Trunk stability
What is trunk stability?
The terms trunk/central and spinal stability are synonymous and are used interchangeably in clinical practice. Core stability is the equivalent lay term. In essence, trunk stability is a reflection of an individual’s postural control, the ability to orientate and stabilize the body using appropriate balance strategies and responses (Raine et al. 2009). As such, trunk stability is an essential core component of balance, the ability to maintain the centre of mass (COM) within the base of support (BOS) (S3.32) and functional activities, by which it provides proximal stability to allow for the coordinated free movement of the limbs and head (2; 12). Trunk stability is also important in controlling and supporting the spinal segments, so reducing the stresses upon soft tissue structures and helping to avoid injury and pain.
This section will focus upon the core trunk muscles which are commonly divided into two groups according to their functional anatomy (Bergmark 1989):
The local stabilizers
These muscles are anatomically deep and have attachments to each individual spinal vertebra. This allows them to act at a segmental level (between adjacent vertebrae) providing a strong basis for trunk stability. The local stabilizers are composed primarily of Type I (slow oxidative fibres) muscle fibres, which produce low forces but are fatigue resistant. These muscles therefore function as postural muscles. They also have smaller motor units which are easily activated due to their low neural threshold and therefore tend to be recruited first (Henneman principle) during functional activities. In theory, this means that the local stabilizers are activated prior to the surrounding global muscles which have larger motor units. This pre-setting of trunk stability is crucial in providing a stable base upon which limb movement can be based and may be part of an anticipatory response to a perceived COM displacement (MacDonald et al. 2006). The anticipatory activation will be built into a learned movement plan.
The anatomical and physiological features of the local muscle stabilizers make them perfectly adapted to perform their specific trunk stability function, however the nervous system also influences the fine control of these muscles. The force of contraction required to provide segmental stability is estimated to be 3% of maximum contraction (Cholewicki and McGill 1996). As antigravity postural muscles, this background level of activity is controlled by the vestibular and reticular systems (S2.10).
The balance of activity between the abdominal (TAb/IOf) and back extensor (MT) pair is vital in terms of the level and timing of activation. A neutral position of the pelvis and lumbar spine is considered to be highly correlated with the co-contraction of this muscle pair (O’Sullivan 2006). In postures of either anterior pelvic tilt with lumbar spine hyperextension or posterior tilt with lumbar spine flexion the local muscles are switched off and over time become deconditioned (O’Sullivan 2006). This is highly relevant in a population of neurologically impaired patients who often spend many hours sitting in poor postures in inadequate seating.
Why do I need to assess trunk stability?
Trunk instability results in less efficient movement, a limited ability to explore the environment (Cristea et al. 2003) and demands compensatory muscle activity to maintain an upright position. The latter may present as abnormal fixation of the trunk or, in extreme cases, excessive use of the upper limbs, and leads to effortful movement for the individual. Poor trunk stability resulting in deviations in posture may also cause abnormal stresses and potential damage to soft tissue structures leading to pain and further functional loss. Often rehabilitation focuses on improving general trunk stability without specific attention to the interaction between the local and global stabilizers. More focus on segmental stability initially may have the potential to improve the movement sequences and the functional outcome for the individual.
In a neurologically impaired patient, poor trunk stability has been linked with a poor functional outcome in multiple sclerosis (Lanzetta et al. 2004), cerebrovascular accident (CVA) (Hsieh et al. 2002) and Parkinson’s disease (PD) (Dibble and Lange 2006; Nardone and Schieppati 2006).
In CVA, trunk instability has also been linked with poor postural control in standing (Palmer et al. 1996; Slijper et al. 2002) and in sitting (Dickstein et al. 2004) and is viewed as a negative prognostic indicator for recovery. Proprioception (position sense) (Mergner et al. 2003; Peterka 2002) and reduced strength (Karatas et al. 2004) in the trunk have been found to be causal in CVA (Ryerson et al. 2008) and in PD (Vaugoyeau et al. 2007).
How do I assess trunk stability?
Observation during functional activities
Patient
Any trunk instability may have already been noted during the second section of the objective assessment (S3.18). However, as the demands on trunk stability appear to be task specific the therapist should ensure they have investigated a range of functional activities.
Therapist
The therapist observes the patient during a functional activity.
How much postural sway is observed in a static position? The normal excursion of postural sway should be very small, occurring in response to the action of gravity and breathing perturbations. If the movements are large, this could indicate trunk instability.
Does this postural sway deteriorate with eyes closed? This could indicate insufficient sensory feedback as a cause of instability.
Do they have difficulty achieving tasks using their upper limbs? They may be using their arms to fix and therefore will be reluctant to use them during functional activities.
Do they lose balance during tasks? Yes, this may indicate trunk instability.
Is there excessive trunk movement when:
Performing any functional activity? Yes, these may indicate trunk instability.
Do they have difficulty with lower limb placement during swing phase? Scissoring may reflect the inability to place the foot accurately because of an unstable trunk in contralateral stance.
Do they use any compensatory fixation? This may involve limbs or fixation/excessive stiffness through the trunk and may indicate trunk instability or a lack confidence to move.
Assessment of the local muscle stabilizers
Therapist: observe and palpate
1. Initially the patient’s position should reflect their posture of choice, in order for the therapist to assess the trunk stabilizers under normal circumstances.
2. Ask the patient to perform a limb movement in order to challenge the trunk stabilizers. This could include one arm being lifted (shoulder flexion or abduction), two arms being raised or one leg being lifted (hip flexion or abduction). The amount the limb is moved will depend on the ability of the individual. In some cases the ability to raise a hand 2 inches may be very challenging.
3. Observe and then palpate the local stabilizers to evaluate the state of contraction.
a. Multifidus (MT): Palpate for MT just medial to the posterior superior iliac spine (PSIS) (Fig. 25.1).

