reference to the intersection of the weight-bearing axis with the tibial plateau. The tibial plateau was divided into four sections and the point of intersection assigned to the corresponding section. Fujisawa et al.14 concluded from their findings that for ideal correction the postoperative axis should lie within the lateral 30% of the tibial plateau as measured from its midpoint. From this study derived the recommendation that the weight-bearing axis should postoperatively pass through the “Fujisawa point” (i.e., it should intersect with the knee joint line at 62% of the tibial plateau width measured from its medial cortex).17–19
Effect of Different Load Axes on Tibiofemoral Cartilage
Literature
Before direct measurement of joint cartilage pressure was technically feasible, indirect methods were employed based on evaluation of radiographs, eventually combined with gait analysis and measurements of ground reaction forces with force plates.20–22
The first direct measurements of transferred joint forces and contact pressures were obtained by application of strain gauges.23,24 Next, pressure-sensitive films (Fuji film) were used that changed color as a result of applied pressure.25,26
The up-to-date techniques use pressure-sensitive film that measures changes in electromechanical resistance (K-Scan System, Tekscan, Inc., Boston, Mass.). These sensors offer the highest accuracy and best reproducibility and have provided the basis for the most recent studies on this subject.27
Most studies are tested under static conditions and rarely under dynamic conditions (i.e., simulation of gait cycle with an increase and decrease in loading). Nevertheless, all the studies were basically able to demonstrate that alterations of the axial alignment led to redistribution of load within the compartments of the tibiofemoral joint. Varus deformity resulted in greater loading of the medial compartment and valgus deformity in greater loading of the lateral compartment. This inequality in the distribution increased with the degree of axis deviation, proximity to the joint line, and amount of applied force.24,25
In addition to those studies describing tibiofemoral pressure distribution under the influence of different load axes in the frontal plane, only two experimental studies have been published that investigated the effect of high-tibial-correction osteotomy on contact pressures distributions within the knee joint. Only one of these studies was concerned with the correction of deformities in the frontal plane (valgus-varus)26; using the closing-wedge technique. The other study, published by the present author, investigated contact pressure changes after correction osteotomy in the sagittal plane.27 Measurements of the contact pressure in the knee joint after correction osteotomy in the varus-valgus plane in open-wedge technique have not been published so far. Furthermore, data correlating the degree of valgus with the desired changes in intraarticular contact pressure distribution are currently not available.
In a biomechanical study with knee joint specimens, Riegger-Krugh et al.25 investigated the effect of HTO in closing-wedge technique on the contact pressure distribution within the tibiofemoral joint. Fuji films were used for pressure measurement (i.e., only measurement under static conditions were possible and there were no repeated measurements). Both varus and valgus malalignments were simulated and a closing-wedge osteotomy of 5 degrees was carried out. The authors found differences in contact pressure distribution as expected, with higher contact pressure in the medial compartment in varus malalignment and higher contact pressure in the lateral compartment in valgus malalignment. Surprisingly, with a neutral loading axis, less contact pressure was recorded in the medial compartments than in the lateral compartments under these test conditions; after valgus HTO, the contact pressure distribution was similar to that with neutral loading axis. The authors concluded that because of those only minimal changes in the contact pressure distribution, an HTO of 5 degrees would represent in most patients an under-correction.
In a biomechanical study conducted by the authors,27 tibiofemoral contact pressure was measured after flexion HTO (i.e., after altering the mechanical axes in the sagittal plane). In a dynamic experimental model involving a knee joint kinemator, contact pressure was measured with the K-Scan System. Flexion osteotomy was performed as a supra tuberositous opening-wedge osteotomy parallel to the tibial slope of the tibial plateau, and then the tibial slope was gradually increased in 5 degrees increments from its original position to 20 degrees. This osteotomy exclusively modified the alignment in the sagittal plane; the alignment in the frontal plane (varus-valgus) was left unchanged.
