Chapter 12 Ulnar Nerve
Anatomy
Ulnar Nerve Origin
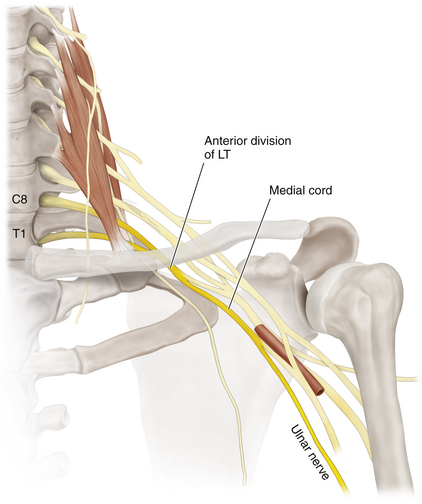
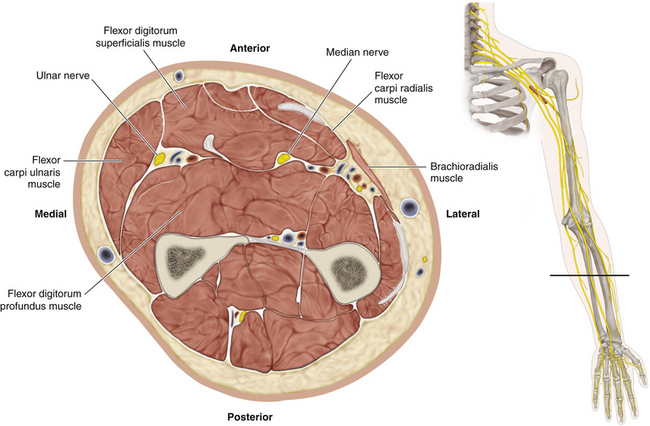
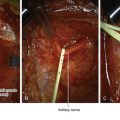
• The medial cord of the brachial plexus continues as the ulnar nerve (Figure 12-1) below the origins of the medial cutaneous nerves of the arm and forearm and the medial head of the median nerve. At its origin, the ulnar nerve lies between the axillary artery and axillary vein, with the medial antebrachial cutaneous nerve in front of it.
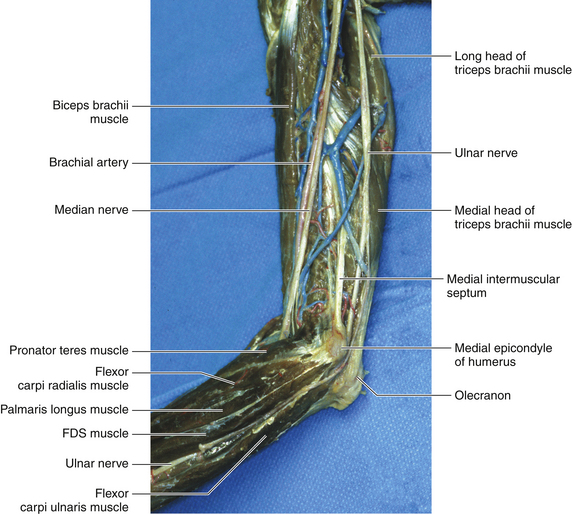
• The ulnar nerve runs straight down from the medial cord complex to the medial epicondyle at the elbow joint (Figure 12-2).
Ulnar Nerve at the Proximal Arm
• The nerve lies deep and medial to the axillary-to-brachial artery segment. The ulnar nerve then descends the proximal arm anterior to the triceps and close to the median nerve.
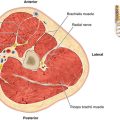
• At the level of insertion of the deltoid, the ulnar nerve leaves the flexor compartment of the arm by running posterior to the medial intermuscular septum. The ulnar nerve is accompanied by the superior ulnar collateral artery and a motor branch to the triceps (radial).
