7 Tricuspid and Pulmonic Valve Disease 
Tricuspid Regurgitation
Scanning Issues
Required parameters to obtain from scanning include the following:
 Valve and RV details to explain the cause of the tricuspid regurgitation (TR)
Valve and RV details to explain the cause of the tricuspid regurgitation (TR)
 RV size and systolic function, and net forward cardiac index (CI) from the left ventricular outflow tract (LVOT)–velocity time interval (VTI) method
RV size and systolic function, and net forward cardiac index (CI) from the left ventricular outflow tract (LVOT)–velocity time interval (VTI) method
Scanning Notes
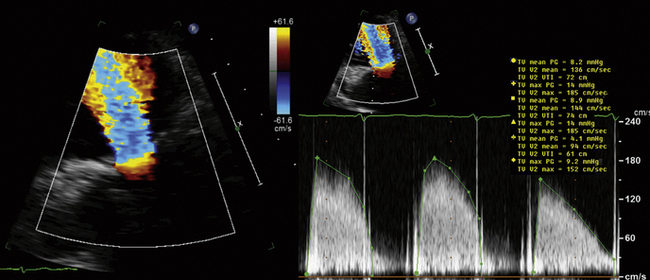
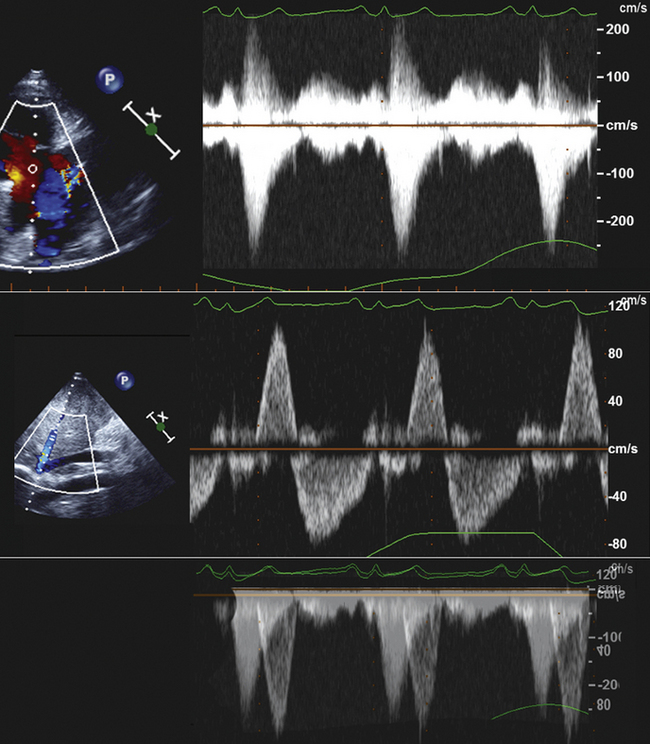
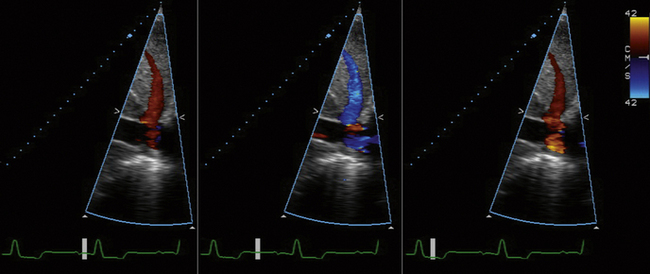
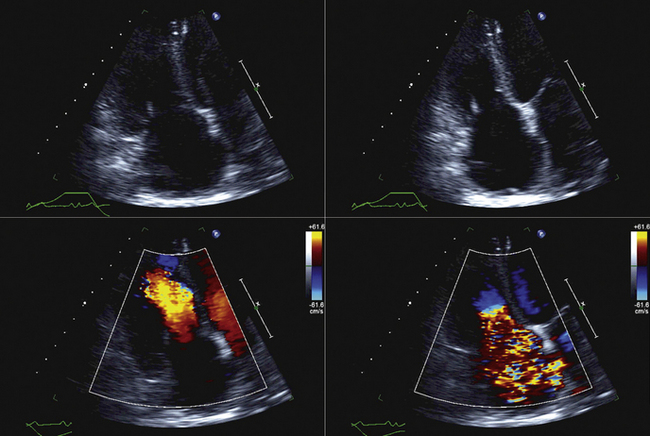
 There are problems with color Doppler “quantification” of TR, as there are for color Doppler flow-mapping of any lesions of insufficiency: TR flow-mapping is dependent on gain, angle, position, and jet shape and orientation.
