CHAPTER 22 Triangular Fibrocartilage Débridement and Arthroscopically Assisted Ulnar Shortening
ANATOMY
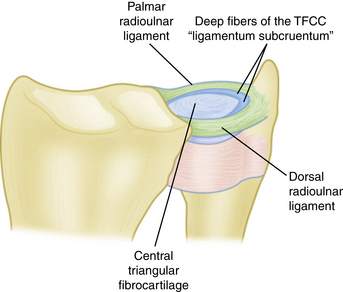
The triangular fibrocartilage is the primary stabilizer of the distal radioulnar joint. It attaches radially on the distal lip of the sigmoid notch. Ulnarly, the triangular fibrocartilage inserts at the base of the ulnar styloid by means of a continuation of the dorsal and palmar radioulnar ligaments and the fibers of the ligamentum subcruentum (Fig. 22-1).1,2
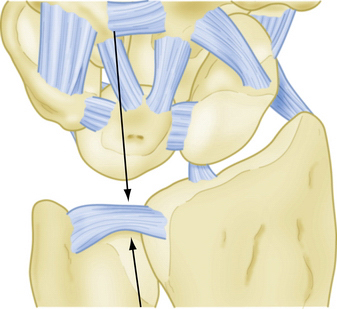
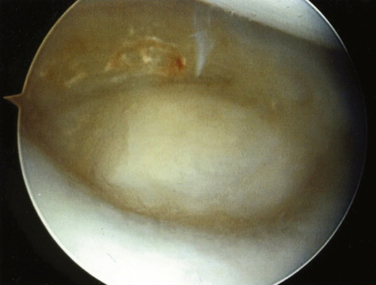
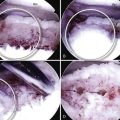
A patient with an ulnar abutment syndrome typically presents with a central tear of the TFCC. Chondromalacia can be seen at the ulnar aspect of the lunate and the distal radial surface of the ulnar head. Ulnocarpal synovitis is usually present (Fig. 22-2).
PATIENT EVALUATION
History
Tears of the triangular fibrocartilage are typically the result of a fall on the outstretched upper extremity. The ulna is driven distally and compresses the TFCC between itself and the lunate, producing a central or radial tear of the articular disk. This same mechanism can result in lunatotriquetral tears and peripheral TFCC tears, neither of which is discussed further here.
An ulnar abutment syndrome can develop as a result of settling of a distal radial fracture fragment. The radial collapse leads to a relative lengthening of the ulna. Palmer and colleagues2 demonstrated an increase in the ulnocarpal load with increasing ulnar variance.
Physical Examination
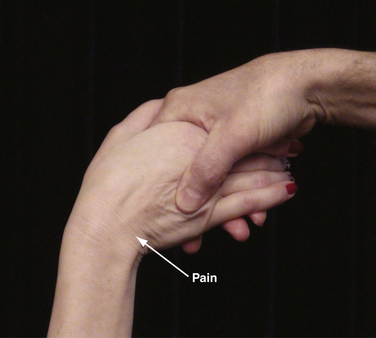
The ulnocarpal compression test (Fig. 22-3) is particularly helpful in assessing the patient with a suspected ulnar abutment syndrome. In this test, the patient sits in front of the examiner with the wrist in supination. The wrist is simultaneously ulnarly deviated and axially loaded while the forearm is supinated and pronated. The patient with an ulnar abutment syndrome experiences pain at the ulnocarpal joint, with or without popping and grinding, during this maneuver.
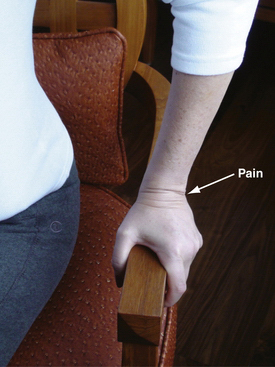
A variation of the ulnocarpal compression test is the Lester press test (Fig. 22-4).3 In this test, the patient sits in a chair with sturdy arms and lifts himself or herself off the chair seat. Pain at the ulnocarpal joint is considered pathognomonic for a TFCC tear.