Experimental Study of the Authors
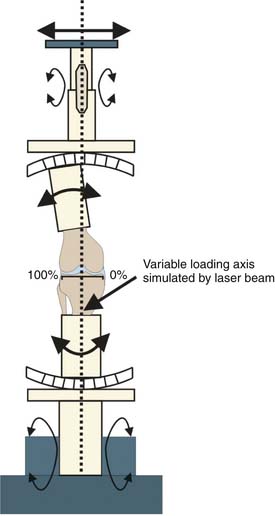
The authors conducted an experimental study to investigate the effect of different loading axes in the frontal plane on the tibiofemoral cartilage pressure.19 Seven knee joints were tested in full extension under axial loading according to a standardized loading protocol (peak load 1000 N) in a materials testing system (MTS 858 Mini Bionix II test system, Eden Prairie, Minn.). Different loading situations of the lower leg were simulated by varying the anatomical alignment angles of the distal femur and the proximal tibia as well as the offset created by the femoral head using a specially designed and constructed fixture. The fixture was allowed to compensate for different preexisting anatomical femoral and tibial angles, and a standardized and reproducible intersection between the mechanical loading axis the knee joint line was set up for each testing. The distal end of the tibia and the proximal end of the femur were potted in cylinders attached to universal joints, which allowed frontal- and sagittal-plane movement but constrained axial rotation.
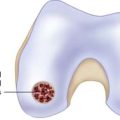
The knee joint line was measured as the width of the tibial plateau and divided into percentages along its length beginning from the medial margin of the cortex (Fig. 12-1).
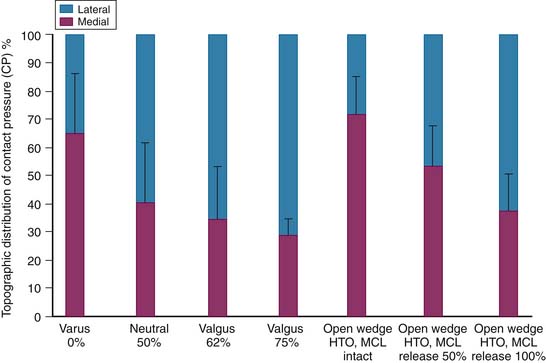
Accurate positioning of the load line was determined by a vertical laser beam translating the frontal plane rotation axes of the proximal and distal universal joints (Fig. 12-2). Zero percent varus alignment was defined as an offset of 0% of the width of the tibia plateau from the medial margin. Other axial alignments then tested were at 25%, 50% (neutral axis), 62% (Fujisawa point), and 75%. Subsequently, an intraligamentous opening-wedge HTO was performed in standard technique with medial approach (discussed later). The opening was standardized at 9 mm, the medial collateral ligament initially left intact, and the load axis again adjusted to 62%. Finally, the distal superficial part of the medial collateral ligament bridging the osteotomy was dissected from anterior to posterior in two stages.
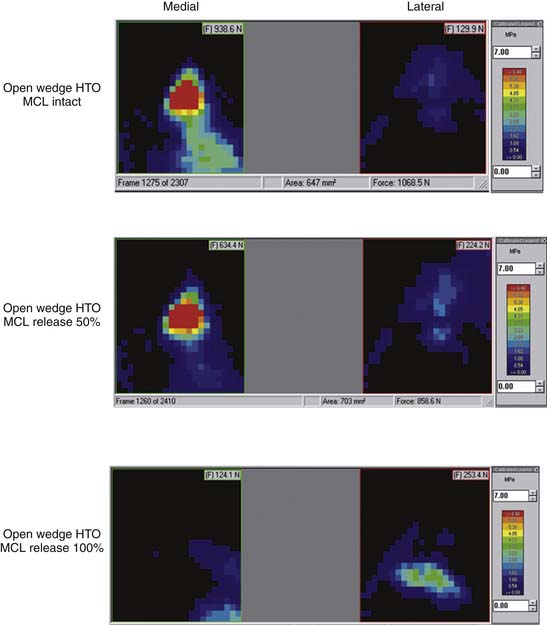
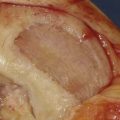
The pressure measurements were performed using pressure-sensitive films (K-Scan 4000) and contact force (N), contact area (mm2), and contact pressure (MPa), as well as the topographical pressure distribution between the medial and lateral tibiofemoral joint were continuously recorded during the load cycle in every testing (Figs. 12-3 through 12-6).