There are problems with color Doppler “quantification” of TR, as there are for color Doppler flow-mapping of any lesions of insufficiency: TR flow-mapping is dependent on gain, angle, position, and jet shape and orientation.
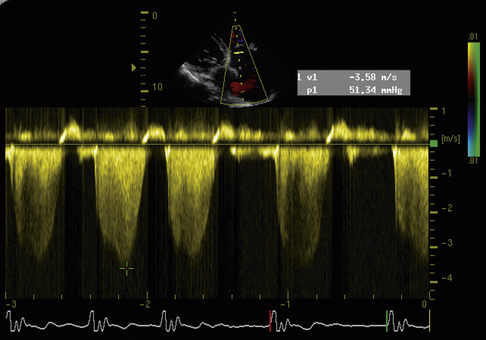
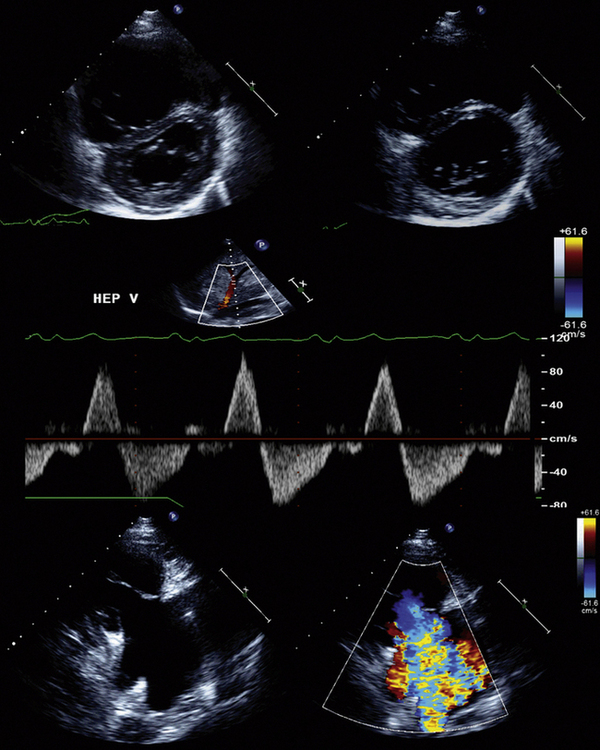
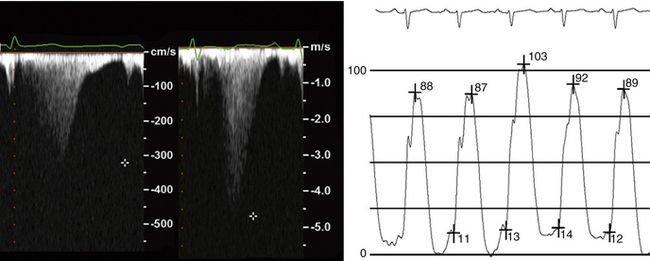
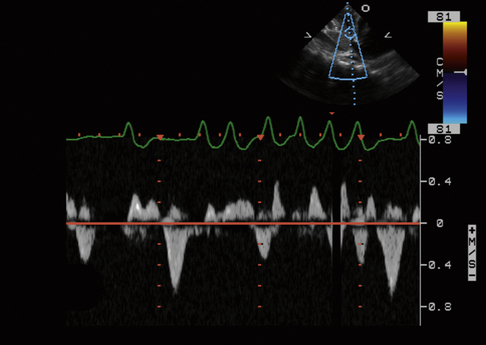
 Retrograde hepatic venous systolic flow reliably establishes that TR is severe.