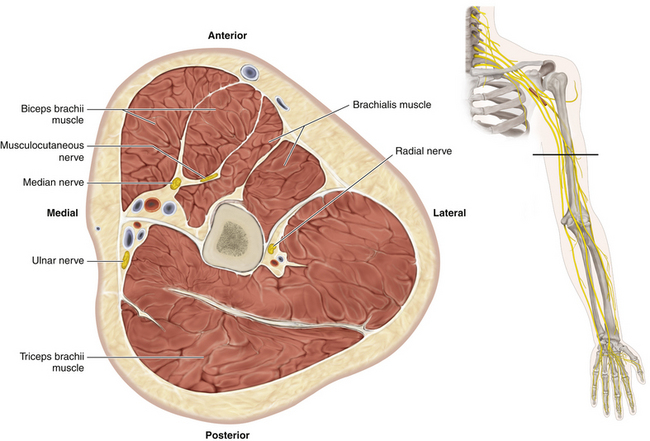
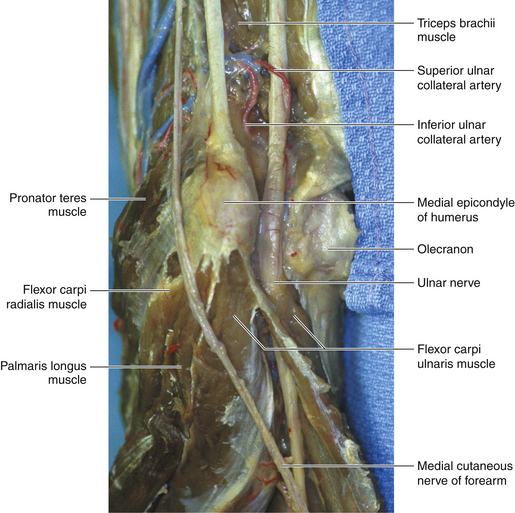
• The nerve runs on the triceps, immediately deep to the investing fascia and just behind the medial intermuscular septum (Figure 12-3).
• In the upper arm, the ulnar nerve is found with reference to the brachial artery. The surgeon must distinguish the ulnar nerve from the median nerve (by relationship to the artery, by stimulation, and, with experience, by appearance).
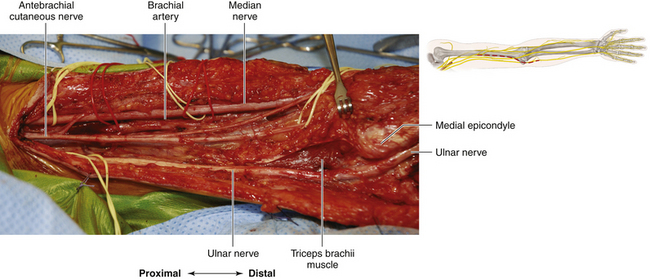
• In the lower arm, there is a constant relationship of ulnar nerve to the olecranon notch. If it is difficult to find the nerve in the lower arm, it can always be found at the elbow and traced proximally (Figure 12-4).
Ulnar Nerve at the Elbow
• The ulnar nerve lies in the groove between the medial epicondyle of the humerus and the olecranon process of the ulna (Figure 12-5). Articular branches are given off to the elbow joint proximal to that structure; they are also given off while the nerve is between the olecranon and medial epicondyle and again while the nerve is below the ulnar collateral ligament.
• The nerve lies in close contact with the periosteum under the deep fascia of the arm and under an expansion of the triceps tendon that fuses medially with the deep fascia of the forearm.
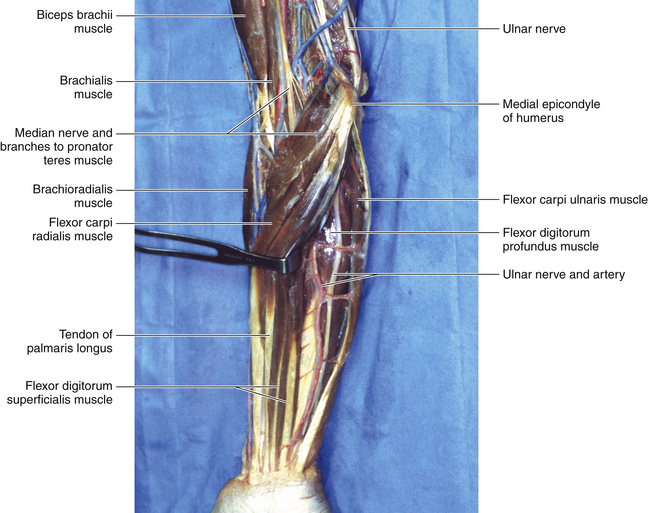
• The ulnar nerve enters the forearm by passing between the two heads (humeral and ulnar) of the flexor carpi ulnaris (FCU). The nerve lies on the surface of the flexor digitorum profundus (FDP) and descends in a straight line to supply the ulnar part of the FDP that sends tendons to digits 4 and 5 (Figure 12-6).
