CHAPTER 13 Treatment of Upper Eyelid Retraction: Internal Approach
For more than 30 years, I have preferred treating upper eyelid retraction secondary to thyroid ophthalmopathy with an internal rather than external approach. Excellent results, high patient satisfaction, and minimal need for secondary surgery lead to my bias toward this approach.
Upper eyelid retraction surgery occasionally is combined with retraction surgery of the lower eyelid, with or without lateral tarsorrhaphies (see Chapter 18). If there is minimal upper eyelid retraction, the surgery can be combined with an upper eyelid skin muscle-fat excision without eyelid reconstruction; if the retraction is moderate or severe, the external tissue excision is deferred to a second sitting since I am concerned that tightening of the skin might interfere with the results of the upper eyelid retraction surgery.
In this chapter, I describe a technique that Urist and I reported on in 1972, in which Müller’s muscle is excised and the levator aponeurosis is recessed from an internal approach.1 The procedure is performed with sensory but not motor anesthesia. The eyelid level is controlled intraoperatively while the patient is seated up on the operating table.
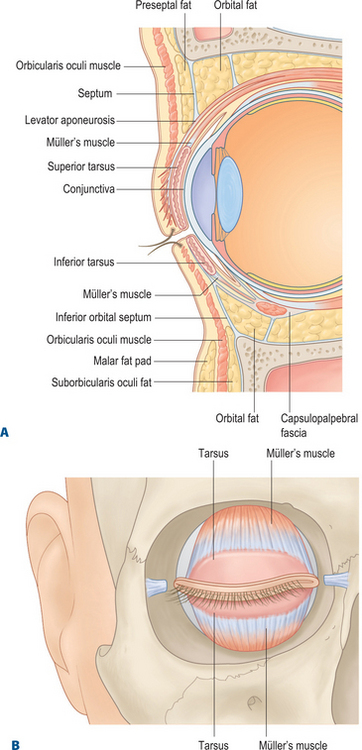
Anatomy
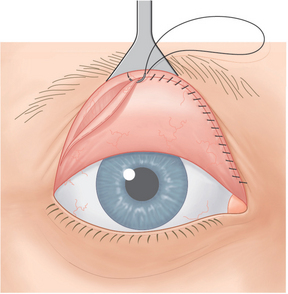
Müller’s muscle in the upper eyelid originates from the levator aponeurosis approximately 15 mm above the superior tarsal border and inserts onto the superior tarsal border (Fig. 13-1). This muscle spans the horizontal dimension of the eyelid, is firmly attached to conjunctiva on its posterior surface, and is loosely attached to the levator aponeurosis on its anterior surface. Müller’s muscle resembles other smooth muscle tissue and is approximately 1 mm thick.
Margin reflex distance-1
It is important to assess the upper eyelid levels with the margin reflex distance-1 (MRD1) measurement (see Chapter 3, Fig. 3-8).
Surgical technique
Anesthesia
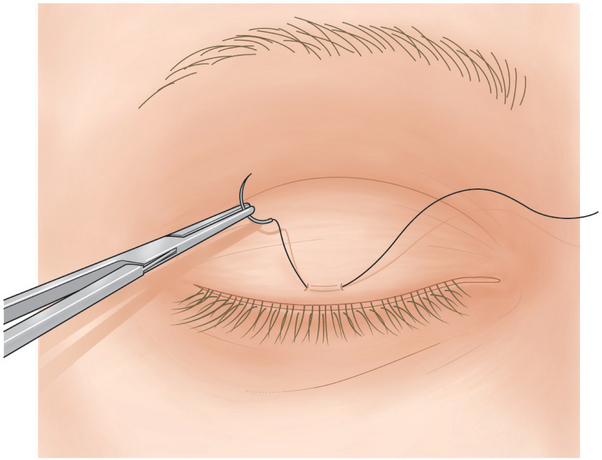
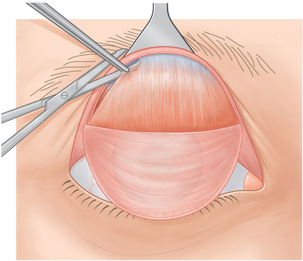
A 4-0 silk suture is placed in the center of the upper eyelid 2 mm above the eyelash line, through the skin, orbicularis muscle, and anterior tarsus (Fig. 13-2). Topical 0.5 percent tetracaine drops are applied to the eye, and a scleral lens is placed over the globe to protect it during surgery.
Conjunctival dissection
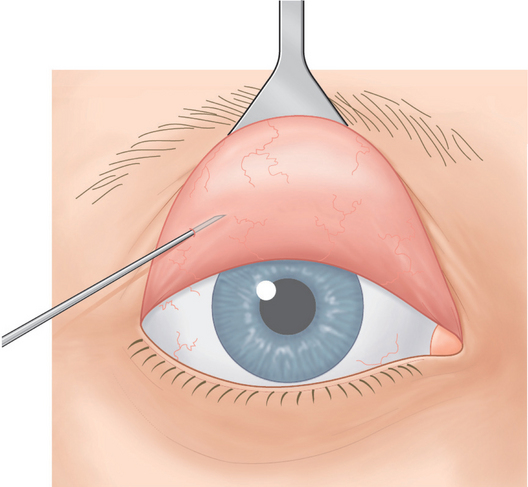
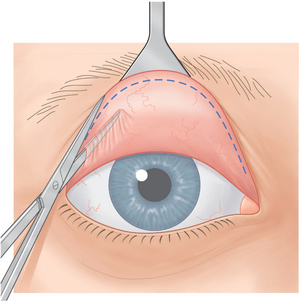
With a Desmarres retractor, the surgeon everts the upper eyelid to expose the superior palpebral conjunctiva. The upper palpebral conjunctiva is flooded with 0.5 percent tetracaine drops. Cotton-tipped applicators saturated with tetracaine also are rolled over the conjunctiva. Then, 0.25–0.5 ml of 2 percent lidocaine with epinephrine is injected subconjunctivally adjacent to the superior tarsal border over the entire width of the eyelid (Fig. 13-3).
