CHAPTER 1 Uni
History and Look to the Future
 The early clinical results with unicondylar implants often included results in which the implants were used to replace the tibio femoral compartments of both condyles with independent components.
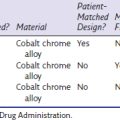
The early clinical results with unicondylar implants often included results in which the implants were used to replace the tibio femoral compartments of both condyles with independent components. The use of polyethylene less than 6 mm thick and without metal backing accounted for early failures with the Marmor implant. The FDA now requires a minimum thickness for polyethylene of greater than 6 mm.
The use of polyethylene less than 6 mm thick and without metal backing accounted for early failures with the Marmor implant. The FDA now requires a minimum thickness for polyethylene of greater than 6 mm. Factors that led to higher failure rates of unicondylar implants included younger age, male gender, and most importantly gamma-in-air sterilization. A prolonged shelf age led to oxidative degradation of the tibial polyethylene.
Factors that led to higher failure rates of unicondylar implants included younger age, male gender, and most importantly gamma-in-air sterilization. A prolonged shelf age led to oxidative degradation of the tibial polyethylene.Early Clinical Experience with Unicondylar Implants
The earliest nonlinked implants for the management of gonarthrosis were mostly unicompartmental implants often used to replace both the tibial and femoral compartments of the knee. The Polycentric knee was described in 1971 as an implant to restore normal knee movement.1 The probability of success of the first 209 Polycentric implants performed at the Mayo Clinic between July 1970 and November 1971 was 66% at 10 years.2 Results were similar when this implant was used for single-compartment replacement.3 These devices, which were single-radius femoral components, were subsequently abandoned for treating arthritis in both single and bicompartmental arthritis of the knee.
During the same time interval, surgeons were having early clinical success when using the Marmor (Richards, Memphis, TN) knee as a unicompartmental implant. The clinical results, however, did not appear in the literature in a timely fashion. In 1981, Scott and Santore reported early encouraging results with only three revisions in the first 100 patients with a different unicondylar implant.4 Unfortunately, these early encouraging results were overshadowed by inferior results reported by others. In 1976, Insall and Walker had already reported a high failure rate in 19 knees with medial unicompartmental implants of a different design.5 The authors had satisfactory outcomes with 5 lateral unicondylar arthroplasties and related that the use of unicondylar implants in the future may only be indicated for such deformities. In a subsequent report involving many of the same patients, Insall and Aglietti reported 7 conversions to another knee prosthesis and 14 fair or poor results from a group of 22 knees.6 This implant had a coronal curved-on-curved design, and 12 of the 22 cases underwent a concomitant patellectomy. Likewise, Laskin experienced and reported discouraging results in 37 patients with unicondylar implants because of recurrent pain, prosthetic settling, and progression of arthritis.7
Oxford meniscal-bearing implants were introduced a decade after traditional fixed-bearing unicondylar implants. The earliest clinical results were reported in 1986 by Goodfellow and O’Connor on 125 cases with 2- to 6-year follow-up.8 These early cases also were bicompartmental replacements with unicondylar implants similar to the earliest cases with fixed-bearing unicondylar implants. The early revision rate was 4.8% for knees that had intact anterior cruciate ligaments (ACLs). The survivorship for all osteoarthritis knees was 83% at 6 years. In a subsequent study of 301 knees followed as long as 9 years, Goodfellow and O’Connor further emphasized the need to have an intact ACL with meniscal-bearing implants.9 Knees in which the ACL was damaged or absent had a survival rate of only 81% at 6 years. Two hundred five of the 301 cases were bicompartmental arthroplasties. In comparison, Murray et al. reported the outcome of 143 medial unicompartmental arthroplasties in which the Oxford implant was used in knees with an intact ACL.10 In this 1998 report, the survival rate of the implants used as unicompartmental replacements was 98% at 10 years.