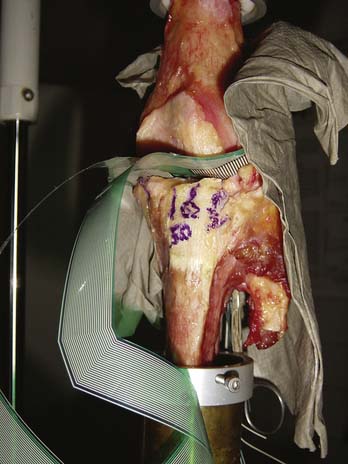
FIGURE 12-4 Several loading axes were simulated: varus (0%), neutral (50%), valgus (62%), and valgus (75%).

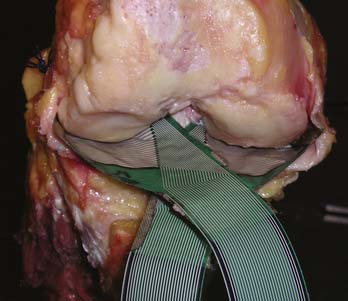
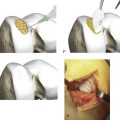
FIGURE 12-5 The valgus osteotomy was performed in an opening wedge technique from medial in a biplanar fashion.
The contact pressure distribution between the medial and lateral joint compartments was shown to be clearly dependent on the different load axes. For varus deformity, about 65% of the total pressure was measured in the medial compartment and 35% in the lateral compartment (Fig. 12-7). The more laterally the load axis was shifted, the lower were the percentages for contact pressure recorded medially and the higher the lateral percentages. Surprisingly, after medial, open-wedge osteotomy with intact medial collateral ligament under a loading of 1000 N the medial percentage of contact force was considerably higher than laterally (71.4% versus 28.6%), although the load axis was in a slightly valgus position at 62% of the width of the tibial plateau. Measurement with the same mechanical loading axis (62%) without osteotomy had produced a reverse and predicted pattern of contact pressure distribution (i.e., medial contact pressure was clearly lower than lateral contact pressure). Thus, the aim of decompressing the cartilage in the medial joint compartment was not achieved by osteotomy, but instead the contact pressure was even slightly increased despite a valgus instead of a varus malalignment (0%). Even without axial loading, a certain amount of contact pressure was measured in the medial compartment with an open HTO and intact medial collateral ligament. Only after step-by-step dissection of the superficial distal portion of the medial collateral ligament was medial contact pressure reduced and the lateral contact pressure increased, reaching values that were previously recorded in the 62% position without osteotomy (Fig. 12-8). Medial decompression compared to original simulated varus alignment was also achieved.
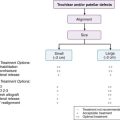
Indication for High Tibial Osteotomy of the Knee
The patient should not be older than 65 to 70 years although this is not a hard criterion. The patient should not be severely overweight, and the range-of-motion should be at least 0/0/120°. Flexion contracture may be accepted if a saggital correction of the tibial slope is included in the surgical plan. Open-wedge osteotomy should not be used if leg lengthening is contraindicated and if the medial soft tissue coverage is compromised. Patella pain is not a contraindication; however, in cases with patella baja, a special type of osteotomy described later should be used. An intact lateral compartment of the knee is an obligatory prerequisite for this technique. The patient should not have lateral joint line pain, and no radiographic signs of lateral osteoarthritis should be present.
