Umbilical and Other Abdominal Wall Hernias
Umbilical Hernia
Anatomy
After birth, closure of the umbilical ring is the result of complex interactions of lateral body wall folding in a medial direction, fusion of the rectus abdominis muscles into the linea alba, and umbilical orifice contraction which is aided by elastic fibers from the obliterated umbilical arteries. Fibrous proliferation of surrounding lateral connective tissue plates and mechanical stress from rectus muscle tension may also help with natural closure. Failure of these closure processes results in umbilical hernia. The hernia sac is peritoneum, which is usually very adherent to the dermis of the umbilical skin. The actual fascial defect can range from several millimeters to 5 cm or more in diameter. The extent of skin protrusion is not always indicative of the size of the fascia defect. Frequently, small defects can result in alarmingly large proboscis-like protrusions (Fig. 49-1). Thus, it is important to palpate the actual fascia defect by reducing the hernia to assess whether operative or nonoperative treatment is appropriate.
Incidence
The incidence of umbilical hernia in the general population varies with age, race, gestational age, and coexisting disorders. In the USA, the incidence in African-American children from birth to 1-year-old ranges from 25–58%, whereas Caucasian children in the same age group have an incidence of 2–18.5%.1,2 Premature and low birth weight infants have a higher incidence than full-term infants.3 Infants with certain other conditions, such as Beckwith–Wiedemann syndrome, Hurler syndrome, various trisomy conditions (trisomy 13, 18, and 21), and congenital hypothyroidism, also have an increased incidence as do children requiring peritoneal dialysis.4,5
Treatment
For many years, it has been known that umbilical hernias will close spontaneously. It seems very safe to observe the hernia until ages 3 to 4 years to allow closure to occur. Pressure dressings and other devices to keep the hernia reduced do not enhance the closure process and may result in skin irritation and breakdown. Although dated, a number of studies in both Caucasian and African-American populations showed spontaneous resolution rates of 83–95% by 6 years of age. 6–10 Another study found that 50% of hernias still present at age 4 to 5 years will close by age 11 years.9 One study suggests that hernias with fascial defects greater than 1.5 cm are unlikely to close by age 6 years, whereas other series conclude that even large defects will spontaneously resolve without operation.8,11,12 The primary danger associated with observation therapy is the possibility of incarceration or strangulation. Studies have shown these complications to be quite rare, with an incidence of less than 0.2%.8,12,13 Patients with small fascial defects (0.5–1.5 cm in diameter) appear more prone to incarceration.14
The operative closure of an umbilical hernia is generally straightforward, and can usually be completed as an outpatient procedure. Methods used commonly in the adult, such as prosthetic placement, are almost never needed in the child. The most common method of repair is shown in Figs 49-2 and 49-3. A small transverse infraumbilical incision is made, usually placed in the redundant skin, which is inverted at the conclusion of the procedure, thereby hiding the incision. The hernia sac is identified and dissected free from the dermis underlying the umbilical cicatrix. The author’s preference is excision of the sac to the fascial edges, although other surgeons prefer a more limited excision of the sac or inversion of the sac through the fascial opening. Interrupted sutures of nonabsorbable or long-lasting absorbable sutures are placed and tied, closing the fascial defect in a transverse direction. The author leaves the needle attached to the central fascial suture, which is then used to tack the underside of the umbilical skin to the fascia. The skin incision is closed with an absorbable subcuticular suture, and a dressing is applied. Many surgeons use a pressure dressing to help prevent the development of hematoma and keep the umbilical skin inverted, but this type of dressing may not be necessary.15
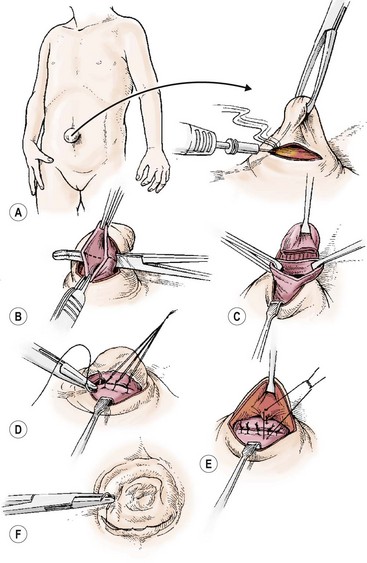
FIGURE 49-2 The technique for operative repair for an umbilical hernia. (A) An infraumbilical skin crease incision is made. (B) The hernia sac is opened, leaving a portion of the sac attached to the umbilical skin for ease of subsequent umbilicoplasty. (C) The umbilical sac has been completely divided and excised to strong fascia. (D) The fascial defect is closed in a transverse fashion with interrupted, simple nonabsorbable sutures. (E) The remaining umbilical sac, which is attached to the umbilical skin, is secured to the fascia with interrupted, absorbable sutures. (F) The skin incision is closed with a subcuticular suture.
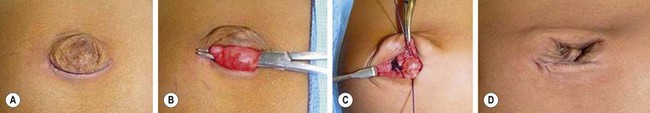
FIGURE 49-3 The steps depicted in the operative diagram in Figure 49-2 are shown. (A) An infraumbilical incision is made. (B) The umbilical hernia sac has been encircled with a hemostat. (C) The umbilical hernia sac is excised, and transverse closure of the fascial defect is accomplished with interrupted long-lasting absorbable sutures. (D) The umbilicus has been tacked to the fascial closure, and the skin is approximated with a subcuticular closure.