Swedish Knee Arthroplasty Register—Early Reports
The Swedish Knee Arthroplasty Register, initiated in 1981, has provided invaluable information as it relates to the outcome of knee arthroplasty surgery and insight into some of the problems that impacted the clinical results. Knutson et al. reported the results of a nationwide survey of over 30,000 knees operated on between 1976 and 1992.11 Total knee components showed gradually improving survival, whereas unicompartmental prostheses did not. The authors reported that this was partly because of newly introduced inferior unicondylar designs that had high failure rates. A survey was mailed to all living patients in the Registry who were operated on between 1981 and 1995 to address the issues of reoperation and patient satisfaction.12 Ninety-five percent of patients answered this survey. Eight percent of patients were dissatisfied. When revision was necessary, the proportion of satisfied patients was higher among patients who underwent a medial unicompartmental knee arthroplasty (UKA) revision than for patients revised following a failed total knee arthroplasty (TKA). Another review of Swedish register data compared the outcome for 699 Oxford (Biomet, Bridgend, UK) UKAs to a matched group of Marmor (Smith & Nephew Richards, Orthez, France) UKAs for unicompartmental arthroplasty.13 After 6 years, the revision rate for the Oxford group was more than two times the revision rate of the Marmor group. Meniscal-bearing dislocation and component loosening were the two main reasons for the 50 Oxford revisions in this cohort of patients.
Unicondylar Arthroplasty in the 1990s
Unicondylar implants fell out of favor among most orthopaedic surgeons during the decade of the 1990s. In 1991, Scott et al. reported that bicompartmental arthroplasties with a condylar prosthesis done in the 1970s had a longer survivorship.14 In this study, the survivorship of 100 consecutive UKAs was 85% at 10 years. Kozinn and Scott also reported very strict criteria for unicondylar arthroplasty to include weight less than 180 pounds, noninflammatory arthritis, an intact ACL, and no evidence of degenerative changes greater than grade II in the opposite and patellofemoral compartments.15 The authors felt that strict selection criteria were essential to avoid failures from progression of disease and failures from implant loosening. Using such strict criteria limited the number of surgical candidates for a unicondylar arthroplasty to less than 5%. Proponents of tricompartmental arthroplasty argued that most orthopedic surgeons in the United States do less than 20 knee arthroplasty cases a year. Therefore, they would only have an opportunity to do 1 or 2 unicondylar procedures a year using strict selection criteria and would have difficulty maintaining the necessary technical proficiency for consistently good clinical results. Furthermore, Padgett et al. related that revision surgery for a failed unicondylar implant was not always a simple procedure.16 In this series of 19 revisions, 76% had osseous defects and two cases required re-revision surgery.
A small number of surgeons advocated UKA for unicompartmental disease and continued to report the benefits of a smaller and less invasive surgical procedure in contrast to full knee arthroplasty. Benefits to the knee with a unicondylar implant included: less blood loss, better flexion in the knee, dominant use of the knee on stairs, and a lesser need for ambulatory aids. Also, patients had better pain relief with the UKA and preferred the UKA to the TKA. Such benefits were reported in studies by Cobb et al. comparing 42 patients who had a TKA in 1 knee and a UKA in the other,17 by Rougraff et al. comparing 120 UKAs to 81 TKAs,18 and by Laurencin et al. comparing 23 patients who had a UKA in 1 knee and a TKA in the other knee during a single hospitalization.19 Knutson et al. had reported earlier from the Swedish Knee Arthroplasty Register data a statistically significant reduction in rate of infection by more than 50% with a unicondylar arthroplasty (0.8% with UKA vs. 2% with TKA).20
The use of unicondylar implants remained sparse through the 1990s. Although patient satisfaction remained high, the revision rates remained marginal. Some of these failures were design issues. As an example, the Robert Brigham implant offered a metal-backed nonmodular tibia that was 6 mm thick. The polyethylene was 4 mm thick. The original Marmor implant had an all-polyethylene tibia that was less than 6 mm thick. Such components had high early failure rates and were withdrawn from the market. As early as 1991, Knutson et al. reported that deformation and loosening occurred in one third of the 6-mm-thick unicompartmental implants placed in rheumatoid knees and one fifth of the osteoarthritic knees within 2 years.21 The 6-mm components had a higher loosening rate. The Food and Drug Administration (FDA) subsequently set greater than 6 mm as the minimum allowable thickness for a tibial polyethylene component. Another design error with unicondylar implants was to try to reduce contact stress by creating a significant coronal curvature to both components. Insall and Aglietti’s original experience featured such a configuration.6 The PCA unicondylar device was a curved-on-curved design in a frontal plane somewhat similar to Insall’s original implant. This implant had an unacceptable failure rate as reported in the Norwegian and Finnish knee arthroplasty registries.22 Positioning the two components correctly in the coronal plane to allow full flexion and axial rotation was technically difficult.
