Treatment Paradigms for the Management of Severe Ocular Surface Disease
Introduction
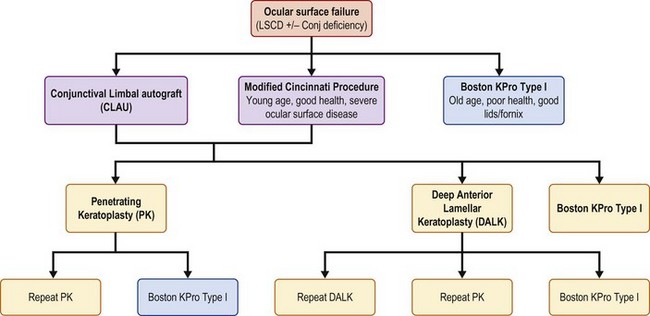
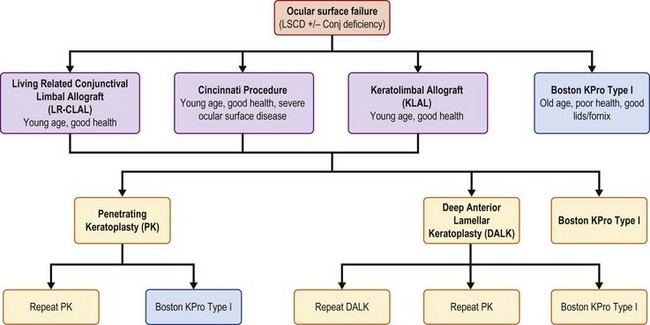
The options for ocular surface stabilization using medical treatment are outlined in Box 54.1. While medical therapy can be both helpful and often necessary for restoration of the integrity of the ocular surface, it may not be suitable as a long-term treatment option, especially if there is severe stem cell damage. In conditions resulting from severe stem cell deficiency, management options shift to surgical alternatives. The flow diagrams outline our approach to decision-making in the surgical treatment of ocular surface disease based on whether the pathology is unilateral (Fig. 54.1) or bilateral (Fig. 54.2).
Surgical Treatment Options
The primary considerations for decision-making in the surgical management of ocular surface disease from stem cell deficiency include: (1) the laterality of disease, (2) the degree of stem cell involvement, (3) the level of tear production/baseline tear status, and (4) whether or not there is conjunctival inflammation. The presence of conjunctival inflammation is a particularly important finding and may have significant bearing on the surgical planning for repair of the damaged ocular surface. Treatment strategies are outlined in the flowcharts for unilateral disease (Fig. 54.1).
Unilateral Disease
Unilateral Conjunctival Disease
In a patient with unilateral ocular surface disease, preoperative planning should include careful evaluation of the status of the conjunctiva in both eyes. A patient with unilateral disease limited to the conjunctiva does not require limbal stem cell transplantation. Conditions in this category would include primary and recurrent pterygium and unilateral focal conjunctival tumors, such as squamous cell carcinoma or conjunctival intraepithelial neoplasia (CIN). These conditions may benefit from a conjunctival autograft from the same eye or from the contralateral eye. The autograft can be harvested from the superior or inferior bulbar conjunctiva, taking into consideration that symblepharon formation remains a slightly higher risk for inferior conjunctival grafts. Limbal tissue is not needed when harvesting an autologous conjunctival graft. Figure 54.1 provides a flow diagram for surgical treatment options.
If conjunctiva cannot be harvested from the same or contralateral eye, amniotic membrane can serve as an adjunct to close the conjunctival defect. Amniotic membrane by itself carries slightly higher risk for recurrence, compared to conjunctival grafts, but can be used when viable conjunctiva is not available.1,2 Conjunctival autograft or amniotic membrane fixation is performed with either suture or fibrin glue and requires local immunosuppression with corticosteroids. Systemic immunosuppression is not required with these techniques.