Diagnostic Imaging
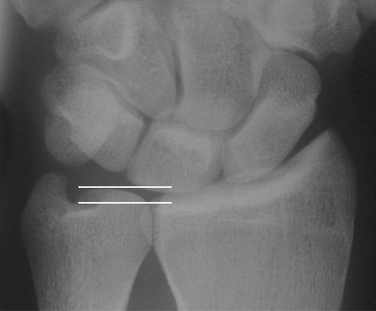
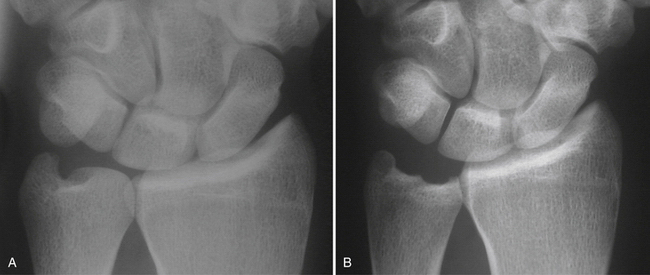
The radiographic evaluation of a patient with an ulnar abutment should include a standard wrist series and a Palmer 90 × 90 view (Fig. 22-5). The Palmer 90 × 90 view places the forearm in neutral rotation while the elbow is flexed to 90 degrees and the shoulder is abducted to 90 degrees.4 The ulnar variance is calculated from this view. An ulnar abutment can be suspected in a patient with an ulnar-zero or ulnar-minus variance. The ulnar aspect of the lunate should be carefully examined for subchondral cysts.
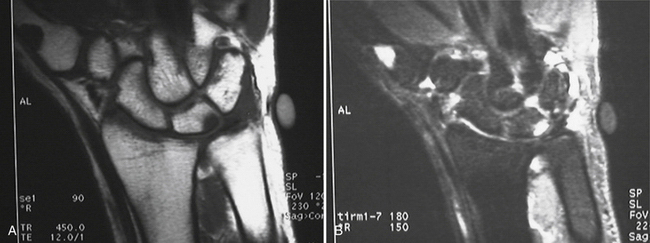
Magnetic resonance imaging (MRI) should be considered when evaluating the patient for ulnar abutment. MRI demonstrates increased signal in the lunate on T2 images (Fig. 22-6), corresponding to a cyst or intraosseous edema. The triangular fibrocartilage can also be evaluated on the MRI images. Whether a magnetic resonance (MR) arthrogram is needed is a function of the MR resolution. The accuracy of lower-resolution MR is increased with the addition of an intra-articular gadolinium injection.
TREATMENT
Preoperative Planning
Preoperative evaluation should include radiographs of the wrist, comprising a wrist series and a 90 × 90 view, as described by Andrew Palmer.2 An MRI study, with or without an arthrogram, can also be helpful.
Arthroscopic Technique
Triangular Fibrocartilage Complex Débridement: Mechanical
The dorsal aspect of the TFCC tear usually can be débrided through the 3-4 and 4-5 portals. Occasionally, the instruments need to be passed through the 6-U portal while the arthroscope is placed in the 3-4 portal. Injury to the dorsal sensory branch of the ulnar nerve is avoided when using the 6-U portal with a longitudinal portal incision and blunt dissection to reach the ulnocarpal joint capsule.
The end point of TFCC débridement is reached when the ulnar head is visible through the TFCC and a stable TFCC perimeter is created (Fig. 22-7). Typically, a central defect measuring at least 1 cm in diameter is created.
