14 Ultrasound-Guided Catheter Placement for Peripheral Nerve Blocks
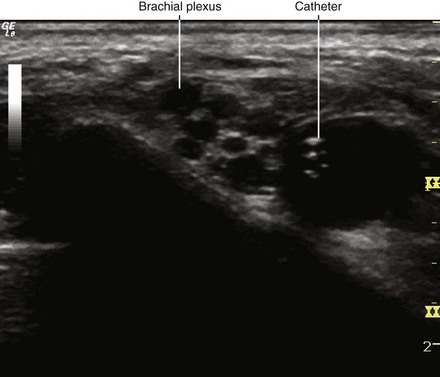
Ultrasound-guided catheter placement is a complex procedure involving advanced manipulative skills of the operator.1 Common procedures are ultrasound-guided interscalene, femoral, and popliteal catheters.2 Both in-plane and out-of-plane approaches are popular for peripheral nerve catheter insertion.3
With in-plane technique the needle bevel can be turned so that the catheter slides along the nerve rather than around the nerve.4 A helically wound, metal-reinforced catheter can act as a spatially modulated wire.5 Therefore, the ultrasound beam will be reflected back to the transducer regardless of the catheter orientation to improve visibility.
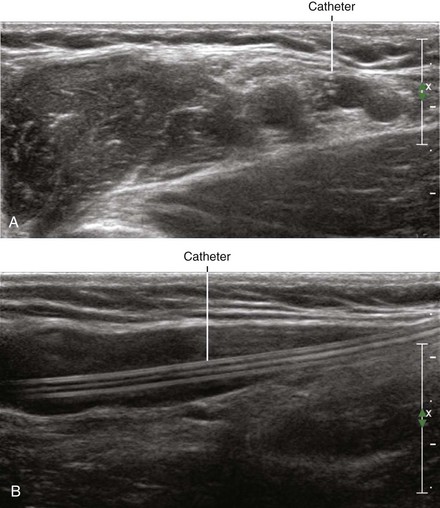
Long-axis in-plane approaches to peripheral nerve catheter placement have been reported.6 The advantage is that the peripheral nerve, block needle, and catheter can all be viewed at the same time. However, it can be difficult to manipulate the transducer to maintain all three within the plane of imaging. Furthermore, because all three are constrained to lie in the same plane, care must be taken not to advance the needle and catheter into the nerve. Sciatic nerve catheters are particularly amenable to the long-axis in-plane approach if the patient can be placed in a prone position. With this long-axis approach, the operator views directly across the patient for anatomic orientation of the ultrasound monitor.
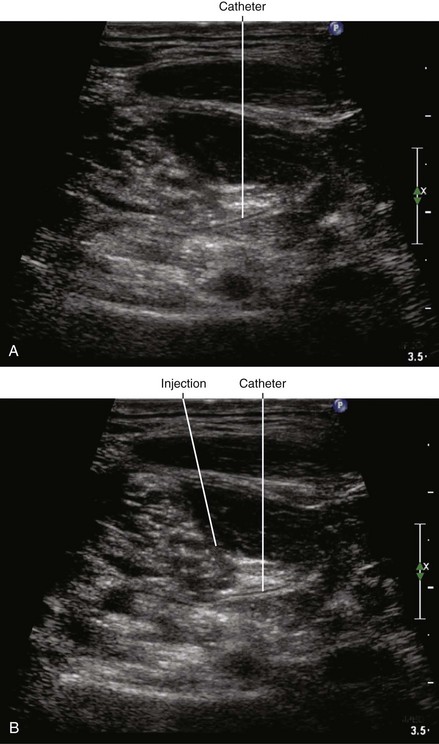
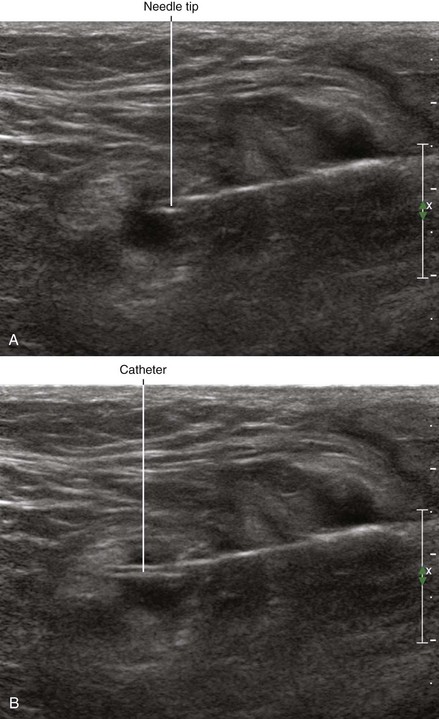
Ultrasound guidance appears to have advantages over nerve stimulation for peripheral nerve catheter placement because the performance times are more consistent.7 Many practitioners use the same in-plane approach to catheter placement that would be used for single-shot blocks. Although treading distances beyond the needle tip are typically short, the in-plane approach to catheter placement is similar to tunneling because of the long path through tissue to reach the target. One study found no difference between 1 cm and 5 cm threading distances with in-plane approach in terms of catheter function and rate of dislodgement.8 If deemed necessary, some practitioners inject local anesthetic or saline and pull the needle back slightly before threading the catheter to create more space for short axis in-plane approach.
1 Fredrickson MJ. Ultrasound assisted perineural catheter placement facilitated by a catheter introduction syringe. Reg Anesth Pain Med. 2007;32:370–371.
2 Swenson JD, Bay N, Loose E, et al. Outpatient management of continuous peripheral nerve catheters placed using ultrasound guidance: an experience in 620 patients. Anesth Analg. 2006;103:1436–1443.
3 Fredrickson MJ, Ball CM, Dalgleish AJ. Successful continuous interscalene analgesia for ambulatory shoulder surgery in a private practice setting. Reg Anesth Pain Med. 2008;33:122–128.
4 Borgeat A, Blumenthal S, Lambert M, et al. The feasibility and complications of the continuous popliteal nerve block: a 1001-case survey. Anesth Analg. 2006;103:229–233.
5 Trimmer WS, Vilkomerson D. A new wire phantom for accurate measurement of acoustical resolution. Ultrason Imaging. 1983;5:87–93.
6 Koscielniak-Nielsen ZJ, Rasmussen H, Hesselbjerg L. Long-axis ultrasound imaging of the nerves and advancement of perineural catheters under direct vision: a preliminary report of four cases. Reg Anesth Pain Med. 2008;33:477–482.
7 Mariano ER, Loland VJ, Sandhu NS, et al. A trainee-based randomized comparison of stimulating interscalene perineural catheters with a new technique using ultrasound guidance alone. J Ultrasound Med. 2010;29:329–336.
8 Ilfeld BM, Sandhu NS, Loland VJ, et al. Ultrasound-guided (needle-in-plane) perineural catheter insertion: the effect of catheter-insertion distance on postoperative analgesia. Reg Anesth Pain Med. 2011;36:261–265.