Sagittal section of a fetus showing measurement of crown–rump length.
Algorithm for a structural survey in early pregnancy
Brain
Cranial bone ossification and the integrity of the skull should be noted to exclude severe anomalies like acrania. The hemispheres should appear symmetrical and separated by a clear midline falx cerebri and interhemispheric fissure. By 7 weeks, a sonolucent area can be seen in the cephalic pole. By 9 weeks, a convoluted pattern of three primary cerebral vesicles is noted, followed by the appearance of brightly echogenic choroid plexus filling the lateral ventricles by 11 weeks. It is difficult to assess the integrity of the cerebellum, cavum septum pellucidum and corpus callosum at this gestation (Figures 5.2 and 5.3).
A BPD measurement less than the 10th centile may be a subtle sign of open spina bifida[7].
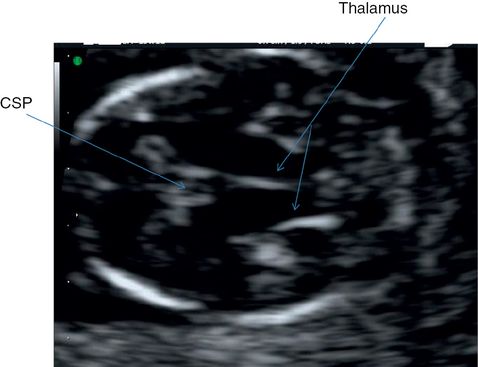
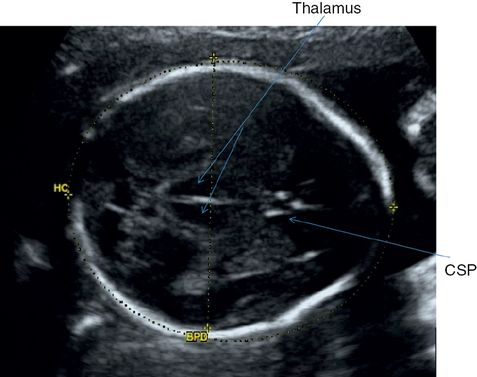
Transverse section through fetal head showing midline echo, thalamus and cavum septum pellucidi (CSP).
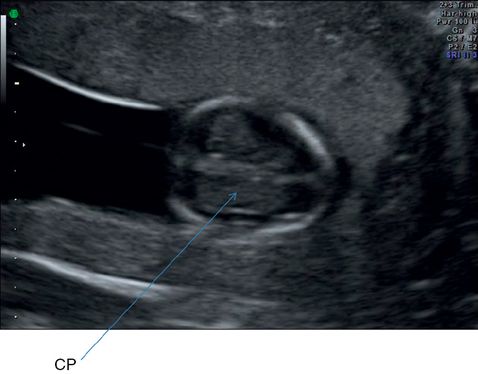
Transverse section through brain ventricles demonstrating relatively prominent-appearing choroid plexus (CP).
Neck
One of the biggest advances in prenatal diagnosis is the measurement of nuchal translucency (NT). The correct NT should be obtained by adopting and ensuring the following criteria are met.
-
Obtain a sagittal section of the fetus and magnify the image in order to include only the fetal head and upper thorax. The true sagittal section will demonstrate an echo from the tip of the nose, a second echo from the nasal bone and a square and well-defined echo from the maxilla.
-
Fetal spine and neck should be in a neutral position with a pool of amniotic fluid between the chin and the upper chest. Hyperflexion or hyperextension will lead to erroneous measurement.
-
Calipers should be placed correctly, with the horizontal portion of the + marker exactly on the inner borders of the lines demarcating the nuchal space or NT. It should be placed perpendicular to the long axis of the fetus at the widest portion of the NT space. The amnion should be seperately identified to avoid mistaking it for the fetal skin (Figure 5.4).
-
If more than one measurement meeting all the criteria is obtained, the maximum one should be recorded and used for aneuploidy risk assessment.