Retrograde hepatic venous systolic flow reliably establishes that TR is severe.
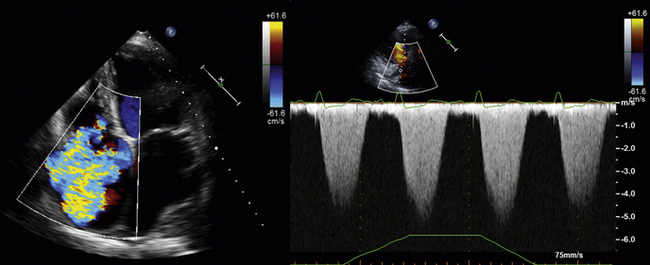
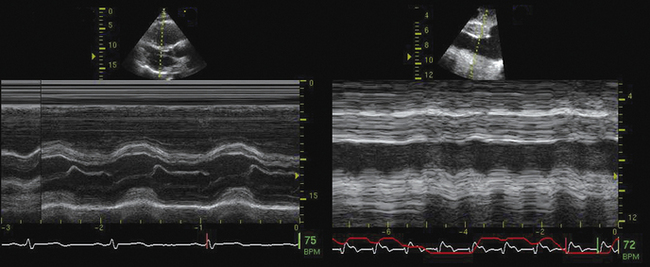
 Obtain the complete TR profile by appropriate means, and measure in the center of the parabola. The single most common problem with TR spectral recording is not having enough signal to establish the true peak velocity. If the complete profile does not appear to be present, the cursor should be placed off to the side of the profile so that the reviewer is not swayed by the position of the cursor placed by the person recording the study.
Obtain the complete TR profile by appropriate means, and measure in the center of the parabola. The single most common problem with TR spectral recording is not having enough signal to establish the true peak velocity. If the complete profile does not appear to be present, the cursor should be placed off to the side of the profile so that the reviewer is not swayed by the position of the cursor placed by the person recording the study.
 Spectral profiles should be two-thirds the height of the display, and wide enough so that there are two or three per display.
Spectral profiles should be two-thirds the height of the display, and wide enough so that there are two or three per display.
 Use zoom views liberally to identify the valve lesion responsible for TR.
Use zoom views liberally to identify the valve lesion responsible for TR.
 Proximal isovelocity surface area (PISA) techniques are acceptable for severity assessment, but offer no more than does hepatic venous flow, and therefore are not required.
Proximal isovelocity surface area (PISA) techniques are acceptable for severity assessment, but offer no more than does hepatic venous flow, and therefore are not required.
Reporting Issues
 Describe the suspected cause of the TR (i.e., leaflet, annular or RV disease).
Describe the suspected cause of the TR (i.e., leaflet, annular or RV disease).
 Describe the severity of the TR.
Describe the severity of the TR.
 Describe the RV function and geometry.
Describe the RV function and geometry.
 Note that the right ventricular systolic pressure (RVSP) varies by 25% throughout a given day.
Note that the right ventricular systolic pressure (RVSP) varies by 25% throughout a given day.
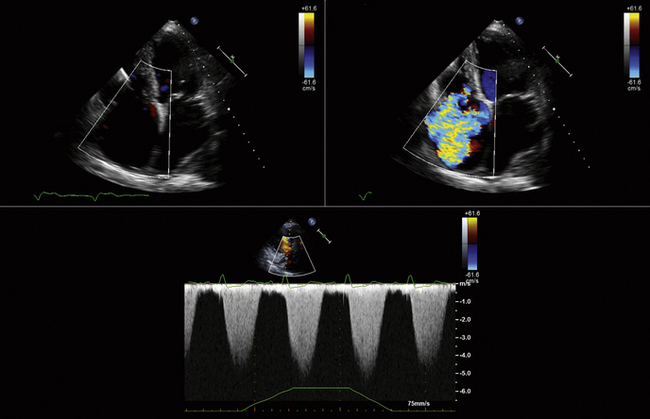
 Ensure that the true peak of the TR jet is used—attempt to avoid under-calling the severity of the RVSP.