Type of Deformity and Preoperative Planning
One of the most important factors for the success of an osteotomy is the preoperative analysis of the deformity and the planning of the correction. This means that the location and the amount of the malalignment have to be investigated in a bipodal standing long leg x-ray. According to the recommendations of Paley,17 the respective angles between the mechanical axes of the femur and tibia and the joint line (mechanical medial proximal tibial angle mMPTA and mechanical lateral distal femoral angle [mLDFA]) have to be measured. A varus deformity in the tibia means that the mMPTA is less than 87 degrees; a valgus in the distal femur by definition is a result of an mLDFA less than 87 degrees.
Operative Technique
The principles of deformity correction as formulated by Paley17 should be generally respected.
For this reason, the authors’ preferred method of valgus osteotomy of the proximal tibia is the medial opening wedge technique (Fig. 12-9, A-C).
The medial collateral ligament running across the osteotomy (discussed earlier) has to be released distally from the tibia to avoid ligament related overcompression in the medial compartment after opening of the wedge. An adjustable spreader is used in the posterior part of the osteotomy to keep the gap open. The spreader can be inserted as desired anteriorly or posteriorly in the osteotomy gap and the tibial slope thus directly be accustomed, which can additionally be monitored on the fluoroscope.
Stability of the osteosynthesis after high tibial osteotomy is crucial for the outcome. It is not only important for quick and functional postoperative rehabilitation with immediate postoperative partial weight bearing but for safe healing of the osteotomy without any loss of the performed correction. Spacer plates designed by Puddu can be used to keep the osteotomy open and serve as osteosynthesis. However, they offer only minimal stability in cases of larger corrections as they cannot adequately eliminate the tremendous lever arm forces created by the quadriceps and the distal tibia. Probably this is why the authors and others have seen implant failures and nonunions in some (especially tall or obese) patients where the spacer implants were used. Therefore, in cases of larger openings (>10 mm), in tall or obese patients or in patients with minor bone stock quality, another more stable implant should be used for osteosynthesis. TomoFix (Synthes, West Chester, Pa.) is a specially designed rigid plate that serves as an internal plate fixator (Figs. 12-10 through 12-12, A-E). Angle-stabilized locking bolts, which can be positioned percutaneously, completely eliminate wobbling of the bolts within the plate, thus largely enhancing the stability of the osteosynthesis. In the case of fractures of the lateral cortex, which frequently occur in openings of more than 12 mm, a lag screw can be applied. This screw is inserted in the first plate hole distal to the osteotomy, and after fixation of the plate it is proximally advanced in a posterolateral direction. By doing so, reapproximation of the lateral cortical edges of the osteotomy can be achieved. Altogether nine locking bolts are used with the TomoFix device, with three bolts proximal and four distal to the osteotomy.
1. Coventry M.B. Osteotomy about the knee for degenerative and rheumatoid arthritis. J Bone Joint Surg Am. 1973 Jan;55(1):23-48.
2. Coventry M.B. Upper tibial osteotomy for gonarthrosis. The evolution of the operation in the last 18 years and long term results. Orthop Clin North Am. 1979;10(1):191-210.
3. Coventry M.B. Proximal tibial osteotomy. Orthop Rev. 1988;17(5):456-458.
4. Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003;11(3):132-138.
5. Lootvoet L., Massinon A., Rossillon R., et al. [Upper tibial osteotomy for gonarthrosis in genu varum. Apropos of a series of 193 cases reviewed 6 to 10 years later]. Rev Chir Orthop Reparatrice Appar Mot. 1993;79(5):375-384.
6. Hernigou P., Medevielle D., Debeyre J., et al. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69(3):332-354.
7. Odenbring S., Egund N., Knutson K., et al. Revision after osteotomy for gonarthrosis. A 10-19-year follow-up of 314 cases. Acta Orthop Scand. 1990;61(2):128-130.