A midline sagittal section showing measurement of nuchal translucency.
Face
An attempt should be made to look at the face in coronal plane. If clear views are not obtained, it should be re-assessed at the second-trimester scan[1].
Heart
A four-chamber view of the heart can be obtained starting from 10 to 13 weeks[8]. Complete examination of the fetal heart in the first trimester can be challenging due to the smaller size. As a minimum, the position of the heart and the four-chamber view should be noted. In case of any suspected abnormality, a detailed scan is warranted in the second trimester for further evaluation.
Abdomen
The physiologic umbilical hernia is present up to 11 weeks, and should be differentiated from gastroschisis and omphalocoele. Kidneys and bladder should be noted. Kidneys appear in the paraspinal region as bean-shaped structures. The bladder can be visualized in the normal site as a hypoechoic area (Figures 5.5–5.8).

Transverse section through fetal abdomen shows the stomach and an oblique section of the umbilical vein. Longitudinal section of a single rib on either side and a cross-section of the spine is also visible.

Coronal section through fetal trunk showing a section of the spine and longitudinal section of the fetal kidneys.
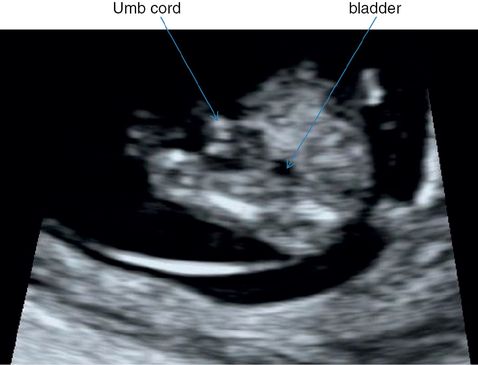
Transverse section through fetal lower abdomen showing umbilical cord insertion and the bladder.

Longitudinal section of fetal trunk showing umbilical cord insertion and the anterior abdominal wall.
Spine
The role of the first-trimester scan in detecting small defects of the spine is limited; however, severe cases of spinal abnormalities may be detected by a systematic examination[9]. Careful observation should be undertaken to visualize an intact skin covering over the spine (Figure 5.9).
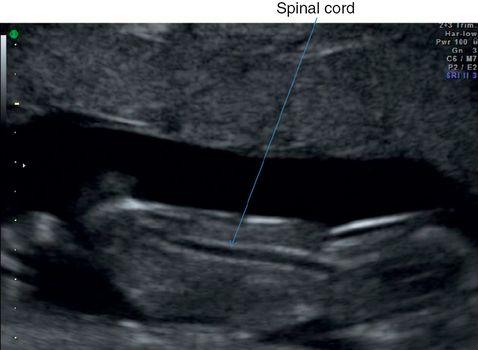
Longitudinal section through fetal spine to show skin covering. The spinal cord is visible as a tubular sonolucent structure. Faint echogenic vertebrae are also visible.
Limbs
Note the presence of four limbs with three bony segments in each of the upper and lower limbs with normal orientation of the two hands and feet (Figure 5.10).