Ensure that the true peak of the TR jet is used—attempt to avoid under-calling the severity of the RVSP.
 Avoid use of the term “trivial” for TR, as it is normal if the valve is structurally normal.
Avoid use of the term “trivial” for TR, as it is normal if the valve is structurally normal.
 RVSP only equates with pulmonary artery (PA) systolic pressure when pulmonic stenosis is absent; therefore, Doppler exclusion of pulmonary stenosis (PS) is essential.
RVSP only equates with pulmonary artery (PA) systolic pressure when pulmonic stenosis is absent; therefore, Doppler exclusion of pulmonary stenosis (PS) is essential.
For any given size of tricuspid valve ERO, there is less regurgitant flow than with MR, as the usual RV–RA gradients are less than the usual left ventricular (LV)–left atrial (LA) gradients. Absence of hepatic venous flow reversal is associated with tricuspid valve EROs (<40 mm2) and therefore, in the final analysis, tricuspid valve–ERO generally adds little to hepatic flow profiling.1
Causes of Tricuspid Regurgitation
 “Functional” (i.e., intact leaflet/chordal/papillary components)
“Functional” (i.e., intact leaflet/chordal/papillary components)
 Myxomatous tricuspid valve disease/tricuspid valve prolapse
Myxomatous tricuspid valve disease/tricuspid valve prolapse
 RV papillary muscle rupture: post-infarction, post-trauma, post-biopsy, post–lead extraction
RV papillary muscle rupture: post-infarction, post-trauma, post-biopsy, post–lead extraction
Ebstein’s Anomaly
 Apical displacement of the septal and or posterior leaflets
Apical displacement of the septal and or posterior leaflets
 “Atrialization” of the right ventricle
“Atrialization” of the right ventricle
 “Tethering” of the anterior leaflet
“Tethering” of the anterior leaflet
 Smaller functional right ventricle
Smaller functional right ventricle
 The amount of TR is usually worst at birth as the PVR is highest
The amount of TR is usually worst at birth as the PVR is highest
Estimation of Right Ventricular Systolic Pressure
Potential problems in estimating the RVSP include the following:
 No TR from which to determine RV–RA gradient
No TR from which to determine RV–RA gradient
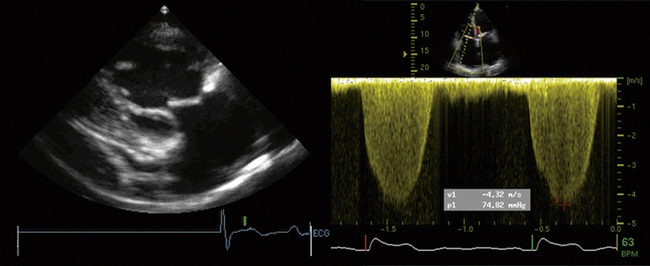
 Insufficient TR from which to determine maximum RV–RA gradient
Insufficient TR from which to determine maximum RV–RA gradient
 Inability to record the full TR profile due to inadequate signal
Inability to record the full TR profile due to inadequate signal
The correlation of RV:RA gradient is excellent (r = 0.95; SEE = 7 mm Hg)2 (r = 0.96; SEE = 7 mm Hg),3 but the correlation of jugular venous pressure estimate to catheter RAP is less good (r = 0.80; SEE = 2.3 mm Hg). Clearly, clinical estimate of jugular venous pressure overestimates lower RAPs (<8 cm) and underestimates higher RAPs—sometimes by 40% when the true RAP is 20 mm Hg.
More patients with an elevated RVSP have analyzable TR spectral profiles than do patients (half) with normal RVSP.3 However, an important minority subset of patients with severely elevated RVSP (approximately 20–25% of cases of primary pulmonary hypertension) may not have associated TR to yield an analyzable (complete) TR spectral profile. Overall, the correlation of echocardiographic RVSP to catheter RVSP is quite good (r = 0.93; SEE = 8 mm), but remains influenced by the vagaries of estimating jugular venous pressure and RAP.2
Indications for the management and intervention in tricuspid regurgitation are listed in Boxes 7-1 and 7-2.