Arthroscopic Ulnar Shortening Technique
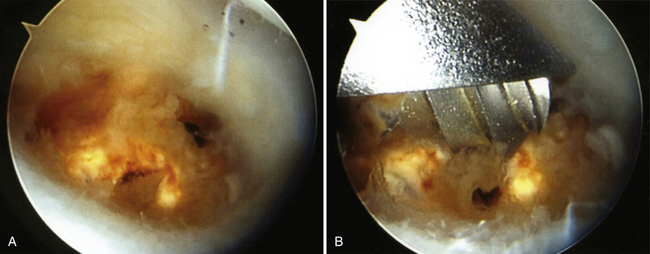
Arthroscopic ulnar shortening is accomplished by placing the arthroscope in the 3-4 portal and introducing the instruments through the 4-5 portal. Occasionally, the 6-U portal can be used, as can the distal radioulnar joint portal. Although the holmium:yttrium-aluminum-garnet (Ho:YAG) laser is very useful for ulnar shortening, the barrel abrader can be used alone or in combination with the laser. If the Ho:YAG laser is used, it is introduced through the 4-5 portal, and the cartilage and subchondral bone of the ulnar seat of the distal ulna are rapidly vaporized (Fig. 22-8A). The laser becomes less efficient after the trabeculae of the distal ulna are visible. At that point, the 2.9-mm barrel abrader is brought in to finish the shortening (Fig. 22-8B). It is important to avoid injury to the sigmoid notch, and frequent fluoroscopic monitoring of the amount of bone resected is mandatory. Care must be taken to fully supinate and pronate the wrist to adequately débride the ulnar head. All instruments are removed at the end of the procedure, and the wrist is ulnarly deviated, axially loaded, supinated, and pronated to be sure no clicking or popping can be heard. If any clicking or popping emanates from the area of the surgery, further ulnar resection may be required. The goal of the surgery is to create an ulnar-minus variance of 2 mm (Fig. 22-9). Any irregularities of the remaining distal ulna should be minimized. Small irregularities, however, have a tendency to flatten out with the passage of time.
PEARLS& PITFALLS
Postoperative Management
Wounds are closed using subcuticular sutures of 4-0 Prolene; the sutures are removed after 2 weeks. Strengthening exercises can be started at 6 weeks if needed. Premature resumption of heavy lifting or repetitive activities will lead to ulnocarpal synovitis. The patient is instructed to avoid heavy lifting for 3 months.
CONCLUSIONS
The results of arthroscopic débridement of traumatic triangular fibrocartilage tears have been very good.5,6 However, Minami and colleagues7 found that degenerative tears (Palmer type 2) have a less favorable prognosis because of their associated ulnar wrist pathology. Our results8 and those reported by Osterman9 and Palmer10 suggest that arthroscopically assisted ulnar shortening in properly selected patients provides excellent or good results in more than 80% of cases.
1. Kleinman WB. Stability of the distal radioulnar joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function. What we have learned in 25 years. J Hand Surg Am. 2007;32:1086-1106.
2. Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg Am. 1984;9:681-682.
3. Lester B, Halbrecht J, Levy IM, Gaudinez R. “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995;35:41-45.
4. Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg Am. 1982;7:376-379.
5. Husby T, Haugstvedt JR. Long-term results after arthroscopic resection of lesions of the triangular fibrocartilage complex. Scand J Plast Reconstr Surg Hand Surg. 2001;35:79-83.
6. Infanger M, Grimm D. Meniscus and discus lesions of triangular fibrocartilage complex (TFCC): treatment by laser-assisted wrist arthroscopy. J Plast Reconstr Aesthet Surg. 2009;62:466-471.
7. Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg Am. 1996;21:406-411.
8. Nagle DJ, Bernstein MA. Laser-assisted arthroscopic ulnar shortening. Arthroscopy. 2002;18:1046-1051.
9. Osterman AL. Arthroscopic debridement of triangular fibrocartilage complex tears. Arthroscopy. 1990;6:120-124.
10. Wnorowski DC, Palmer AK, Werner FW, Fortino MD. Anatomic and biomechanical analysis of the arthroscopic wafer procedure. Arthroscopy. 1992;8:204-212.