Longitudinal section through fetal forearm and hand showing both long bones and five digits.
Checklist for examination of fetal anatomy in the first trimester[1]
| Brain | Integrity of skull Midline falx Choroid plexus – filled Ventricles |
| Face | Eyes with lens Nasal bone Normal profile/mandible Intact lips |
| Neck | Nuchal translucency thickness Any fluid-filled collections |
| Spine | Longitudinal and axial view of vertebrae Skin integrity |
| Chest | Symmetrical lung fields No effusions or masses Regular cardiac activity Four-chamber view Check situs visceralis with stomach and heart on the left side of the abdomen Diaphragm |
| Abdomen | Stomach in left upper quadrant Intact abdominal wall Normal cord insertion after 12 weeks Kidney and bladder |
| Extremities | Four limbs each with three segments Hands and feet with normal orientation Femoral length |
| Placenta and amniotic fluid volume |
Limitations
One of the limitations of the first-trimester anomaly scan as a routine screening method in a low-risk population is the poor sensitivity for certain anomalies like those of the heart, spine and brain due to the stages of embryologic development. Therefore, even if an early fetal anomaly scan were offered, the second-trimester scan should not be abandoned. Secondly, in women with raised body mass index, the image quality in the transabdominal scan may be compromised. A transvaginal approach will improve the sensitivity, but the patient’s acceptance may be a limiting factor.
The routine second-trimester scan
The second-trimester anomaly scan is offered between 18+0 weeks to 20 weeks and 6 days of gestation in most countries. The timing is appropriate for detailed evaluation of most of the anatomical structures. Although not the ideal gestation for dating the pregnancy, it can be useful in dating in the case of a missed opportunity for a first-trimester scan.
Diagnostic value of routine ultrasound scan in the second trimester
(a) Lethal anomalies[10]
| Anencephaly | 97.6% |
| Trisomy 18 | 68.4% |
| Trisomy 13 | 50.0% |
| Hypoplastic left heart | 54.5% |
| Bilateral renal agenesis | 90.0% |
| Lethal musculoskeletal disorders | 33.3% |
(b) Possible survival and long-term morbidity[10]
| Spina bifida | 66.3% |
| Hydrocephalus | 68.9% |
| Encephalocele | 90.9% |
| Holoprosencephaly | 72.7% |
| Down’s syndrome | 14.6% |
| Complex cardiac malformations | 21.3% |
| Atrioventricular septal defect | 12.9% |
| Nonlethal dwarfism | 100% |
| Anterior abdominal wall defect | 89.5% |
| Gastroschisis | 94.1% |
| Exomphalos | 84.6% |
| Congenital diaphragmatic hernia | 47.9% |
| Tracheoesophageal atresia | 7.4% |
| Small bowel obstruction/atresia | 40.6% |
| Congenital cystic adenomatoid malformation | 100% |
| Renal dysplasia (bilateral) | 84.2% |
| Multiple abnormality/syndrome | 77.8% |
| Obstructive uropathy | 100% |
| Pleural effusion or hydrothorax | 100% |
(d) Anomalies associated with possible short term/immediate morbidity[10]
| Facial clefts | 13.8% |
| Talipes | 20.1% |
| Atrial/ventricular septal defect | 6.3% |
| Isolated valve anomalies | 22.7% |
| Renal dysplasia (unilateral) | 86.7% |
A stepwise approach for a routine second-trimester anomaly scan is listed below.
(1) Confirm viability.
(2) Order of pregnancy.
(3) Placentation.
(4) Fetal biometry.
(5) Systematic structural survey.
(6) Amniotic fluid assessment.
Fetal biometry
For assessment of the fetal size and growth, the standard measurements used are the HC, BPD, abdominal circumference and femoral length.
Head circumference and biparietal diameter
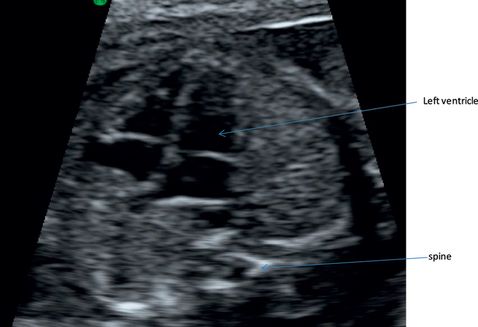
Both the HC and BPD measurements can be obtained from the same plane; the transventricular plane or the transthalamic plane can be used for obtaining these measurements. The HC can be measured by using the ellipse method by placing the ellipse around the outside of the skull bone echoes. HC measurement is more reliable than the BPD in cases of abnormal shape of the head.
The BPD can be measured by two techniques – the outer-edge to inner-edge technique or the outer-edge to outer-edge by placing the calipers at the widest part of the skull. It is important to ensure that the placement of the calipers corresponds to the technique described on the reference chart, especially for the BPD (outer-to-outer or outer-to-inner) (Figures 5.11 and 5.12).
Transthalamic section of fetal head showing measurement of head circumference (HC) and biparietal diameter (BPD).
A cross-sectional view of the head is obtained at the level of thalami with a short midline echo equidistant from the proximal and distal skull echoes. The structures that should be identified in the midline anteriorly to posteriorly are the cavum septum pellucidum (CSP), the thalami and basal cisterns[12].

A cross-sectional view of the head is obtained at the level of lateral ventricles with a long midline echo equidistant from the proximal and distal skull echoes. The structures that should be identified in the midline anteriorly to posteriorly are the anterior horn of the lateral ventricles, cavum septum pellucidum and posterior horns of the lateral ventricles.

Transverse section through fetal upper abdomen demonstrating the cross-section of a vertebrae, an unbroken rib, stomach, cross-section of the umbilical vein, which should be one-third of the distance between the anterior abdominal wall and fetal spine and midway between the lateral abdominal walls[12]. AC, abdominal circumference.