Tricuspid Stenosis
Scanning Issues
Required parameters to obtain from scanning include the following:
Tricuspid Atresia
Concerns
 By definition, TS is present when there is a mean gradient of ≥5 mm Hg. The difference between normal tricuspid valve “gradient” by the modified equation (= 4 × V2, = 4 × 0.72 = 2 mm Hg), where V is peak diastolic velocity across the tricuspid valve, and what constitutes significant TS (≥5 mm Hg) is a small difference.
By definition, TS is present when there is a mean gradient of ≥5 mm Hg. The difference between normal tricuspid valve “gradient” by the modified equation (= 4 × V2, = 4 × 0.72 = 2 mm Hg), where V is peak diastolic velocity across the tricuspid valve, and what constitutes significant TS (≥5 mm Hg) is a small difference.
 Neither the modified Bernouilli relation nor the PHT relation is as accurate for the evaluation of most cases of TS as they are for most cases of MS.
Neither the modified Bernouilli relation nor the PHT relation is as accurate for the evaluation of most cases of TS as they are for most cases of MS.
 The 220/PHT has not been validated for the tricuspid valve, and is essentially “borrowed” from the validation of MS with areas of 1.0 to 1.5 cm2.
The 220/PHT has not been validated for the tricuspid valve, and is essentially “borrowed” from the validation of MS with areas of 1.0 to 1.5 cm2.
 It is proposed by some that 190/PHT be used for the assessment of TS.
It is proposed by some that 190/PHT be used for the assessment of TS.
 In TS, the RAP will be very elevated, confounding estimation of RVSP determination using usual estimated RAP.
In TS, the RAP will be very elevated, confounding estimation of RVSP determination using usual estimated RAP.
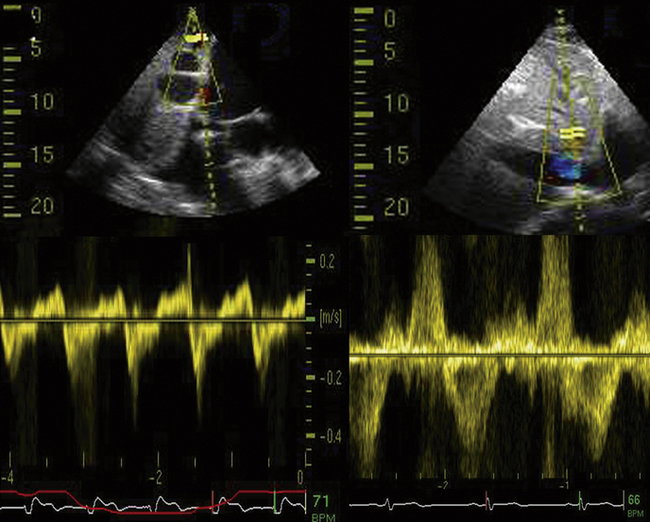
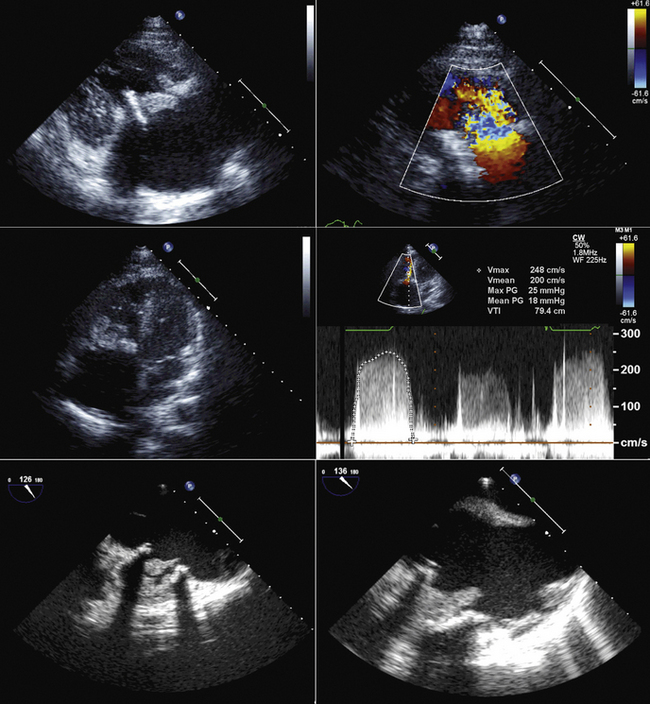
Pulmonic Stenosis
The valvular diameter dimension is used to identify the optimal balloon size for dilation.