Anderson Orthopaedic Research Institute Results
Four hundred eleven medial unicondylar implantations were performed at the Anderson Clinic between 1984 and 1998.23 The implants were of 12 different designs from six different manufacturers. The Kaplan-Meier survivorship with an end point of revision was 80% at 9 years. Rather than abandoning unicondylar arthroplasty at this time because of this unacceptable revision rate, the risk factors for revision were identified and survivorship reexamined using multivariate data analysis to determine the role (if any) for unicondylar arthroplasty in the treatment of isolated unicondylar arthritis. The risk factors examined were patient factors, including age, weight, and gender, and implant variables, including polyethylene thickness, method of sterilization, shelf age of polyethylene, and implant design. Using Cox proportional hazards regression with revision as an end point, three variables were statistically significant; younger age (p < .01), thin polyethylene (p < .01), and shelf age (p < .01). Of the 411 medial unicondylar knees, 152 had a shelf age less than 1 year and polyethylene thickness of at least 8 mm. The survivorship for this subset of patients was 95%. Confidence was restored in this surgical procedure by using polyethylene of adequate thickness without the potential of oxidative degradation.
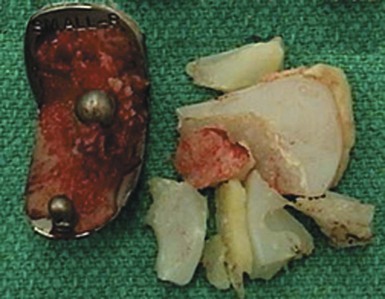
The impact of oxidation on the failure of knee implants is best documented in retrieval studies. The 42 unicondylar implants that were revised at the Anderson Clinic between 1986 and 2000 were cataloged as to reason for revision and then analyzed for wear. Seventy-one percent of the revisions were for polyethylene wear. An analysis of the retrieved components confirmed severe fatigue wear with delamination and in some instances wear-through of polyethylene to the underlying tibial baseplate. No revisions occurred in 42 of the 411 implants that were sterilized by methods other than gamma irradiation in air.23 In another study, Blunn et al. examined 26 retrievals of Marmor unicondylar implants in situ from 1–13 years.24 These nonirradiated tibial polyethylene components showed no delamination. In contrast, Williams et al. in 1998 identified delamination with subsurface white bands characteristic of oxidation in over 80% of gamma-in-air sterilized components.25 In this study, 32 unicondylar implants sterilized by ethylene oxide had no delamination or evidence of oxidation. The impact of shelf age leading to polyethylene oxidation and its impact on survivorship was far greater for unicondylar implants because of infrequent usage of unicondylar implants and the frequent usage and popularity of total knee implants. Implants were manufactured and sterilized in large batches. Depleted inventory was replenished frequently with total knee implants. The shelf age on unicondylar implants at the Anderson Clinic averaged 2.0 ± 1.9 years. This was more than a year longer than total knee implants, which averaged 0.9 ± 1.0 years (AORI Knee Clinic Database). Two studies best demonstrate the impact of shelf age on implant survivorship. In the first study, 100 consecutive SCR (Osteonics, Allendale, NJ) UKA components with an average shelf age of 1.7 years after gamma irradiation in air were divided into two equal groups: shelf age greater than 1.7 versus shelf age less than 1.7 years.26 The survivorship at 6 years was 96% for the shorter shelf-age group versus 71% for the group with the longer shelf age (p < .01). The second study was a review of 75 Duracon (Stryker Osteonics Howmedica, Rutherford, NJ) unicondylar implants (Fig. 1–1).27 Seventy-three of the components had a shelf-age storage of 4.5–6.5 years. Since publication of that study, 65 of the 75 implants were revised in less than 5 years, with all revisions performed for accelerated polyethylene wear.