Longitudinal section through fetal thigh showing measurement of femur length (FL). The longest axis of the ossified diaphysis of the upper femur is measured. Each caliper is placed at the ends of the ossified diaphysis without including the distal femoral epiphysis. It is important to exclude artifacts at the end as this might give falsely raised values.

Transverse section through fetal brain showing measurement of the lateral ventricle width distal to the ultrasound probe. Once the transventricular plane is obtained, the calipers are placed at the level of the glomus of the choroid plexus along the inner edges of the ventricular walls at the widest part of the atrium. Values of more than 10 mm are considered abnormal. Due to the physical properties of ultrasound, the proximal ventricle is always more difficult to delineate when scanning from the lateral aspect. Readjusting the ultrasound machine controls and angulating the probe may provide a better view.

Measurement of the proximal cerebral ventricular width.

Transcerebellar section showing measurement of cisterna magna width, which is the horizontal distance between the outer border of the vermis of cerebellum to the inner border of the skull. It should normally measure ≤10 mm.

Transverse section through the posterior aspect of fetal skull showing measurement of nuchal fold thickness. The antero-posterior width is measured from the outer border of the skull to the outer border of the skin and normally should not be more than 6 mm. Part of the cerebellum and cisterna magna is also visible.
(e) Checklist for a midtrimester scan[13]
| Structure | Routine screening |
|---|---|
| Skull | Integrity, shape Measurement of biparietal diameter, head circumference |
| Brain | Cavum septi pellucidi Midline falx Thalami Cerebral ventricles (atrial width measurement of lateral ventricles) Cerebellum (measurement of transcerebellar diameter) Cisterna magna |
| Face | Both orbits, lips, mouth Median facial profile Coronal view of nostrils and both lips |
| Neck | Absence of masses Nuchal fold thickness |
| Spine | Transverse, coronal, sagittal views Check integrity, overlying skin |
| Heart | Normal situs, rate, rhythm Four-chamber view Aortic and pulmonary outflow tracts Three-vessel view |
| Thorax | Regular shape of thorax and ribs Exclude any increased echogenicity in the lungs and mediastinal shift Diaphragm |
| Abdomen | Abdominal wall, stomach, any bowel dilatation, umbilical cord insertion |
| Genitourinary tract | Kidneys, renal pelvis, bladder Assessment of the external genitalia is optional, dependent on parental consent and local policy |
| Limbs | Arms with radius, ulna, humerus, both hands with normal relationship Legs with femur, tibia and fibula, both feet with normal relationship |
| Placenta | Placental position and amniotic fluid volume assessment |
Algorithm for structural survey in the second trimester
Brain
Examine the brain in the three planes as described in Figures 5.11, 5.12 and 5.15–5.18. Assess the integrity of the skull, midline structures, lateral ventricles, cavum septum pellucidum, cerebellum and cisterna magna.
Face
Two-dimensional ultrasound screening for cleft lip and palate in a low-risk population has a relatively low detection rate (DR)[14]. The generally reported rates of prenatal recognition of cleft lip range between 21% and 30%. However, this can be increased when the face is examined in three planes, i.e., sagittal, coronal and axial, and by using three-dimensional ultrasound[15].

Coronal section through the lower face showing the chin, opening of mouth, faint view of upper jaw, nasal bone and the lower margin of orbits.

Coronal section through fetal lips and nostrils.

Coronal section through upper face showing orbits.
Thorax
Assessment of the thorax is important to exclude any abnormalities in the heart, lungs, diaphragmatic hernia, hydrops and lethal skeletal dysplasias.
Checklist for assessment of the thorax
-
Shape of the chest. Normal shape is circular to an ellipse in the axial section.
-
Lungs appear as low level homogeneous echoes.
-
The diaphragm appears as a thin echo, poor concave line separating the thorax and abdomen.
-
Exclude any chest wall edema.
-
Assess the shape of the ribs and integrity of the thoracic spine.
-
Measurement of the thoracic circumference at the level of the four-chamber view of the heart in cases of suspected skeletal dysplasia.
-
Position of the heart. The heart occupies one-third of the thoracic area with the cardiac axis pointed to left by 45° ± 20°.