Figure 25.1 Palpation for multifidus.
b. Transversus abdominus (TAb): Palpate 1 inch medially and 1 inch inferiorly from the anterior superior iliac spine (ASIS) (Fig. 25.2).

Figure 25.2 Palpation for transversus abdominus.
Can they activate the local muscle stabilizers during the task? Or do they primarily use a global muscle contraction to gain stability.
Can they maintain the contraction? If they can recruit the local stabilizers, do they have good muscle endurance? If not, this may lead to trunk instability linked to muscle weakness or fatigue.
Is there appropriate co-contraction of the local stabilizers? There should be simultaneous contraction of MT and TAb but the degree of contraction of each will be dictated by the task requirements. During a unilateral limb movement the contralateral pair of stabilizers (MT and TAb) should contract more strongly and in a bilateral task there should be symmetry of contraction.
Do they activate the local stabilizers prior to limb movement? This is evidence of an anticipatory contraction. Poor sequencing of muscle recruitment may result in trunk instability and the need for compensatory strategies. However, in electromyographical (EMG) studies the anticipatory response is a fraction of a second and is unlikely to be identifiable in practice. Appreciation of a simultaneous activation is more realistic.
Do they use compensatory strategies? Common examples include breath holding, over use of the global stabilizers, excessive use of the shoulder elevators or hip adductors/flexors. These are strategies used to provide false stability.
Therapist: realign pelvis/lumbar spine
1. If no muscle contraction can be palpated with the patient in their posture of choice (Fig. 25.3) then the therapist should try altering the alignment of the patient’s pelvis/lumbar spine. A neutral alignment of the pelvis and lumbar spine is correlated with the preferential recruitment of the local stabilizer muscles (O’Sullivan et al. 2006).

Figure 25.3 Posture of choice (sitting).
2. The therapist should instruct or facilitate the patient towards a more neutral alignment (Fig. 25.4).

Figure 25.4 Neutral pelvis and lumbar spine (sitting).
Therapist: assessment of individual muscle components
Transversus abdominus (TAb)
a. To evaluate TAb, use crook lying (i.e. supine with knees bent up to 90°) (Fig. 25.5). The aim is to encourage an isolated contraction of TAb through the alignment of a neutral pelvis and lumbar spine.