Unicondylar Implants That Were Successful in the 1990s
Historically, some unicondylar fixed-bearing implants that were performed in the 1980s and 1990s faired well. Squire et al. reported an 84% survivorship at 22 years using revision for any reason with the original Marmor implant with an all-polyethylene tibial component.28 This implant was minimally congruent, and success was probably related to non-gamma sterilization (most early implants were sterilized with ethylene oxide) and precise surgical technique as this was a single senior surgeon experience. Berger et al. reported a 10-year survivorship of 98% for 51 patients with the Miller-Galante implant.29 The method of polyethylene sterilization is not reported. The implant probably had a short shelf age if gamma irradiated in air, as this was the surgeon-designers’ initial clinical experience with this implant. In another study, Pennington et al. reported 98% retained components at a mean follow-up of 11 years with the same Miller-Galante implant in young, active patients (mean age of 54 years).30 Some early studies with mobile bearings were equally promising. Murray et al. reported a 98% survivorship at 10 years with the Oxford mobile-bearing unicondylar knee.31 Again this was a series of cases done by surgeon-designers in a select subset of patients including only knees that had an intact ACL. In addition, better contact stresses made this implant less sensitive to fatigue modes of wear. The benefits of lower contact stress with a mobile-bearing implant probably contributed to the excellent outcome with 124 Oxford implants with a 10- to 15-year survivorship in a study by Svard and Price.32
Although excellent unicondylar results began appearing in the literature, survivorship from other studies and joint registry data continued to favor TKA. Once again, the reader of these reports can either accept this information at face value or take more than a cursory look at the data that led to these conclusions and determine the feasibility for unicondylar arthroplasty for unicondylar disease. As an example, in 2003 Gioe et al. reported the 10-year survivorship for 516 UKAs in comparison with 4654 TKAs from a regional joint registry.33 The survivorship at 10 years was 88.6% for UKAs versus 94.8% for TKAs during the same time interval. Two confounding variables may have dramatically impacted these findings. First, the authors reported that two thirds of the UKAs were sterilized by gamma irradiation in air but the shelf age was not reported. More than likely, the shelf age of the unicondylar implants in this study was significantly longer than the total knee implants. The second variable was the Kirchner implant that was inserted in 34 of the 516 unicondylar cases. This implant alone accounted for 38% (15/39) of the UKA failures in the study. If the 34 Kirschner implants were excluded from the analysis, the revision rate for UKAs would be 5% (24/482); hence 95% of the implants would remain in situ after 10 years. Without the Kirschner UKA in the analysis, the survivorship of UKA implants would be similar to that of the TKA implants in this study.
Minimally Invasive Surgery: An Epiphany for UKA
The popularity and demand for minimally invasive techniques led to the introduction of new unicondylar implants and instruments modified for minimally invasive procedures. Surgeons were learning a new surgical procedure with new instruments and implants but with little or no previous experience with traditional unicondylar surgery. The early clinical results with unicondylar procedures reflect the impact of these variables. In some instances the complications were clearly secondary to the limited surgical exposure. Hamilton et al. reported an increase in new complications and modes of failure not previously reported.34 Wound complications, most likely, were secondary to overzealous soft tissue retraction with small incisions. Retained cement fragments, not encountered with traditional surgical exposures, were secondary to limited surgical exposure to the back of the knee with small incisions. Femoral loosening was probably related to a change in implant design and instrumentation to accommodate implant insertion through a limited surgical approach. As an example in Hamilton et al.’s study, the single femoral peg parallel to the posterior condylar bone cut made implant insertion easier but was not optimal for femoral component fixation. Very thin bone resections were secondary to implant and instrument modifications that did not expose adequate porous bone for optimal cement penetration and contributed to the early femoral loosening. The placement of multiple small drill holes in areas of dense sclerotic bone to allow cement penetration is now advocated to address the problem of early component loosening (Fig. 1–2).
