Chapter 45 Tumescent local anesthesia for liposuction
• Tumescent local anesthesia (TLA) leads to pain reduction and hydrodissection to result in a more predictable outcome.
• TLA leads to homogenization of fat tissue.
• The Hamburg formula is recommended today.
• Two different kinds of local anesthetic drugs reduce the risk of toxicity by half.
• Infiltration speed = 200 ml/min.
• A maximum of 10 liters can be infiltrated in an 80 kg patient.
• Hydrodissection allows fat debulking under anatomical considerations in different levels.
Historical Background
In 1985 Jeffrey Klein, a dermatologist from San Juan Capistrano, California, performed his first case using the original TLA formula (Table 45.1). Dr. Klein is trained also in internal medicine, pharmacology, biostatistics and mathematics.
| Original Tumescent Anesthesia Formula (Described by Jeffrey Klein) | |
|---|---|
| lidocaine 1% | 50.0 ml |
| bicarbonate 8.4% | 6.0 ml |
| epinephrine (1 : 1000) | 1.0 ml |
| (triamcinolone 10 mg | 1.0 ml) |
| NaCl 0.9% | 1000.0 ml |
| __________ | |
| ~0.0475 (0.05%) % concentration | 1028.0 ml |
Today1 we use the term “tumescent local anesthesia” (TLA). The formula is composed of a combination of a local anesthetic drug (short acting), epinephrine, bicarbonate, and optional triamcinolone, diluted in physiologic saline solution. Today we use the so called “Hamburg Formula”, which has been described by Friedrich and Schneider-Affeld (Table 45.2).
| Tumescent Local Anesthesia Formula (Preparation Described by Schneider-Affeld and Friedrich) | |
|---|---|
| lidocaine 2% | 10.0 ml |
| prilocaine 2% | 10.0 ml |
| bicarbonate 8.4% | 6.0 ml |
| epinephrine (1 : 1000) | 0.7 ml |
| (triamcinolone 10 mg | 1.0 ml) |
| NaCl 0.9% | 1000.0 ml |
| __________ | |
| ~0.038 % concentration | 1027.7 ml |
The subcutaneous infiltration of large volumes of this formula causes the targeted tissue to become swollen and firm, or tumescent, and permits procedures to be performed on patients without general anesthesia while minimizing blood loss due to the vasoconstrictive effect of epinephrine2 and also reduces the resorption of the local anesthesia drug in order to avoid lidocaine toxicity.
Prilocaine is metabolized in the liver but also in the kidneys and the lungs.
Preoperative Preparation
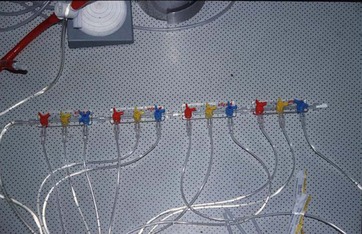
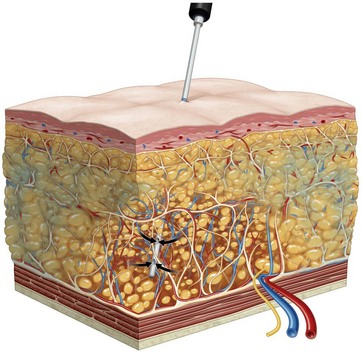
The prepared bags of TLA solution are connected to an infusion pump which should be able to determine the speed of infiltration, currently infiltrated amount, and maximum amount of fluid. Preferably the solution should be preheated, at least to room temperature. While the infiltration process is ongoing the patient should be kept in warm blankets and supplied with a warm air system. Blunt or sharp cannulas can be used as infiltration devices; these are called rainbow cannulas. We use a sharp needle system using 12 outlets simultaneously so a slow administration of fluid can be accomplished in an acceptably short period of time (Fig. 45.1). At an infiltration speed of 200 ml/min, 10 liters of TLA fluid can be infiltrated in about 50 minutes (Fig. 45.2 and Box 45.1).