Midline sagittal section through fetal trunk showing the dome of diaphragm. Faint echo of umbilical cord insertion is also visible.
HeartChecklist for assessment of the fetal heart[8,16]
-
Position of the heart. The apex of the heart and stomach should be on the left side of the fetus and the liver on the right side. The laterality should be decided by assessing orientation of the fetal lie and position, and not on the basis of the position of the stomach or the heart.
-
Four-chamber view of the heart. The two atria and the two ventricles, with the foramen ovale in the interatrial septum and the intact interventricular septum, should be visualized. Both the atria and the ventricles should be of the same size. The tricuspid and mitral valves form an offset cross at the atrioventricular (AV) junction as the septal leaflet of the tricuspid valve inserts slightly lower than the mitral valve. Observe the contractility of the atria and the ventricles. An isolated finding of a small echogenic rim around the heart usually represents a normal variation and should not be mistaken for a pericardial effusion.
-
The AV valves and the flap valve of the foramen ovale should be freely opening and closing.
-
Venous drainage. The pulmonary venous connection can be seen on the back of the left atrium by scanning up and down horizontally at the back of left atrium.
-
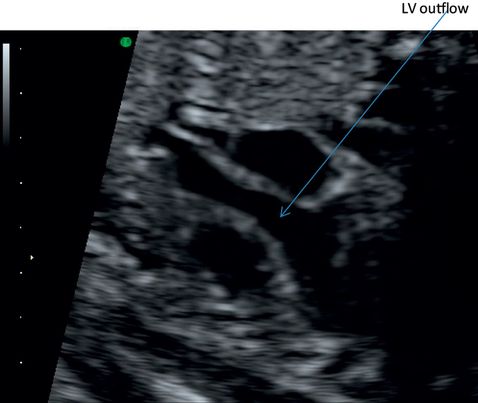
Origin of the great vessels. This is best done by moving the probe cranially from the four-chamber view. On angling towards the right shoulder, the left ventricular outflow tract can be demonstrated. The transverse section cranial to this will demonstrate the origin of the pulmonary artery from the right ventricle.
-
Crossover of the great vessel at right angles to each other at their respective origins.
-
Three-vessel views demonstrate from left to right, and anterior to posterior, the pulmonary artery, the aorta and the superior vena cava (SVC). The pulmonary artery is the largest in diameter, followed by the aorta and the SVC.
-
In the three-vessels and tracheal view, which is more cephalad from the three-vessel view, the aortic arch, the ductal arch and the trachea can be visualized. For the right ventricular connections, obtain a longitudinal view of the left ventricle and angulate the transducer slightly in the opposite direction. This will demonstrate the inferior vena cava entering the right atrium, the origin of pulmonary artery from the right ventricle and its connection to the ductus arteriosus.
-
The aortic arch can be examined in the longitudinal axis view.
-
Observe the cardiac rhythm and exclude pericardial effusion.
Transthoracic close-up view showing four-chamber view of the heart and foramen ovale. Note the offset valve leaflets. Ultrasound fall-off at the interventricular septum near the crux of the heart gives a false impression of a ventricular septal defect.
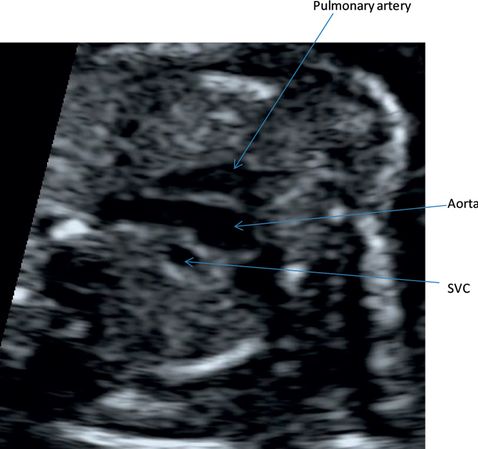
Oblique view through the heart demonstrating the three-vessel view, pulmonary artery, aorta and the superior vena cava (SVC) from above below.
Abdomen
Systematic examination of the abdomen is important to exclude anterior abdominal wall defects (gastroschisis and exomphalos), bowel atresia or obstruction, diaphragmatic hernia, tracheoesophageal fistula. It is also an important landmark for fetal biometry.
The following are the structures that need to be routinely identified.
-
The normal insertion of the umbilical cord should be documented after 12 weeks. The physiologic umbilical hernia is present up to 11 weeks and should be differentiated from gastroschisis and omphalocoele.
-
Presence of the stomach. Absence of the stomach could be due to anhydramnios or a tracheoesophageal fistula.
-
The position of the stomach on the left side of the abdomen together with levocardia helps to confirm normal situs visceralis.
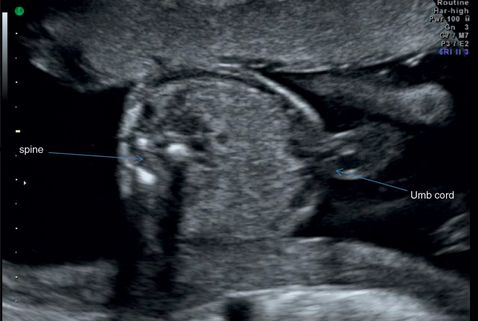
Transverse section through fetal abdomen showing cross-section of the spine and umbilical cord insertion.
Spine
To improve the detection rate of spinal abnormalities, the spine should be viewed in three planes – sagittal, coronal and transverse.
-
In the sagittal plane, the spine has a double railway appearance and it should enable one to appreciate the soft tissue over it.
-
In the coronal plane, the three ossification centers of the vertebrae should be seen. The neural arch should be examined from the cervical segment to the sacrum in all three planes.
-
In the transverse/axial plane, the vertebrae have different shapes at different levels. The cervical vertebrae are quadrangular in shape, the thoracic and lumbar vertebrae have a triangular shape with the ossification centers surrounding the neural canal, and the sacral vertebrae appear flat.