The impact of surgical experience is best reflected in joint registry data. The Swedish Knee Arthroplasty Register reports a more than threefold increase in the revision rate of Oxford unicompartmental knees for institutions that perform fewer than 23 procedures per year.35 This limited experience factor is also evident from other registries. The 2004 Australian Knee Registry report includes a revision rate of 5.9 to 7.4 for implants, with more than 100 revisions per year. The New Zealand registry for implants inserted from 2000 to 2006 documented revision rates from 3.4 to 6.4 for the most commonly used components. In essence, surgeons with little surgical experience with unicondylar arthroplasty were inserting new designs using new instruments modified for minimally invasive techniques. In the United States, where roughly 8% of knee arthroplasty cases are unicondylar implants, a surgeon doing 100 cases a year using traditional indications would perform 7 or 8 TKAs per month but only 1 UKA every other month using traditional indications for this procedure. A still unresolved question is: what volume of cases is essential to maintain adequate technical expertise with a unicondylar surgical technique?
UKA Today: Comparing Apples to Apples
Joint arthroplasty surgeons today must contend with the issue that the raw data from registries substantiates a higher failure rate at both 5 and 10 years with unicondylar arthroplasty procedures. In the Swedish Knee Arthroplasty Register report for 2007, the revision rate for all UKAs at 10 years was 10% as compared to 5% at 10 years for TKAs.36 The 10-year failures somewhat reflect oxidized polyethylene with implants inserted in the 1980s and 1990s sterilized by gamma radiation in air. Implant manufacturers eliminated manufacturing and distributing gamma sterilization in air implants in the late 1990s. This variable therefore cannot account for the early implant failures in the current joint registry reports. We can explain and address the higher early failure rates with unicondylar components inserted after the year 2000 by carefully examining knee registry data. A marked difference is noted in the slope of the curves in the first 4 years, with higher early failures for UKAs (Fig. 1–3). Early failures are commonly related to technical errors in the surgical procedure. The three common modes of early failure are infection, aseptic loosening, and progression of disease. Since we know that infection rates are lower with UKA, then loosening and progression of disease are the likely cause of these early failures. Early failures are most likely technical errors in surgical technique. Industry needs to focus on refined instrumentation and enhancing surgical training to resolve this problem. There is compelling support for unicondylar arthroplasty procedures in 10-year registry data, if the data are analyzed with adjustment for patient variables as well as the surgeon experience variables that are known to impact outcomes. Patient demographics are distinctly different. The most common age group for a UKA in the Swedish register is under the age of 60, with almost half the cases in this age group. The revision rate at 10 years for TKAs done in patients under the age of 60 is 13%.37 UKAs, unlike TKAs, are not performed in patients with an inflammatory disease diagnosis. The Mayo Clinic study reported a higher survivorship in this category and a higher survivorship for female patients following TKA surgery.38 The ratio of females to males undergoing TKA is roughly 2 : 1. In the 2006 Australian registry, 50% of the patients undergoing a UKA were male (ratio 1 : 1) and 40% were males in the 2007 Swedish register. Males and particularly young males have statistically higher revision rates in TKA outcome reports.38
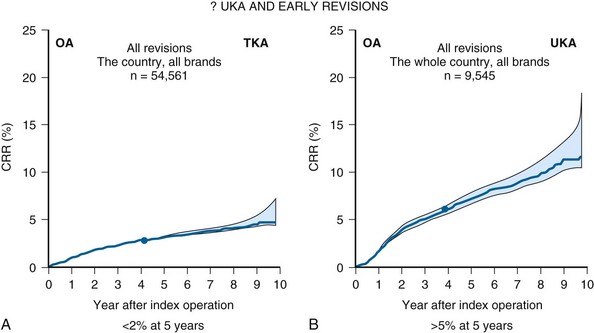
Figure 1–3 Higher failure rates in the first 4 years with unicondylar implants.