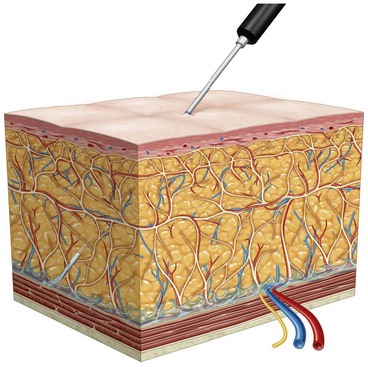
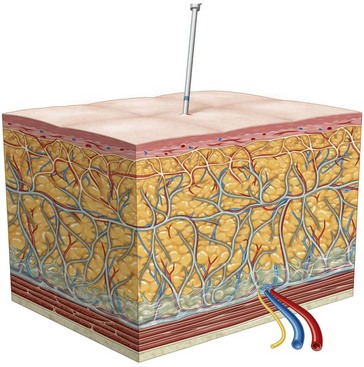
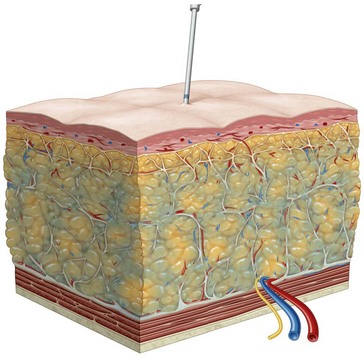
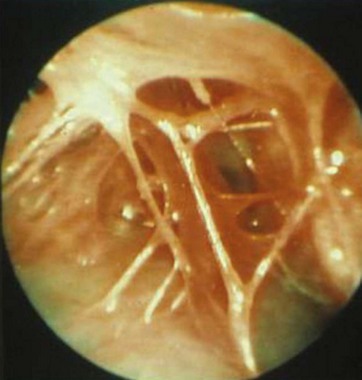
A quick manner of fluid infiltration will lead in the first step to an “interseptal hydrodissection” (Fig. 45.3), since these tissue planes offer the lowest resistance for the TLA fluid to spread. After a short time, depending on the rising interstitial tissue pressure, the TLA fluid will penetrate the fascias and will surround the fat lobules, which we call “paralobular distribution” (Fig. 45.4). Increasing amounts of fluid will cause the fat lobules to absorb the TLA fluid. This stage is called the “intralobular penetration” (Fig. 45.5). After more and more fluid is added, the complete extent of all the fat levels is flooded by the TLA fluid, which after 30 minutes of diffusion we call the “state of tumescence” (Fig. 45.6).
Surgical Technique
Furthermore, the hydrodissection of the subcutaneous space separates the horizontal fascia planes from the different fat compartments. This allows the surgeon to perform a fat debulking procedure under anatomical considerations at different levels (Fig. 45.7).
Optimizing Outcomes
In regard to safety, TLA demonstrates the issues of local anesthesia. There is always a range of action. This disadvantage in regard to safety is a very important point. A potential injury from perforation of the underlying structures (such as the abdominal wall) by the liposuction cannula would be noticed by the patient immediately, so undesired injuries can be prohibited before they even happen. Also, the softening effect on the fat by the TLA fluid severely reduces the force needed to push the liposuction cannula forward. This increases the surgeon’s control of his own fine-motor-sensitivity (Fig. 45.8).
After a liposuction under TLA, the situation of open drainage will occur; having extensive amounts of saline solution present in the surgical area has an exceptional advantage. Blood will not coagulate in the presence of saline solution and therefore the postoperative liposuction period will show a pronounced wash-out situation with the open drainage of reddish-colored fluid through the distal incisions of the surgical field. This leads to less bruising, less pain, and less swelling, as well as a lesser potential for infection during the postoperative period (Fig. 45.9).
Complications and Contraindications
Breuninger H. Geschichte der Tumeneszenz-Anästhesie. Akt Dermatol. 2009;35:290–292.
Grassegger A, Haussler R. [Is the use of tumescence anesthesia in general anesthesia contraindicated?]. Anaesthesist. 2001;50(10):794.
Hanke CW, Sattler G, Sommer B. Textbook of Liposuction. Informa Healthcare. 2007.
Hempel V. [Is the use of tumescence anesthesia in general anesthesia contraindicated?]. Anaesthesist. 2001;50(5):363–364.
Klein JA. The tumescent technique for liposuction surgery. Am J Cosmet Surg. 1987;4:263–267.
Sattler G, Sommer B, Hanke CW. Lehrbuch der Liposuktion. Georg Thieme Verlag; 2003. 1. Auflage
Selzle KET, Kamionek I, Kuropka R, Schonath M. [Tumescence local anesthesia in venous surgery]. Zentralbl Chir. 2001;126:517–521.
Weinberg GL, Laurito CE, Geldner P, et al. Malignant ventricular dysrhythmias in a patient with isovaleric acidemia receiving general and local anesthesia for suction lipectomy. J Clin Anesth. 1997;9:668–670.