8. Dugdale T.W., Noyes F.R., Styer D., Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length Clin Orthop Relat Res. 1992(274) Jan;:248-264.
9. Goutallier D., Hernigou P., Medevielle D., et al. [Outcome at more than 10 years of 93 tibial osteotomies for internal arthritis in genu varum (or the predominant influence of the frontal angular correction)]. Rev Chir Orthop Reparatrice Appar Mot. 1986;72(2):101-113.
10. Engel G.M., Lippert F.G.3rd. Valgus tibial osteotomy: avoiding the pitfalls. Clin Orthop Relat Res. 1981 Oct;160:137-143.
11. Kettelkamp D.B., Wenger D.R., Chao E.Y., et al. Results of proximal tibial osteotomy. The effects of tibiofemoral angle, stance-phase flexion-extension, and medial-plateau force. J Bone Joint Surg Am. 1976 Oct;58(7):952-960.
12. Koshino T.T., Morii T., Wada J., et al. High tibial osteotomy with fixation by a blade plate for medial compartment osteoarthritis of the knee. Orthop Clin North Am. 1989 Apr;20(2):227-243.
13. Hernigou P., Ovadia H., Goutallier D. [Mathematical modelling of open-wedge tibial osteotomy and correction tables]. Rev Chir Orthop Reparatrice Appar Mot. 1992;78(4):258-263.
14. Fujisawa Y., Masuhara K., Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10(3):585-608.
15. Miniaci A., Ballmer F.T., Ballmer P.M., et al, Proximal tibial osteotomy. A new fixation device Clin Orthop Relat Res 1989(246) Sep;:250-259.
16. Noyes F.R., Barber S.D., Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees. A two- to seven-year follow-up study. Am J Sports Med. 1993;21(1):2-12.
17. Paley D. Principles of Deformity Correction. Berlini: Springer Verlag; 2002.
18. Stukenborg-Colsman C., Ostermeier S., Hurschler C., et al. Tibiofemoral contact stress after total knee arthroplasty: comparison of fixed and mobile-bearing inlay designs. Acta Orthop Scand. 2002;73(6):638-646.
19. Agneskirchner J.D., Hurschler C., Stukenborg-Colsman C., et al. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124(9):575-584. Epub 2004 Aug 03
20. Lobenhoffer P., De Simoni C., Staubli A.E. Open wedge high-tibial osteotomy with rigid plate fixation. Techniques in Knee Surgery. 2002;1(2):93-105.
21. Agneskirchner J.D., Freiling D., Hurschler C., et al. Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):291-300. Epub 2005 Nov 12
22. Lobenhoffer P., Agneskirchner J., Zoch W. [Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator]. Orthopade. 2004;33(2):153-160.
23. Lobenhoffer P., Agneskirchner J., Zoch W. Open-wedge high tibial osteotomy with special medial plate fixator. Orthopade. 2004;33(2):153-160.
24. McKellop H.A., Sigholm G., Redfern F.C., et al. The effect of simulated fracture-angulations of the tibia on cartilage pressures in the knee joint. J Bone Joint Surg Am. 1991;73(9):1382-1391.
25. Riegger-Krugh C., Gerhart T.N., Powers W.R., et al, Tibiofemoral contact pressures in degenerative joint disease Clin Orthop Relat Res 1998(348) Mar;:233-245.
26. Bachus K.N., DeMarco A.L., Judd K.T., et al. Measuring contact area, force, and pressure for bioengineering applications: using Fuji Film and TekScan systems. Med Eng Phys. 2006;28(5):483-488. Epub 2005 Sep 21
27. Shelburne K.B., Torry M.R., Pandy M.G. Contributions of muscles, ligaments, and the ground-reaction force to tibiofemoral joint loading during normal gait. J Orthop Res. 2006;24(10):1983-1990.