Indications for the evaluation of pulmonary stenosis are given in Box 7-3 and and indications for balloon valvulopathy are given in Box 7-4.
Summary
 TS requires fusion of at least two commissures.
TS requires fusion of at least two commissures.
 The 5-mm Hg gradient of significant TS is a problem for the modified Bernouilli equation.
The 5-mm Hg gradient of significant TS is a problem for the modified Bernouilli equation.
 Tricuspid insufficiency is readily detected by echocardiography, and its cause is usually apparent.
Tricuspid insufficiency is readily detected by echocardiography, and its cause is usually apparent.
 Alternate imaging modalities generally add little for the assessment of the tricuspid valve.
Alternate imaging modalities generally add little for the assessment of the tricuspid valve.
 Conversely, cardiac magnetic resonance offers a robust means, and the only accurately quantitative means, to calculate pulmonic insufficiency volume, regurgitant fraction, right ventricular volume, and ejection fraction. Cardiac magnetic resonance also can more accurately depict the anatomy of the pulmonary subvalvar and supravalvar segments.
Conversely, cardiac magnetic resonance offers a robust means, and the only accurately quantitative means, to calculate pulmonic insufficiency volume, regurgitant fraction, right ventricular volume, and ejection fraction. Cardiac magnetic resonance also can more accurately depict the anatomy of the pulmonary subvalvar and supravalvar segments.
BOX 7-1 Management of Tricuspid Regurgitation: ACC/AHA 2006 Recommendations
Class III
 Tricuspid valve replacement or annuloplasty is not indicated in asymptomatic patients with TR whose pulmonary artery systolic pressure is <60 mm Hg in the presence of a normal mitral valve. (Level of evidence: C)
Tricuspid valve replacement or annuloplasty is not indicated in asymptomatic patients with TR whose pulmonary artery systolic pressure is <60 mm Hg in the presence of a normal mitral valve. (Level of evidence: C)
 Tricuspid valve replacement or annuloplasty is not indicated in patients with mild primary TR. (Level of evidence: C)
Tricuspid valve replacement or annuloplasty is not indicated in patients with mild primary TR. (Level of evidence: C)
From ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 2006;48(3):e1–e148.
BOX 7-2 Indications for Intervention in Tricuspid Regurgitation: ACC/AHA 2006 Recommendations
Class I
1. Surgery for severe tricuspid regurgitation (TR) is recommended for adolescent and young adult patients with deteriorating exercise capacity (New York Heart Association [NYHA] functional class III or IV). (Level of evidence: C)
2. Surgery for severe TR is recommended for adolescent and young adult patients with progressive cyanosis and arterial saturation less than 80% at rest or with exercise. (Level of evidence: C)
3. Interventional catheterization closure of the atrial communication is recommended for the adolescent or young adult with TR who is hypoxemic at rest and with exercise intolerance due to increasing hypoxemia with exercise, when the tricuspid valve appears difficult to repair surgically. (Level of evidence: C)
Class IIa
1. Surgery for severe TR is reasonable in adolescent and young adult patients with NYHA functional class II symptoms if the valve appears to be repairable. (Level of evidence: C)
2. Surgery for severe TR is reasonable in adolescent and young adult patients with atrial fibrillation. (Level of evidence: C)
Class IIb
1. Surgery for severe TR may be considered in asymptomatic adolescent and young adult patients with increasing heart size and a cardiothoracic ratio of more than 65%. (Level of evidence: C)
2. Surgery for severe TR may be considered in asymptomatic adolescent and young adult patients with stable heart size and an arterial saturation of less than 85%, when the tricuspid valve appears repairable. (Level of evidence: C)
3. In adolescent and young adult patients with TR who are mildly cyanotic at rest but who become very hypoxemic with exercise, closure of the atrial communication by interventional catheterization may be considered when the valve does not appear amenable to repair. (Level of evidence: C)
4. If surgery for Ebstein’s anomaly is planned in adolescent and young adult patients (tricuspid valve repair or replacement), a preoperative electrophysiologic study may be considered to identify accessory pathways. If present, these may be considered for mapping and ablation either preoperatively or at the time of surgery. (Level of evidence: C)
From ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 2006;48(3):e1–e148.