Midline sagittal section through fetal spine showing normal curvature and continuous skin covering.
Extremities/appendicular skeleton
In a routine midtrimester scan, examine the presence of the upper limbs with the humerus, radia, ulna and hands, and the lower limbs with femur, tibia and fibula. The fingers and toes need not be counted. The only bone that needs to be measured in a routine scan is the femur.

Transverse section through fetal feet showing normal orientation of feet.

Coronal section through four fingers. The thumb usually lies in a slightly different plane in the resting position.

Longitudinal section through lower limbs showing normal relation of feet to lower legs. The three long bones of each leg are visible.

Forearm showing both long bones with fingers.
Renal system
The following points are useful in assessing the fetal renal system.
-
The fetal kidneys should be noted in their expected paraspinal location by 12 weeks of gestation.
-
Assessment of renal pelvis. The renal pelvis appears as a hypoechoic area in the kidney. It is measured in the transverse section of the kidneys with the calipers placed on the inner-to-inner side of the renal pelvis. There is wide variation in the literature regarding the maximum cut-off for the renal pelvic diameter at each gestation. A value of 5 mm in the second trimester and 7–10 mm in the third trimester can be used as a cut-off to increase the sensitivity of detection for significant postnatal renal pathology[8].
-
Echogenicity of the kidneys.
-
Assess for any parenchymal abnormality (e.g., renal cortical thinning, lack of corticomedullary differentiation).
-
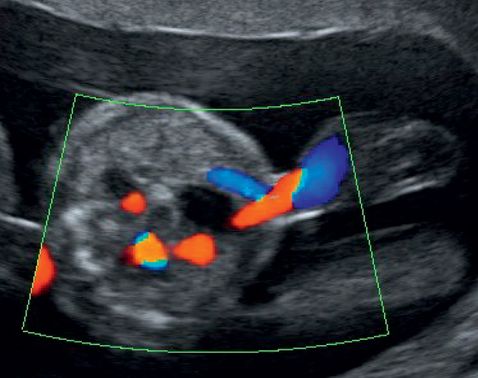
Imaging of fetal bladder. By 12–13 weeks of gestation, the fetal bladder should be visible as a median hypoechoic round structure in the lower abdomen. In case of difficulty in visualizing the bladder, color Doppler can be used to demonstrate the two umbilical arteries encircling the bladder. Changes in the size of the bladder can be observed during the course of the examination because the fetus empties its bladder every 30 to 45 min.
-
Assessment of the adrenal gland. The normal adrenal glands can be imaged with ultrasound as early as 9½ weeks of gestation. They appear as bilateral midecho structures located immediately above the fetal kidneys.
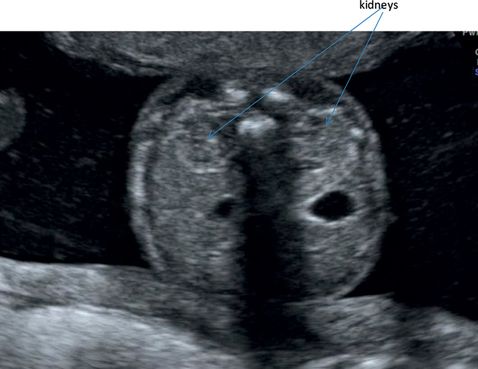
Transverse section through fetal abdomen showing hypoechoeic kidneys situated on either side of the spine.
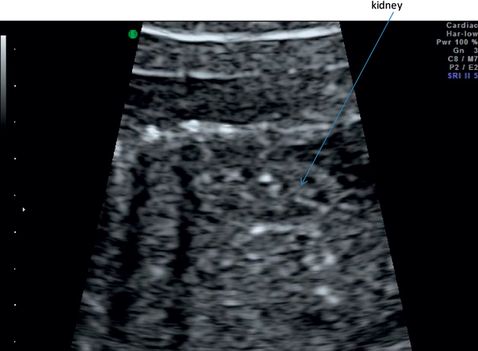
Section through long axis of the spine. The renal length should be measured in this plane.
Transverse section through fetal lower abdomen demonstrating the two umbilical arteries around the bladder.
External genitalia
Reporting of gender is not a part of the routine midtrimester scan. It should be considered only with parental consent and in the context of local practice and clinical need, for example, to assist in managing an X-linked disorder.
Extended examination