Bilateral Disease
Bilateral ocular surface disease has a more guarded prognosis and the surgical options are more limited. Both the extent of disease and the presence of conjunctival inflammation are important considerations in the preoperative evaluation. In bilateral disease, use of tissue from the contralateral eye is not feasible. Figure 54.1 provides a flow diagram for surgical treatment options.
Bilateral Limbal Disease with Normal Conjunctiva
Many of the ocular surface disease states are complicated by corneal scarring and opacification and will ultimately require subsequent keratoplasty. In such situations, deep anterior lamellar keratoplasty (DALK) may be advantageous over penetrating keratoplasty (PK) with elimination of potential endothelial rejection and improved tectonic wound stability.3 Keratoprosthesis surgery may also be useful after failed keratoplasty in lieu of DALK or PK in conditions where repeat cadaveric tissue transplantation has little to no chance of survival. Patients with bilateral limbal disease should not undergo DALK or PK prior to an ocular surface transplantation procedure, because the graft will not survive functionally if a significant amount of the limbal stem cells have been damaged.
Bilateral Limbal Disease with Prior Conjunctival Disease
This category of ocular surface disease involves conditions which cause bilateral limbal disease with previous but now subsided or controlled conjunctival inflammation. Box 54.1 lists the treatments that might be used to treat such inflammation. This category includes eyes with past injuries to the conjunctiva or previous episodes of inflammation from conjunctival inflammatory conditions. In these patients, KLAL or lr-CLAL, or a combination of the two (Cincinnati Procedure) are potential options for surgical treatment. Keratoprosthesis surgery is an additional option. If minimal conjunctival damage is present and/or no living-related donors are present, KLAL is the best option unless the patient is elderly or has systemic disease that would contraindicate the systemic immunosuppression needed with KLAL. If conjunctival damage is significant and a living-related donor is available, lr-CLAL remains the best options in a young and otherwise healthy patient as conjunctiva and limbal cells are provided to the ocular surface and a tissue match may be possible. In severe cases with large amounts of symblepharon and ocular surface failure, the preferred treatment option would be the Cincinnati procedure. This procedure combines lr-CLAL segments to the superior and inferior limbus in combination with cadaveric KLAL along the nasal and temporal limbus. Keratoprosthesis surgery may be the best option if systemic immunosuppression is contraindicated.
Bilateral Limbal Disease with Active Conjunctival Inflammation
Bilateral limbal disease with concurrent active conjunctival inflammation represents the most challenging situation for surgery of the ocular surface. This category of diseases includes conditions such as Stevens–Johnson syndrome, ocular cicatricial pemphigoid, and autoimmune inflammatory conditions. These disease states carry the poorest prognosis of diseases of the ocular surface. Prior to any surgical intervention, every effort must be made to mitigate conjunctival inflammation. The authors typically utilize topical, as well as systemic immunosuppressive therapy, including a number of additional adjunct medical treatments listed in Box 54.1. Autologous serum drops can be a particularly useful adjunct to topical and systemic immunosuppression, due to its constituents of vitamins, anti-inflammatory factors and growth factors that promote stabilization of the ocular surface.4 Any surgery should be delayed if possible until there is either resolution or significant improvement in conjunctival inflammation.
References
1. Luanratanakorn, P, Ratanapakorn, T, Suwan-Apichon, O, et al. Randomised controlled study of conjunctival autograft versus amniotic membrane graft in pterygium excision. Br J Ophthalmol. 2006;90:1476–1480.
2. Kaufman, SC, Lee, WB, Jacobs, DS, et al. Options and adjuvants in surgery for pterygium: A Report by the American Academy of Ophthalmology. Ophthalmology. 2013;120:201–208.
3. Reinhart, WJ, Musch, DC, Jacobs, DS, et al. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty. Ophthalmology. 2011;118:209–218.
4. Quinto, GG, Campos, M, Behrens, A. Autologous serum for ocular surface diseases. Arq Bras Oftalmol. 2008;71:47–54.