BOX 7-3 Evaluation of Pulmonic Stenosis in Adolescents and Young Adults: ACC/AHA 2006 Recommendations
Class I
1. An ECG is recommended for the initial evaluation of pulmonic stenosis in adolescent and young adult patients, and serially every 5–10 years for follow-up examinations. (Level of evidence: C)
2. Transthoracic Doppler echocardiography is recommended for the initial evaluation of pulmonic stenosis in adolescent and young adult patients, and serially every 5–10 years for follow-up examinations. (Level of evidence: C)
3. Cardiac catheterization is recommended in the adolescent or young adult with pulmonic stenosis for evaluation of the valvular gradient if the Doppler peak jet velocity is >3 m/sec (estimated peak gradient >36 mm Hg), and balloon dilation can be performed if indicated. (Level of evidence: C)
From ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 2006;48(3):e1–e148.
BOX 7-4 Balloon Valvotomy in Pulmonic Stenosis: ACC/AHA 2006 Recommendations
Class I
1. Balloon valvotomy is recommended in adolescent and young adult patients with pulmonic stenosis who have exertional dyspnea, angina, syncope, or presyncope and an RV–to–pulmonary artery peak-to-peak gradient >30 mm Hg at catheterization. (Level of evidence: C)
2. Balloon valvotomy is recommended in asymptomatic adolescent and young adult patients with pulmonic stenosis and RV–to–pulmonary artery peak-to-peak gradient >40 mm Hg at catheterization. (Level of evidence: C)
From ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 2006;48(3):e1–e148.
Transthoracic Echocardiography
ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography5
Native Valvular Regurgitation or Stenosis with TTE
 Routine surveillance of trace valvular regurgitationAppropriateness criteria: I; median score: 1
Routine surveillance of trace valvular regurgitationAppropriateness criteria: I; median score: 1
 Routine surveillance (<3 yr) of mild valvular regurgitation or stenosis without a change in clinical status or cardiac examinationAppropriateness criteria: I; median score: 2
Routine surveillance (<3 yr) of mild valvular regurgitation or stenosis without a change in clinical status or cardiac examinationAppropriateness criteria: I; median score: 2
 Routine surveillance (≥3 yr) of mild valvular regurgitation or stenosis without a change in clinical status or cardiac examinationAppropriateness criteria: U; median score: 4
Routine surveillance (≥3 yr) of mild valvular regurgitation or stenosis without a change in clinical status or cardiac examinationAppropriateness criteria: U; median score: 4
 Routine surveillance (<1 yr) of moderate or severe valvular regurgitation or stenosis without a change in clinical status or cardiac examinationAppropriateness criteria: U; median score: 6
Routine surveillance (<1 yr) of moderate or severe valvular regurgitation or stenosis without a change in clinical status or cardiac examinationAppropriateness criteria: U; median score: 6
 Routine surveillance (≥1 yr) of moderate or severe valvular regurgitation or stenosis without change in clinical status or cardiac examinationAppropriateness criteria: A; median score: 8
Routine surveillance (≥1 yr) of moderate or severe valvular regurgitation or stenosis without change in clinical status or cardiac examinationAppropriateness criteria: A; median score: 8
Transesophageal Echocardiography
Nuclear
ACCF/ASNC/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging7
Evaluation of LV Function
 Assessment of LV function with radionuclide angiography (ERNA or FP RNA)
Assessment of LV function with radionuclide angiography (ERNA or FP RNA)
In absence of recent reliable diagnostic information regarding ventricular function obtained with another imaging modality
Appropriateness criteria: A, appropriate; I, inappropriate; U, uncertain.