Ulnar Nerve at Forearm Level
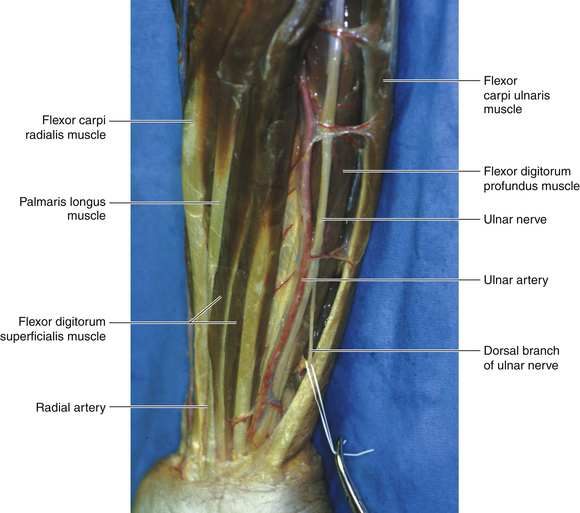
• As the ulnar artery passes distally, it runs medially and obliquely to reach the ulnar nerve at the middle of the forearm (Figures 12-7 and 12-8). The ulnar nerve emerges superficially from under cover of the flexor carpi ulnaris just above the wrist, lying medial to the artery and lateral to the tendon.
• Just as the key to finding the ulnar nerve in the distal arm is the olecranon notch, so the FCU tendon is the key to finding the nerve in the distal forearm (see Figure 12-7).
• The first muscular branch of the ulnar nerve is given off as the nerve passes between the two heads of the FCU. The ulnar nerve usually supplies the FCU in three or four branches.
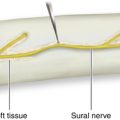
• The dorsal branch is sensory in nature. It winds around, deep to the FCU tendon, to gain the extensor surface.
Ulnar Nerve at the Wrist
• At the wrist level, both the ulnar nerve and the ulnar artery course lateral to the pisiform bone, passing under a fibrous band. The ulnar nerve then travels through the Guyon canal.
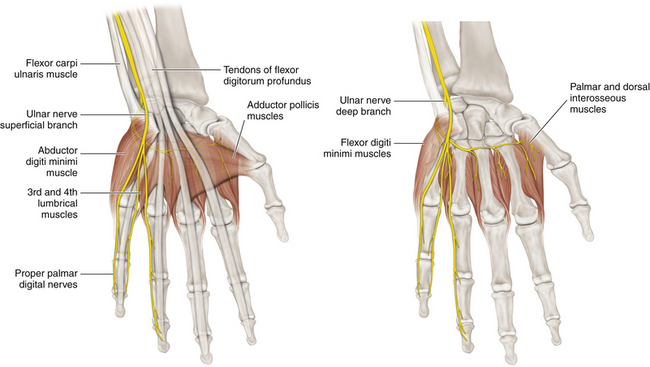
• At the level of the distal border of the flexor retinaculum, the ulnar nerve divides into superficial and deep branches (Figure 12-9). The superficial branch gives off cutaneous branches to the anterior surfaces of the medial one and a half digits. The deep branch supplies hypothenar muscles, the medial two lumbricals, and all the interossei, and ends in the adductor pollicis. The deep branch hooks around the hook of the hamate and then runs laterally.
Surgery: Arm and Elbow
Skin Incision
• The skin incision is over the course of the nerve. If it is carried into the forearm, the distal end of the cut is brought anterior to the epicondyle. (The incision can be made directly over the nerve in the notch but must not be positioned so as to result in a tender scar when the patient rests the elbow joint on a hard surface.)
Dissection in the Distal Arm
• The ulnar nerve lies beneath the upper arm fascia and deep to the edge of the intermuscular septum. This investing fascia needs to be opened to expose the nerve.