An extended examination may be required for further evaluation in case of suspected anomalies. Some of the additional measurements are briefly outlined below and will be covered in detail in the relevant chapters.
Brain
Examination of the corpus callosum is useful in certain conditions, such as ventriculomegaly. It can be imaged in the coronal and sagittal planes. Applying color Doppler to identify the pericallosal artery is useful in the imaging of the corpus callosum. The artery can be demonstrated in the mid-sagittal plane and forms a semicircular course over the superior surface of the corpus callosum[17].
Face
The interorbital distance is useful to rule out hyper- or hypotelorism. It is the distance between the medial borders of the two orbits.
Thorax
Normograms are available for thoracic circumference[15]. Values less than 5th centile and a thoracic and abdominal circumference ratio less than 0.79 are associated with lethal skeletal dysplasia and pulmonary hypoplasia[18].
Kidneys
Measurement of renal size in anteroposterior (AP), transverse and longitudinal diameter in cases of suspected renal anomaly. Longitudinal diameter is measured in the sagittal image, the AP and transverse diameters are measured in the transverse section image. All these measurements are obtained by using the outer-to-outer placement of the calipers along the renal outline. Normograms are available for renal size[19].
Abdomen
Measurement of the bowel diameter is useful in suspected bowel obstruction. Multiple fluid-filled areas in the abdomen can indicate bowel obstruction. In this case, measure the diameter, assess the peristalsis and echogenicity. The diameter is measured from the inner wall to inner wall at the point of maximum dilatation in a cross-section of the fetal abdomen. A clue to differentiate the large bowel from the small bowel is the peripheral location and presence of haustrae. There are no standardized normograms for bowel diameters. A prospective study by Lap et al. has produced a reference chart for small and large bowel diameters in normal fetuses at varying periods of gestation.
Extremities
A femoral length less than 5th centile for the gestation or less than three standard deviations is a strong predictor of skeletal dysplasia. In this case, it is useful to measure all the other long bones and feet, assess the contour of the bones and the mobility of the joints. The views of the tibia and fibula are obtained by rotating the probe from the lower end of the femur. In this view, only the cross-section of the talus of the foot should be seen. Normally, only one bone can be measured at a time. A sagittal view of the foot can be obtained in the lateral view image of the lower limb. By rotating the probe 90° from the lateral view, the plantar view of the foot can be obtained[12]. Three features should be noted in the foot – the carrying angle, shape of the heel and the sole of the foot. The normal femur/foot ratio should be 1, irrespective of the gestational age.