LV, left ventricular; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
TABLE 7-1 Utility of Different Imaging Modalities and Cardiac Catheterization in the Assessment of Tricuspid Valve Disease
| MODALITY | PROS | CONS/CAVEATS |
|---|---|---|
| Transthoracic Echocardiography |
CMR is the best test to follow right ventricular volumes and systolic function, and tricuspid valve regurgitant volumes and fraction. SSFP sequences will determine the total RV stroke volume, velocity-encoded phase contrast sequences will determine the net forward stroke volume; the difference is the TR volume.
CMR, cardiac magnetic resonance; NA, not applicable; RVEF, right ventricular ejection fraction; SSFP, steady-state free precession; TEE, transesophageal echocardiography; TR, tricuspid regurgitation; TS, tricuspid stenosis; TTE, transthoracic echocardiography.
TABLE 7-2 Utility of Different Imaging Modalities and Cardiac Catheterization in the Assessment of Pulmonic Valve Disease
| MODALITY | PROS | CONS/CAVEATS |
|---|---|---|
| Transthoracic Echocardiography | ||
| Transesophageal Echocardiography | ||
| Cardiac CT | ||
| Cardiac MRI | ||
| LGE sequences: NA | ||
| Nuclear | NA | |
| Chest Radiography | NA | |
| Cardiac Catheterization | NA |
CMR, cardiac magnetic resonance; ECG, electrocardiographic; LGE, late gadolinium enhancement; NA, not applicable; PI, pulmonary insufficiency; PS, pulmonary stenosis; RV, right ventricular; RVEF, right ventricular ejection fraction; RVOT, right ventricular outflow tract; SSFP, steady-state free precession; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography; VEPC, velocity-encoded phase contrast.
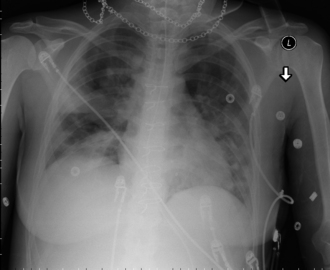
Figure 7-11 Same patient as in Figure 7-10. The sternotomy wires are obvious, and the bioprosthesis stent wires can be seen. There is extensive patchy consolidation due to septic embolization of tricuspid valve vegetations into the lungs.
1. Tribouilloy C.M., Enriquez-Sarano M., Capps M.A., et al. Contrasting effect of similar effective regurgitant orifice area in mitral and tricuspid regurgitation: a quantitative Doppler echocardiographic study. J Am Soc Echocardiogr. 2002;15(9):958-965.
2. Yock P.G., Popp R.L. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984;70(4):657-662.
3. Currie P.J., Seward J.B., Chan K.L., et al. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985;6(4):750-756.
4. Bonow R.O., Carabello B.A., Chatterjee K., et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 2006;48(3):e1-e148.
5. Douglas P.S., Garcia M.J., Haines D.E., et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography. J Am Coll Cardiol. 2011;57(9):1126-1166.
6. Taylor A.J., Cerqueira M., Hodgson J.M., et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. J Am Coll Cardiol. 2010;56(22):1864-1894.
7. Hendel R.C., Berman D.S., Di Carli M.F., et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging. J Am Coll Cardiol. 2009;53(23):2201-2229.
8. Nishimura R.A., Carabello B.A., Faxon D.P., et al. ACC/AHA 2008 guideline update on valvular heart disease: focused update on infective endocarditis. J Am Coll Cardiol. 2008;52(8):676-685.