Trocar Placement
The most important prerequisite for proper trocar placement is knowledge of abdominal wall anatomy. Patient position is critical for a safe procedure. The patient is placed in the dorsal lithotomy position with foam-padded leg stirrups (Allen Medical Systems, Acton, Massachusetts), in which the calves and heels are supported and can be elevated for the vaginal portion of the surgery. The legs are checked for pressure points, and the arms are placed at the side wrapped in sheets and with cushions placed at pressure points.
An examination is performed with the patient under anesthesia, and the bladder is catheterized. For operative laparoscopy, a Foley catheter is left in the bladder. A uterine manipulator is inserted. For infertility cases, we use a RUMI (Cooper Medical, Oklahoma City, Oklahoma) or a Cohen manipulator (Eder Instruments, Oak Creek, Wisconsin).
Veress Needle Insertion
A local anesthetic, such as an equal mixture of 1% lidocaine without epinephrine and 0.25% bupivacaine, is infiltrated into the umbilical area. A 20-gauge, 2-inch needle is used so that the skin and fascia are infiltrated. The abdominal skin should be elevated while this procedure is performed.
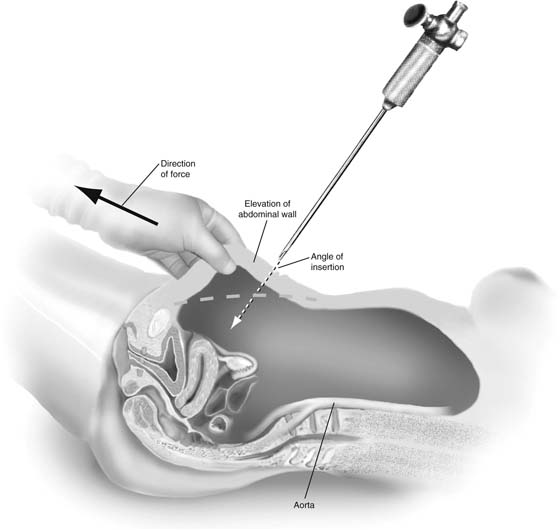
An orogastric tube should be inserted if intubation has been difficult or ventilation prior to intubation has been prolonged. A dilated stomach can be punctured easily under circumstances that result in gastric dilation. It is mandatory that the patient be kept in a horizontal position. An incision is made intraumbilically in the natural folds. It is a matter of preference whether a pneumoperitoneum is created before insertion of the primary trocar. Several articles have documented the safety of a direct trocar insertion without a pneumoperitoneum. Injuries to intraperitoneal structures such as the bowel and blood vessels have been clearly associated with Veress needle insertion. The abdominal wall should be elevated prior to insertion. If the bowel is adherent to the anterior abdominal wall, it will not move away with elevation. If the bowel is not adherent, it will be farther away from the needle. Vascular structures also will be farther away. The Veress needle should be aimed toward the uterus at a 45° angle and in the midline (Fig. 115–1). Before insufflating, correct intraperitoneal placement of the needle should be performed by one of these techniques:
 A drop of fluid placed on the needle hub will trickle downward, especially if the anterior abdominal wall is elevated.
A drop of fluid placed on the needle hub will trickle downward, especially if the anterior abdominal wall is elevated.
 A syringe of fluid can be attached to the needle and easily injected. This fluid can then be aspirated. If there is no return, the needle has been placed correctly. If there is return of blood or bowel content, there is a problem.
A syringe of fluid can be attached to the needle and easily injected. This fluid can then be aspirated. If there is no return, the needle has been placed correctly. If there is return of blood or bowel content, there is a problem.
 Gas flow can be started at 1 L/min. Pressure should be less than 10 mm Hg.
Gas flow can be started at 1 L/min. Pressure should be less than 10 mm Hg.
High-flow insufflators that deliver 9 to 15 L/min are necessary to compensate for the constant irrigation and suction of fluids, as well as the leaking of gas that may occur. Intraperitoneal pressure should not exceed 15 mm Hg. Higher pressures can cause decreased venous return or ventilation problems.
Primary Trocar Insertion
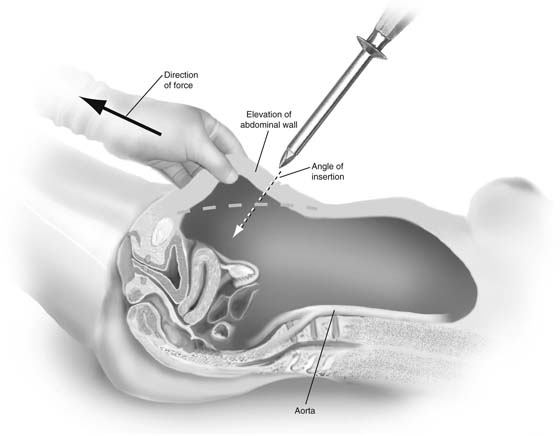
The primary trocar can be inserted with or without a pneumoperitoneum. If the direct trocar technique is used, correct placement is easily confirmed with introduction of the laparoscope. Either way, the abdominal wall should be grasped and elevated maximally, and with the other hand the trocar should be directed at a 45° angle and in the midline (Fig. 115–2). The patient must be kept in a horizontal position. In Trendelenburg’s position, the anatomic relationship of the major vessels to the angle of insertion is altered, which may increase the risk of injury. We usually use a blunt-tipped optical trocar for this step. A pyramidal tip incises the fascia, whereas the conical tip dilates it. More force is required for the latter trocar. Excessive force reduces control of the angle and depth of the trocar tip, increasing the risk of injury to internal structures. Resistance to trocar insertion also occurs if the skin incision is too small, or if the instrument is dull. Optical access trocars were recently introduced into the market. Two commercially available trocars are the Excel (US Surgical, Norwalk, Connecticut) and the OptiView (Ethicon, Somerville, New Jersey). Several small case series but no large randomized studies have shown that these trocars are associated with fewer injuries than are conventional techniques.
