U
Uhthoff’s symptom Temporary blurring of vision occurring when there is an increase in body temperature (e.g. during or following exercise) in patients with multiple sclerosis, optic neuritis and other optic neuropathies. The symptom may also occur as a result of emotional stress, menstruation, increased illumination or a hot bath. Uhthoff’s symptom is sometimes considered to be a prognostic indicator of multiple sclerosis in patients with idiopathic optic neuritis. Syn. Uhthoff’s phenomenon; Uhthoff’s sign; Uhthoff’s syndrome.
ulcer A localized lesion of the skin or of a mucous layer in which the superficial epithelium is destroyed and deeper tissues are exposed.
See abscess.
corneal u. A superficial loss of corneal tissue as a result of infection that has led to necrosis. It may be caused by a bacterium (e.g. Pseudomonas aeruginosa, Streptococcus pneumoniae), by a virus (e.g. herpesvirus), or by a fungus (e.g. Candida, Aspergillus, Penicillium). It causes pain and usually reduced visual acuity, especially if the ulcer occurs in the centre of the cornea. Corneal ulcers usually look dirty grey or white and are opaque areas of various sizes and a mucopurulent discharge may be present. If induced by contact lenses, especially extended wear lenses, patients must cease wearing their lenses immediately, and the appropriate therapy instituted: antibacterial, antifungal or antiviral agent.
See corneal facet; keratitis, herpes simplex; keratitis, hypopyon; keratitis, rosacea; keratitis, ulcerative; keratocele; keratomycosis; leukoma.
dendritic u. See keratitis, herpes simplex.
von Hippel’s internal u. A depression noted in the posterior surface of the cornea. This lesion resembles posterior lenticonus, except that it is thought to be due to an infection or inflammation. The lesion can be differentiated from Peter’s anomaly by the presence of endothelium and Descemet’s membrane in the former. Due to its posterior location, the lesion does not usually disturb visual function.
See Peter’s anomaly.
marginal corneal u. Benign condition due to a hypersensitivity reaction to bacterial conjunctivitis, particularly staphylococcal blepharoconjunctivitis. It is characterized by infiltration of the peripheral cornea by white cells and by ocular irritation. The condition is usually self-limiting but painful. Treatment includes frequent cleaning of the eyelid margin with a cotton-tipped applicator or face cloth or cotton ball with baby shampoo, warm compresses, antibiotic ointment and occasionally topical corticosteroids.
Mooren’s u . A rare, superficial ulcer of the cornea of unknown origin. It starts near the limbus as an overhanging advancing edge that in severe cases spreads over the entire cornea and may even invade the sclera. The patient complains of pain and blurred vision. There are two types: a self-limiting form, usually unilateral, affecting old people, and a progressive form, bilateral, affecting young people. The condition is difficult to treat and this may include topical and systemic steroids, immunosuppressants, or conjunctival excision.
See keratitis, peripheral ulcerative.
serpiginous u. See keratitis, hypopyon.
shield u. A localized corneal ulcer noted in severe cases of vernal conjunctivitis. The lesion is usually oval or pentagonal resembling a warrior’s shield. It is located in the upper portion of the cornea as a result of irritation from the large papillae on the palpebral surface of the overlying eyelid.
ulcerative keratitis See keratitis, ulcerative.
ultrafiltration One of the mechanisms that produce aqueous humour from blood plasma into the ciliary epithelium of the ciliary processes. This mechanism takes advantage of the natural pressure gradient between the capillary vascular pressure and intraocular aqueous pressure, to drive fluid into the eye. Ultrafiltration is one of three physiological processes that create aqueous fluid, the others being active transport and diffusion.
See ciliary body; diffusion; humour, aqueous rate of outflow, transport, active.