• Branches to the underlying FCU and elbow joint and collateral vessels may tether the nerve just proximal to the olecranon notch. These small sensory connections may require section to mobilize the nerve at this level. (Check for a proximal motor branch by stimulation.)
• If the nerve is to be transposed, the medial intermuscular septum must be cut down to the humerus so that the nerve does not become kinked as it moves forward from the extensor to the flexor compartment of the arm in its new routing.
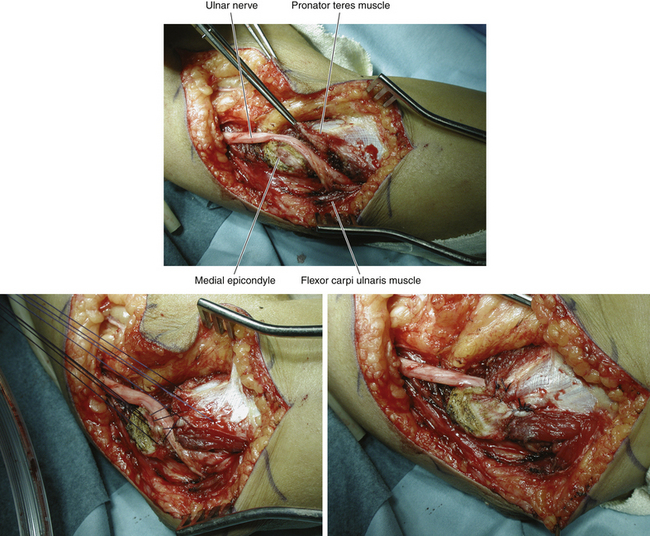
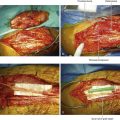
• When the ulnar nerve is exposed at the level of the distal arm, the nerve can be displaced by a Penrose drain. Medial antebrachial cutaneous nerve branches can be dissected free and encircled by plastic loops. Distally, the two heads of the FCU are split to expose the nerve at the proximal forearm level.
Dissection in the Olecranon Notch and Proximal Forearm
• Distal to the olecranon notch, the nerve runs under the two heads of the FCU, which are split over the course of the nerve (Figure 12-10).
• At this level the nerve sends branches to the FCU, which can be dissected either distally or back into the main nerve to provide length and preserve the branches during transposition.
• About 1 to 1½ inches distal to the olecranon notch, branches to the flexor profundus (ulnar half) arise from the lateral inferior portion of the nerve and need to be preserved.
Transposition
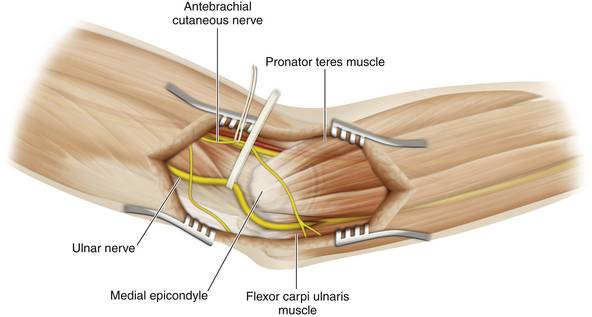
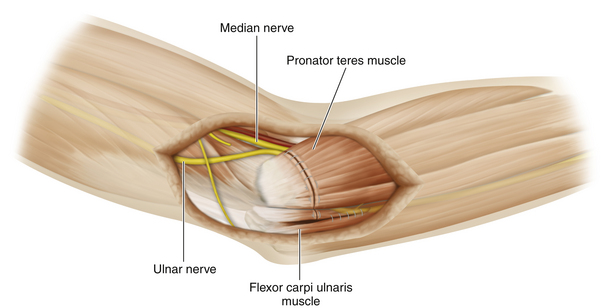
There are a wide variety of opinions as to what constitutes the appropriate operation for ulnar neuropathy at the elbow joint (Figures 12-11 and 12-12). These range from limited access surgery through complex transposition procedures. The following description is of a procedure at the latter end of this continuum.
1. The radial border of the pronator teres is freed for several inches distally, which usually exposes the elbow and proximal forearm portion of the median nerve. Antebrachial cutaneous branches are usually resected. The more proximal pronator teres is also dissected. The brachial artery and vein are usually encountered during this step and require preservation; smaller vessels can be coagulated or ligated if necessary.