(Reprinted with permission from Department of Orthopedics. The Swedish Knee Arthroplasty Registry—Annual Report 2007–Part II. Lund, Sweden: Lund University Hospital, 2007, pp 26, 29.)
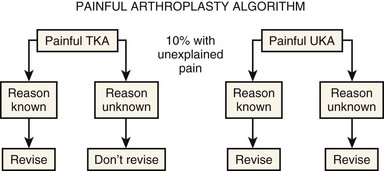
One additional explanation for the continued higher failures with unicondylar surgery is that, in most outcome studies, roughly 10% of patients have fair or poor results following knee arthroplasty, without a known explanation for subjective failure. Surgeons commonly have a different bias for revision of a painful UKA than a TKA (Fig. 1–4). Surgeons are hesitant to revise a painful TKA without a known cause for the pain because the reported success rate with such a procedure is only 25%.39 They are not hesitant, however, to convert a UKA to a TKA.
 The Future for UKA (see Video 1-1)
The Future for UKA (see Video 1-1)
Unicondylar knee arthroplasty did not become an accepted surgical procedure for most of the orthopaedic community until the year 2000. To a certain extent UKA implants, instruments, and surgical experience are in their infancy. The results are spectacular when the procedure is properly performed and equivalent to or better than TKA, as recently reported by Newman et al. in a prospective randomized study with 15-year outcome data.40 The literature supports excellent outcomes with both fixed- and mobile-bearing unicondylar implants inserted with cement fixation. Correct component-to-component alignment is a variable that is not present with a TKA and comes only with surgical experience with today’s traditional instrumentation. Progression of disease in the opposite compartment appears to be a rare occurrence, but overstuffing the replaced compartment to try to restore full correction of mechanical alignment is contraindicated. The status of acceptable changes in the opposite patellofemoral and tibiofemoral compartments for a successful unicompartmental arthroplasty remains controversial and requires critical prospective randomized study data. The greatest challenge, however, appears to be the surgeon variable (Box 1–1).
1 Gunston FH. Polycentric knee arthroplasty. J Bone Joint Surg [Br]. 1971;53:272-277.
2 Lewallen DG, Bryan RS, Peterson LF. Polycentric total knee arthroplasty: a ten year follow-up study. J Bone Joint Surg [Am]. 1984;66:1211-1218.
3 Insall JN, Ranawat CS, Aglietti P, et al. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg [Am]. 1976;58:754-765.
4 Scott RD, Santore RF. Unicondylar unicompartmental replacement for osteoarthritis of the knee. J Bone Joint Surg [Am]. 1981;63:536-544.
5 Insall JN, Walker P. Unicondylar knee replacement. Clin Orthop Relat Res. 1976;120:83-85.
6 Insall JN, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg [Am]. 1980;62:1329-1337.
7 Laskin RS. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg [Am]. 1978;60:182-185.
8 Goodfellow JW, O’Connor J. Clinical results of the Oxford knee: surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res. 1986;205:21-42.
9 Goodfellow JW, O’Connor J. The anterior cruciate ligament in knee arthroplasty: a risk factor with unconstrained meniscal prostheses. Clin Orthop Relat Res. 1992;276:245-252.
10 Murray DW, Goodfellow JW, O’Connor J. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg [Br]. 1998;80:983-989.
11 Knutson K, Lewold S, Robertsson O, et al. The Swedish Knee Arthroplasty Register: a nation-wide study of 30,003 knees 1976–1992. Acta Orthop Scand. 1994;65:375-386.
12 Robertsson O, Dunbar M, Pehrsson T, et al. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262-267.
13 Lewold S, Goodman S, Knutson K, et al. Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis: a Swedish multicenter survival study. J Arthroplasty. 1995;10:722-731.
14 Scott RD, Cobb AG, McQueary FG, et al. Unicompartmental knee arthroplasty: eight- to 12-year follow-up evaluation with survivorship analysis. Clin Orthop Relat Res. 1991;271:96-100.