Excision of the redundant skin is usually not performed because it tends to return to a normal appearance after the hernia is repaired. This can take up to 12 months to occur, and the family should be reassured appropriately. If the umbilicus fails to return to an acceptable appearance after one to two years, there are a number of techniques described to restore it to a more normal configuration.16–18
There are a few complications of umbilical hernia repair and include seroma or hematoma formation. These are usually self-limited and resolve spontaneously. Wound infections can generally be managed with local care and antibiotics, whereas a recurrent hernia, occurring in less than 1%, requires reoperation.14
Epigastric Hernia
Hernias of the abdominal wall through the midline linea alba, also termed epigastric hernias, are common in the pediatric age group. These hernias present as small masses, usually with incarcerated properitoneal fat, between the umbilicus and xiphoid process (Fig. 49-4). An epigastric hernia should not be confused with diastasis recti, which is generalized weakness in the linea alba from umbilicus to xiphoid, and virtually always resolves by age 10 years. Incarcerated epigastric hernias can be painful. These hernias can also be multiple and associated with an umbilical hernia. Epigastric hernias do not resolve and should be repaired.
Spigelian Hernia
Spigelian hernias are quite rare in children and can be difficult to detect and diagnose. The actual defect occurs at the intersection of the linea semicircularis, linea semilunaris, and the lateral border of the rectus abdominis muscle. It usually involves absence or attenuation of the transversus abdominis and internal oblique muscles. These hernias are more frequently found in girls and more commonly occur on the right side below the umbilicus.19 They are also occasionally associated with skeletal abnormalities.20 Pain in the area with a feeling of fullness or an actual mass are the most common symptoms. Ultrasonography may aid in the diagnosis. In select cases, computed tomography may be needed.
Lumbar Hernia
Lumbar hernias are usually visible shortly after birth as a bulge in the area bordered by the 12th rib, sacrospinalis muscle, and internal oblique muscle. Occasionally, they extend inferiorly to the iliac crest. These hernias tend to develop at the site of penetration of the intercostal nerves and vessels, or of the ilioinguinal, iliohypogastric, and lumbar nerves. The bulge is usually properitoneal fat. Therefore, the physical findings include a soft mass that is easily reducible. Although frequently asymptomatic, repair is advisable because the defect never resolves spontaneously and incarceration is possible.
References
1. Crump, EP. Umbilical hernia: Occurrence of the infantile type in Negro infants and children. J Pediatr. 1952; 40:214–233.
2. Evans, AG. The comparative incidence of umbilical hernia in colored and white infants. J Natl Med Assoc. 1940; 33:158–160.
3. Vohr, BR, Rosenfield, AG, Oh, W. Umbilical hernia in the low-birth weight infant (less than 1500 gm). J Pediatr. 1977; 90:807–808.
4. Jones, KL. Abdominal wall. In: Jones KL, ed. Smith’s Recognizable Patterns of Human Malformation. 4th ed. Philadelphia: WB Saunders; 1988:P753–P754.
5. Tank, EW, Hatch, DA. Hernias complicating chronic ambulatory peritoneal dialysis in children. J Pediatr Surg. 1986; 21:41–42.
6. Woods, GE. Some observations on umbilical hernias in infants. Arch Dis Child. 1953; 28:450–462.
7. Heifitz, CJ, Bilsel, ZE, Gans, WW. Observations on the disappearance of umbilical hernias of infancy and childhood. Surg Gynecol Obstet. 1963; 116:467–473.
8. Walker, SH. The natural history of umbilical hernia. Clin Pediatr. 1967; 6:29–32.
9. Hall, DE, Roberts, KB, Charney, E. Umbilical hernia: What happens after age 5 years? J Pediatr. 1981; 98:415–417.
10. Sibley, WL, Lynn, HE, Harris, LE. A twenty-five year study of infantile umbilical hernia. Surgery. 1964; 55:462–468.
11. Blumberg, NA. Infantile umbilical hernia. Surg Gynecol Obstet. 1980; 150:187–192.
12. Halpern, LJ. Spontaneous healing of umbilical hernias. JAMA. 1962; 182:851–852.
13. Mestal, AL, Burns, H. Incarcerated and strangulated umbilical hernias in infants and children. Clin Pediatr. 1963; 2:368–370.
14. Lassaletta, L, Fonkalsrud, EW, Tovar, JA, et al. The management of umbilical hernia in infancy and childhood. J Pediatr Surg. 1975; 10:405–409.
15. Merci, J. Umbilical hernia repair in children: Is pressure dressing necessary? Pediatr Surg Int. 2006; 22:446–448.
16. Jamra, F. Reconstruction of umbilicus by a double V-Y procedure. Plast Reconstr Surg. 1979; 64:106–110.
17. Reyna, T, Hllis, H, Smith, S. Surgical management of proboscoid hernia. J Pediatr Surg. 1978; 22:911–912.
18. Koshy, C, Taams, K. Umbilicoplasty. Plast Reconstr Surg. 1999; 104:1203–1204.
19. Spangen, L. Spigelian hernia. Surg Clin North Am. 1984; 64:351–366.
20. Asku, B, Temizoz, O, Inan, M, et al. Bilateral Spigelian concomitant with multiple skeletal anomalies and fibular aplasia in a child. Eur J Pediatr Surg. 2008; 18:205–208.