Figure 25.5 Modified crook lying.
b. The instruction to the patient will be dependent on the initial position adopted by the individual. A patient who adopts crook lying with an anteriorly tilted pelvis and extended lumbar spine needs an instruction such as ‘flatten your back’ or ‘push your back down onto the bed’ or ‘pull your belly button in’. Whereas a patient who initially presents in posterior pelvic tilt and lumbar spine flexion will need to raise their back towards neutral.
c. A rolled towel (2 inches thick) placed under the patient’s back, at waist level (Fig. 25.5), allows for a larger movement by which to achieve neutral making the task easier for the patient to comprehend and feel.
d. Initially the therapist may ask the patient just to tighten these muscles (an isometric contraction).
e. If an isometric contraction can be initiated limb movements may be added in the same position to assess whether the contraction can be maintained during a challenge.
f. The therapist should then return to the observation and palpation assessment protocol and re-test.
Multifidus (MT)
a. To evaluate MT, use sitting. The aim is to focus on a contraction of MT through a neutral alignment of pelvis and lumbar spine.
b. From upright sitting the therapist instructs and/or facilitates a release of the lumbar spine into flexion. This allows for a larger movement to achieve neutral and is therefore easier for the patient to comprehend and feel (Fig. 25.6).
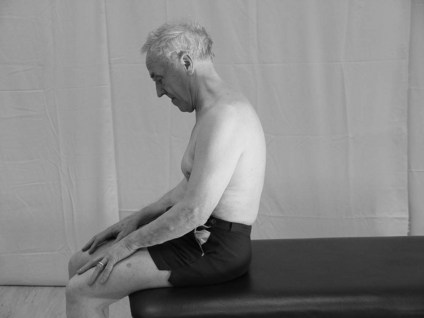
Figure 25.6 Preparation: Release of lumbar spine.
c. The patient is then guided towards a neutral sitting posture using facilitation. Simultaneously, the patient should attempt to activate the appropriate muscle while being given immediate accurate verbal feedback on the accuracy of recruitment from the therapist.
d. If an isolated contraction of MT is achieved, limb movements may be added in the same position to assess whether the contraction can be challenged.
e. The therapist should then return to the observation and palpation assessment protocol and re-test.
Analysis
The findings from an assessment of trunk stability should be considered in relation to other assessment tools (S3.19–34) and especially postural control/balance as the two are highly integrated. Analysis and synthesis of all this information may allow the therapist to predict a possible cause of the trunk instability.
References and Further Reading
Bergmark, A. Stability of the lumbar spine: a study in mechanical engineering. Acta Orthopaedica Scandinavica. 1989; 230(Suppl):20–24.
Brown, TD. Getting to the core of the matter. Strengthening and Conditioning Journal. 2006; 282:1524–1604.
Cholewicki, J, McGill, S. Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clinical Biomechanics. 1996; 11:1–15.
Cristea, MC, Mitnitski, AB, Feldman, AG, et al. Interjoint coordination dynamics during reaching in stroke. Experimental Brain Research. 2003; 1513:289–300.
Dibble, LE, Lange, M. Predicting falls in individuals with Parkinson disease: a reconsideration of clinical balance measures. Journal of Neurologic Physical Therapy. 2006; 30:60–67.
Dickstein, R, Sheffi, S, Markovici, E. Anticipatory postural adjustment in selected trunk muscles in post stroke hemiparetic patients. Archives of Physical Medicine and Rehabilitation. 2004; 85:228–234.
Hsieh, CL, Sheu, CF, Hsueh, IP, et al. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002; 33:2626–2630.
Karatas, M, Cetin, N, Bayramoglu, M, et al. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. American Journal of Physical Medicine and Rehabilitation. 2004; 83:81–87.
Lanzetta, D, Cattaneo, D, Pellegatta, D, et al. Trunk control in unstable sitting posture during functional activities in healthy subjects and patients with multiple sclerosis. Archives of Physical Medicine and Rehabilitation. 2004; 85:279–283.
MacDonald, DA, Moseley, GL, Hodges, PW. The lumbar multifidus: does the evidence support clinical belief? Manual Therapy. 2006; 11:254–263.
Marshall, P, Murphy, B. The validity and reliability of surface EMG to assess the neuromuscular response of the abdominal muscles to rapid limb movement. Journal of Electromyography and Kinesiology. 2003; 13:477–489.
Massion, J, Alexandrov, A, Frolov, A. Why and how are posture and movement coordinated? Progress in Brain Research. 2004; 1432:13–27.
Mergner, T, Mauer, C, Peterka, RA. Multisensory posture control model of human upright stance. Progress in Brain Research. 2003; 142:189–201.
Nardone, A, Schieppati, M. Balance in Parkinson’s disease under static and dynamic conditions. Movement Disorders. 2006; 21:1515–1520.
O’Sullivan, PB, Dankearts, W, Burnett, AF, et al. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain free population. Spine. 2006; 3119:E707–E712.
Palmer, E, Downes, L, Ashby, P. Associated postural adjustments are impaired by a lesion of the cortex. Neurology. 1996; 46:471–475.
Peterka, JR. Sensorimotor integration in human postural control. Journal of Neurophysiology. 2002; 883:1097–1118.
Raine, S, Meadows, L, Lynch-Ellerington, M. Bobath concept theory and clinical practice in neurological rehabilitation. Oxford: Wiley Blackwell; 2009.
Ryerson, S, Byl, NN, Brown, DA, et al. Altered trunk position sense and its relation to balance functions in people post-stroke. Journal of Neurologic Physical Therapy. 2008; 321:14–20.
Slijper, H, Latash, M, Rao, N, et al. Task specific modulation of anticipatory postural adjustments in individuals with hemiparesis. Clinical Neurophysiology. 2002; 113:642–655.
Vaugoyeau, M, Viel, S, Assaiante, C, et al. Impaired vertical postural control and proprioceptive integration deficits in Parkinson’s disease. Neuroscience. 2007; 146:852–863.