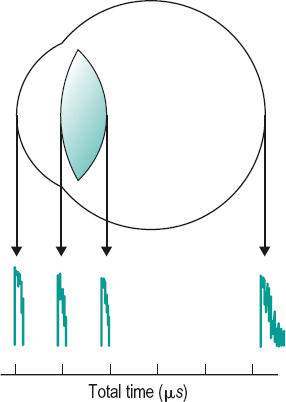
ultrasonography A technique utilizing high frequency ultrasound waves (greater than 4 MHz) emitted by a transducer placed near the eye. The silicone probe, which rests on the eye, is separated from the transducer by a water column to segregate the noise from the transducer. The technique is used to make biometric measurements such as the axial length of the eye, the depth of the anterior chamber, the thickness of the lens, the distance between the back of the lens and the retina, the thickness of the cornea and detect ocular pathology. The ultrasound wave is reflected back when it encounters a change in density of the medium through which it is passing. The reflected vibration is called an echo. Echoes from the interfaces between the various media of the eye are converted into an electrical potential by a piezoelectrical crystal and can be displayed as deflections or spikes on a cathode-ray oscilloscope.
There are two basic techniques used for examination: a contact system (often referred to as applanation) described above in which the probe is in contact with cornea and an immersion system in which the transducer and the cornea are separated by a water bath. This latter method eliminates the risk of indentation of the cornea and underestimation of the anterior chamber depth and axial length. Two types of ultrasonographic measurements are used: (1) The time-amplitude or A-scan which measures the time or distance from the transducer to the interface and back. Thus echoes from surfaces deeper within the eye take longer to return to the transducer for conversion into electrical potential and so they appear further along the time base on the oscilloscope display. The A-scan is useful for the study of the biometric measurements, as well as measurements of intraocular tumour size (e.g. choroidal melanoma) (Fig. U1). (2) The intensity-modulated or B-scan in which various scans are taken through the pupillary area and any change in acoustic impedance is shown as a dot on the oscilloscope screen, and these join up as the transducer moves across a meridian. The B-scan is useful to indicate the position of a retinal or vitreous detachment, or of an intraocular foreign body or a tumour, and for the examination of the orbit. The B-scan is especially useful in the examination of the posterior structures of the eye when opacities prevent ophthalmoscopic examination (e.g. cataract, corneal oedema). Syn. echography.
See biometry of the eye; length of the eye, axial.
ultraviolet (UV) Radiant energy of wavelengths smaller than those of the violet end of the visible spectrum and longer than about 1 nm. The wave band comprising radiations between 315 and 380 nm is referred to as UV-A. Excessive exposure to these radiations can cause cataract. The wave band comprising radiations between 280 and 315 nm is referred to as UV-B. Excessive exposure to all these radiations can cause photokeratitis and corneal opacity, while radiations between 295 and 315 nm can cause cataract. The wave band comprising radiations between 200 and 280 nm is referred to as UV-C. Excessive exposure to these radiations can cause photokeratitis and corneal opacity.
See blepharospasm; keratoconjunctivitis, actinic; laser, excimer; lens, absorptive; nanometre; pinguecula; wavelength.
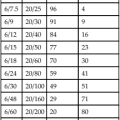
Table U1
Divisions of the ultraviolet spectrum
| UV-A (near) | 380–315 nm |
| UV-B (middle) | 315–280 nm |
| UV-C (far) | 280–200 nm |
umbo An area (0.15 mm–0.20 mm) in the centre of the foveola. Stimulation of this area results in the highest visual acuity.
umbra See penumbra.
unaided vision; visual acuity See acuity, unaided visual.
uncompensated heterophoria See heterophoria, uncompensated.
uncrossed diplopia See diplopia, homonymous.
undercorrected spherical aberration See aberration, spherical.
undercorrection A term applied to a corrective lens prescription of slightly lower power than required. It has been prescribed in an unsuccessful attempt to slow the progression of myopia in children because it reduces the accommodative stimulus.
See defocus, myopic; myopia control.
unharmonious retinal correspondence See retinal correspondence, abnormal.
uniocular See monocular.
unoprostone isopropyl See prostaglandin analogues.
upbeat nystagmus See nystagmus.
upgaze Movement of the eyes upward with the head in the straight-ahead position.
See elevation of the eye.
urea See hyperosmotic agent.
use-abuse theory See theory, use-abuse.
Usher’s syndrome See syndrome, Usher’s.