15 Kozinn SC, Scott RD. Unicondylar knee arthroplasty. J Bone Joint Surg [Am]. 1989;71:145-150.
16 Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg [Am]. 1991;73:186-190.
17 Cobb AG, Kozinn SC, Scott RD. Unicondylar or total knee replacement: the patient’s preference. J Bone Joint Surg [Br]. 1990;70:166.
18 Rougraff BT, Heck DA, Gibson AE. A comparison of tricompartmental and unicompartmental arthroplasty for the treatment of gonarthrosis. Clin Orthop Relat Res. 1991;273:157-164.
19 Laurencin CT, Zelicof SB, Scott RD, et al. Unicompartmental versus total knee arthroplasty in the same patient. Clin Orthop Relat Res. 1991;273:151-156.
20 Knutson K, Lindstrand A, Lidgren L. Survival of knee arthroplasties: a nation-wide multicentre investigation of 8000 cases. J Bone Joint Surg [Br]. 1986;68:795-803.
21 Knutson K, Jonsson G, Langer Anderson J, et al. Deformation and loosening of the tibial component in knee arthroplasty with unicompartmental endoprostheses. Acta Orthop Scand. 1981;52:667-673.
22 Koskinen E, Paavolainen P, Eskelinen A, et al. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop Scand. 2007;78:128-135.
23 Eickmann TH, Collier MB, Sukezaki F, et al. Survival of medial unicondylar arthroplasties placed by one surgeon 1984–1998. Clin Orthop Relat Res. 2006;452:143-149.
24 Blunn GW, Joshi AB, Lilley PA, et al. Polyethylene wear in unicondylar knee prostheses: 106 retrieved Marmor, PCA, and St Georg tibial components compared. Acta Orthop Scand. 1992;63:247-255.
25 Williams IR, Mayor MB, Collier JP. The impact of sterilization method on wear in knee arthroplasty. Clin Orthop Relat Res. 1998;356:170-180.
26 Collier MB, Engh CAJr, Engh GA. Shelf age of the polyethylene tibial component and outcome of unicondylar knee arthroplasty. J Bone Joint Surg [Am]. 2004;86:763-769.
27 McGovern TF, Ammeen DJ, Collier JP, et al. Rapid polyethylene failure of unicondylar tibial components sterilized with gamma irradiation in air and implanted after a long shelf life. J Bone Joint Surg [Am]. 2002;84:901-906.
28 Squire MW, Callaghan JJ, Goetz DD, et al. Unicompartmental knee replacement: a minimum 15 year followup study. Clin Orthop Relat Res. 1999;367:61-72.
29 Berger RA, Nedeff DD, Barden RM, et al. Unicompartmental knee arthroplasty: clinical experience at 6- to 10-year followup. Clin Orthop Relat Res. 1999;367:50-60.
30 Pennington DW, Swienckowski JJ, Lutes WB, et al. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg [Am]. 2003;85:1968-1973.
31 Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty. J Bone Joint Surg [Br]. 1998;80:983-989.
32 Svard UCG, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival study. J Bone Joint Surg [Br]. 2001;83:191-194.
33 Gioe TJ, Killeen KK, Hoeffel DP, et al. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003;416:111-119.
34 Hamilton WG, Collier MB, Tarabee E, et al. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):98-107.
35 Department of Orthopedics. The Swedish Knee Arthroplasty Register—Annual Report 2004, Part I. Lund, Sweden: Lund University Hospital; 2004. p 6
36 Department of Orthopedics. The Swedish Knee Arthroplasty Register—Annual Report 2007, Part II. Lund, Sweden: Lund University Hospital; 2007. pp 26-29
37 Harrysson OLA, Robertsson O, Nayfeh JF. Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res. 2004;421:162-168.
38 Rand JA, Trousdale RT, Ilstrup DM, et al. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg [Am]. 2003;85:259-265.
39 Mont MA, Serna FK, Krackow KA, et al. Exploration of radiographically normal total knee replacements for unexplained pain. Clin Orthop Relat Res. 1996;331:216-220.
40 Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomized controlled trial. J Bone Joint Surg [Br]. 2009;91:52-57.