FIGURE 115–1 Insertion of the Veress needle should be performed with elevation of the anterior abdominal wall. The angle should be at 45° and in the midline.
FIGURE 115–2 Insertion of the primary trocar requires elevation of the abdominal wall. The other hand inserts the trocar at a 45° angle and in the midline.
Open Laparoscopy and Alternative Techniques
Open laparoscopy is the only technique demonstrated to eliminate large-vessel injury. However, bowel injury has been reported with this technique as well. A 2- to 3-cm horizontal infraumbilical incision is made, and the fascia is exposed. An incision is made horizontally, and a suture is placed at each angle (Fig. 115–3). A blunt-tipped Hasson-type trocar is then inserted (Fig. 115–4). With the advent of single port laparoscopy, several disposable devices are available and can be placed through this incision.
Alternative methods should be utilized in patients who have midline scars from previous abdominal surgery. An open technique with a Hasson trocar at the umbilicus or at a left upper quadrant site should be utilized. In the left upper quadrant technique, an incision is made 2 cm below the costal margin at the left midclavicular line. A Veress needle or a small trocar can be inserted. The angle should be 45° and in a longitudinal plane without deviation toward the midline. The closest organs that may be injured are the stomach and the left lobe of the liver. This procedure should not be performed in patients with hepatomegaly, splenomegaly, or left upper quadrant surgery. An orogastric tube should be placed before the trocar is inserted.
Secondary Trocar Insertion
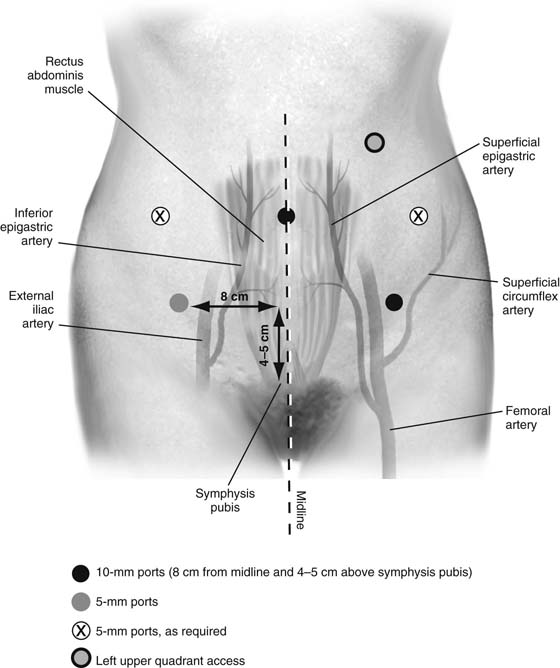
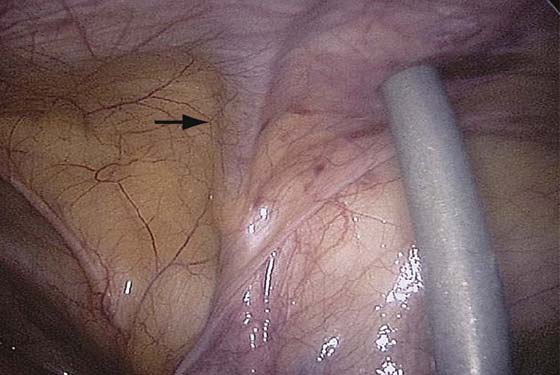
Secondary trocars for pelvic surgery are placed lateral to the rectus muscle or suprapubically under direct vision. Knowledge of the anterior wall anatomy is essential for proper accessory port placement (Fig. 115–5). The most important vessels to visualize are the inferior epigastric arteries and veins. Transillumination will not help to delineate these vessels. They are lateral to the obliterated umbilical vessels and medial to the deep inguinal ring, which can be found by following the entry of the round ligament into the inguinal canal (Fig. 115–6). We recommend placing trocars 8 cm from the midline and 4 to 5 cm above the symphysis pubis. Conical-tipped trocars are probably better for these secondary sites because they have been associated with decreased risk of vessel injury. The tip of the trocar should be aimed toward the cul-de-sac. At the end of the procedure, the trocar sites should be inspected for bleeding. All lower quadrant incisions of 7 mm or greater should be closed (Fig. 115–7).
FIGURE 115–3 Open laparoscopy technique: the skin and fat can be retracted with small S retractors. The fascia is incised, and a suture is placed at each angle.
FIGURE 115–4 The peritoneum is incised and the peritoneal cavity entered. A blunt-tipped trocar is inserted. The suture is then wrapped around the special grooves of the trocar.
FIGURE 115–5 Relationship of accessory port sites and the vessels of the anterior abdominal wall.
FIGURE 115–6 Correct placement of a trocar lateral to the inferior epigastric vessels (arrow).
FIGURE 115–7 This figure demonstrates the insertion of a fascial closure device (Karl Storz GmbH & Co KG, Tuttlingen, Germany) to close the defect. The suture is grasped within the instrument and is pushed through the superior part of the fascial defect.

 Mark D. Walters
Mark D. Walters