2. A thorough neurolysis of the nerve is done, and the dissection is extended distally. The proximal site of section of the antebrachial cutaneous branch is cauterized. A trough is then made by sectioning, usually with a No. 10 scalpel blade, through the pronator teres and proximal FCU, 1 inch or so to the radial side of the medial epicondyle. The muscles are sectioned down to the finger flexor muscle mass but not through those muscle fibers.
3. The superficial head of pronator teres is completely sectioned and then undermined distally, taking care to preserve the pronator and deeper flexor branches from the median nerve supplying it.
4. The FCU is undercut distally, and its proximal free edge is also undercut back to the olecranon.
5. Some of the fibrous origin of the pronator teres from the medial epicondyle is released so that it can be moved laterally and toward the radial side of the forearm to reach the disconnected pronator and FCU.
6. The ulnar nerve is transposed deep to the transected pronator muscle. A scalpel, or electrocautery, is used to free some of the origin of the pronator to assist in repair of that muscle.
7. It is important that the course of the transposed nerve be smooth and graceful, without angulation or potential kinks with elbow flexion or extension.
8. The disconnected muscle is then brought back to the partially released soft tissues on the medial epicondyle by bringing it more inferiorly than its original location to make up some length and to provide a transposition site for the ulnar nerve that is not tight.
9. Then the fascia with muscle is closed by a series of locking sutures after a “bump” of folded towels or sheets is placed beneath the wrist and hand to provide a little elbow and wrist flexion so the muscular repair is not under great tension.
10. FCU branches are sometimes dissected back along the more proximal nerve to provide enough length for the transposition. If one antebrachial cutaneous branch is preserved, the other may be sectioned.
11. The FCU is also repaired, although it is not always possible to bring some of the sectioned FCU back to the medial epicondyle. The forearm portion of the FCU over the ulnar nerve, however, can usually be closed without too much tension.
12. A less extensive procedure entails cutting a trough in the superficial head of the pronator teres and maintaining the nerve in that position by a small fascial flap. The brachial artery and median nerve are not seen in this procedure (Figure 12-13).
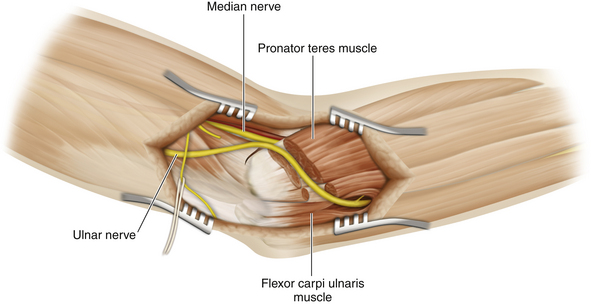
Figure 12-11 The ulnar nerve has been transposed and placed in a trough created in the common flexor mass.
Surgery: Wrist and Hand
1. The incision is usually made over the FCU tendon proximal to the wrist.
2. The incision is longitudinal and runs distally to the wrist crease; it then runs in the crease a short distance toward the thumb and finally crosses into the palm in a curvilinear fashion, heading over the hypothenar eminence.
3. The incision is deepened, and dissection is carried through subcutaneous tissues until the radial edge of the FCU is found.
4. A plane along and beneath the radial edge of the FCU is developed until the ulnar nerve, which tends to be under the FCU at this level, is found. The nerve is then dissected out and encircled by a Penrose drain.
5. The ulnar nerve is traced across the wrist to where it enters the Guyon canal, which is situated between the pisiform bone (a sesamoid bone in the FCU tendon) and the hook of the hamate. The medial boundary is the pisiform bone, and, more distally, the lateral boundary is the hook of the hamate.
6. The artery and vein travel with the nerve, and branches of these vessels sometimes lie superficial to the canal.
7. Tracking the deep branch beyond the Guyon canal is not an easy matter, because it runs deep to the flexor tendons and the deep palmar arterial arch. Exposure at this level requires a careful and patient dissection with magnification.
8. It helps to dissect out and mobilize the nerve from the ulnar artery as completely as possible. This is best done at the wrist level.
9. The key point is to release the entrapment point where the deep branch winds around the hook of the hamate and is indented by the fibrous margins of the overlying hypothenar muscles. Once released, the nerve runs without tension across the deep aspect of the hand.