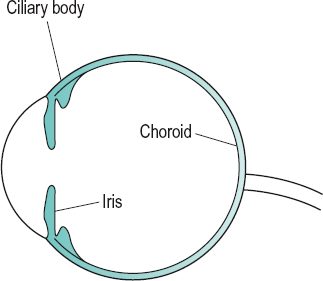
uvea The vascular tunic of the eye, consisting of the choroid, ciliary body and the iris. The last two structures are usually considered to form the anterior uvea. The uvea contains most of the blood supply (Fig. U2). Syn. uveal tract; vascular tunic of the eye.
uveal effusion syndrome See syndrome, uveal effusion.
uveal melanoma See melanoma, uveal.
uveal meshwork See meshwork, trabecular.
uveal tract See uvea.
uveitis Inflammation of the uvea. All three tissues of the uvea tend to be involved to some extent in the same inflammatory process because of their common blood supply. However, the most severe reaction may affect one tissue more than the others as in iritis, cyclitis or choroiditis or sometimes two tissues, e.g. iridocyclitis. The symptoms also vary depending upon which part of the tract is affected. Acute anterior uveitis is accompanied by pain, photophobia and lacrimation and some loss of vision because of exudation of cells (aqueous flare), protein-rich fluid and fibrin into either the anterior chamber or vitreous body, as well as ciliary injection, adhesion between the iris and lens (posterior synechia), miosis and keratic precipitates. The condition is often associated with ankylosing spondylitis, rheumatoid arthritis, sarcoidosis, syphilis or tuberculosis (usually with granulomatous uveitis). It is the most common form of uveitis. Many cases are HLA-B27 positive. Treatment includes corticosteroids and mydriatics to reduce the risk of posterior synechia and to relieve a spasm of the ciliary muscle.
See arthritis, juvenile idiopathic; disease, Reiter’s; nodules, Busacca’s; nodules, Koeppe’s; ophthalmia, sympathetic; syndrome, Behçet’s; phthisis bulbi; synchisis scintillans; syndrome, Vogt–Koyanagi– Harada; Table I6.
fungal u. Uveitis caused by a fungus such as Candida albicans, Cryptococcus neoformans and Histoplasma capsulatum. It is often accompanied by other disorders (e.g. choroiditis, retinitis). It may have spread from other bodily tissues (e.g. skin, mouth, gastrointestinal tract) in patients who are intravenous drug addicts, patients with indwelling venous catheters or patients who are immunosuppressed.
intermediate u. A chronic inflammation of the ciliary body (cyclitis) or its pars plana zone (pars planitis) or of the peripheral retina and vitreous (peripheral uveitis). The cause is unknown in most cases but others are associated with systemic conditions such as multiple sclerosis, sarcoidosis or HIV infection. It affects mainly young adults and is bilateral in about 80% of cases. Symptoms are floaters and, sometimes, blurred vision, and there may be anterior chamber cells and flare. Ophthalmoscopic examination may show vitreous condensation and gelatinous exudates (‘cotton balls’ or ‘snowballs’). Snowbanking, i.e. a whitish plaque or exudates involving the pars plana, often the inferior part of it, appears mainly in pars planitis. Intermediate uveitis may be associated with retinal vasculitis (i.e. inflammation of a retinal blood vessel). In a few cases the condition is self-limiting within a few months. However, in most cases the condition lasts several years may lead to complications such as cystoid macular oedema, posterior subcapsular cataract, retinal detachment or cyclitic membrane formation. Treatment includes corticosteroids and in resistant cases immunosuppressive agents.
posterior u. A uveitis involving the posterior segment of the eye. Symptoms include floaters and visual loss if the choroiditis involves the macular area. Ophthalmoscopically there is an accumulation of debris in the vitreous and choroidal lesions appear as yellow-white areas of infiltrates surrounded by normal fundus. Retinitis is also present in most cases, as well as retinal vasculitis. Posterior uveitis may be associated with AIDS, Behçet’s disease, Lyme disease, histoplasmosis, sarcoidosis, toxoplasmosis, syphilis, tuberculosis, Vogt–Koyanagi–Harada syndrome, sympathetic ophthalmia, etc.
viral u. Uveitis caused by a virus. Common viruses are: herpes simplex, which is usually associated with keratitis and may cause anterior uveitis; herpes zoster which may also be associated with keratitis; human Tcell lymphotrophic virus; measles; cytomegalovirus; rubella; human immunodeficiency virus (HIV).
See blepharoconjunctivitis, herpes simplex; herpes zoster ophthalmicus.
uveoscleral pathway See pathway, uveoscleral.