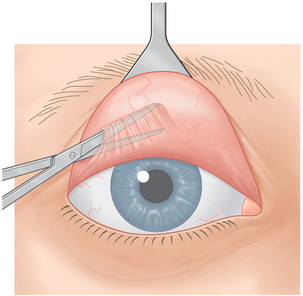
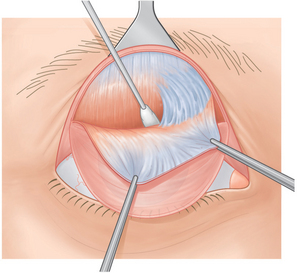
The conjunctiva is grasped just over the superior tarsal border at the temporal aspect of the eyelid and is severed with Westcott scissors. The surgeon inserts straight, sharp-pointed iris scissors between the conjunctiva and Müller’s muscle and spreads the scissors blades to separate conjunctiva from the muscle (Fig. 13-4).
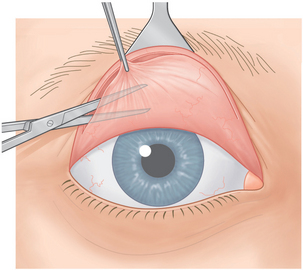
Conjunctiva is severed from the superior tarsal border (Fig. 13-5). The surgeon further dissects conjunctiva from the muscle by spreading the scissors blades between the two tissues to the superior fornix (Fig. 13-6). The surgeon can facilitate this dissection by observing the points of the blades through the translucent conjunctiva. Sharp dissection with the iris scissors releases any remaining attachments between conjunctiva and Müller’s muscle.
Müller’s muscle dissection
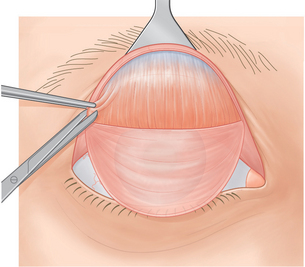
The surgeon grasps Müller’s muscle with a toothed forceps at the temporal aspect of the eyelid just above the superior tarsal border. The muscle is pulled outward, and the Desmarres retractor is pulled simultaneously in the opposite direction. Müller’s muscle is cut from the tarsus temporally (Fig. 13-7).
Müller’s muscle is then undermined from the levator aponeurosis at the level of the superior tarsal border (Fig. 13-8). Müller’s muscle, which is all the tissue attached to the top of the tarsus, is severed over the temporal two-thirds of the eyelid (Fig. 13-9).
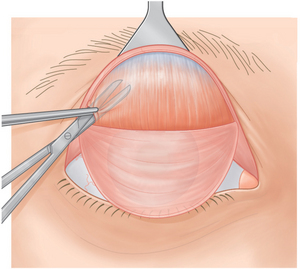
Wet cotton-tipped applicators are used to dissect Müller’s muscle bluntly from its loose attachment to the levator aponeurosis. This dissection is performed approximately 10–12 mm above the superior tarsal border over the temporal one half to two thirds of the eyelid (Fig. 13-10).
If the upper eyelid is at a satisfactory position, the head of the operating table is lowered and the patient lies down. The section of Müller’s muscle that has been detached is clamped with a straight hemostat at its base and is excised. Bleeding from the stump of Müller’s muscle is carefully controlled with a disposable cautery. If there is residual retraction, Müller’s muscle is released to 10–15 mm above the tarsus over the temporal two-thirds to three-fourths of the eyelid. It is better to be conservative in releasing Müller’s muscle nasally because a nasal ptosis can easily occur.
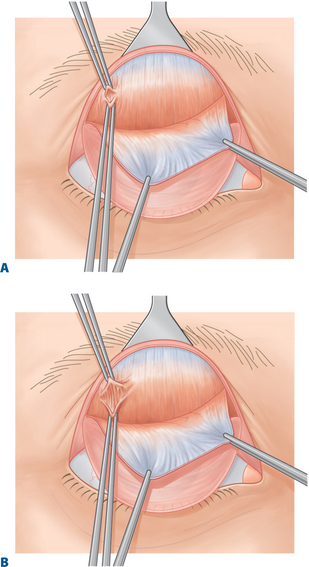
Levator stripping
Again, the patient is brought to a sitting position and the eyelid levels are evaluated. If the eyelid is still retracted, overaction of the levator muscle is implicated and this muscle must be released. The patient lies down, and the scleral lens and Desmarres retractor are reapplied. With the eyelid everted, the fibers of the levator aponeurosis that pass over the anterior surface of the tarsus are exposed. Using two toothed forceps, the surgeon grasps the superficial layers of the levator aponeurosis at the level of the superior tarsus. The levator aponeurosis layers are stripped vertically, layer by layer, along the sections of the eyelid that remain retracted (Fig. 13-11A & B).
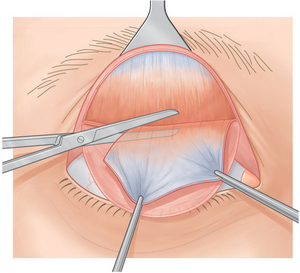
Müller’s muscle excision
The detached part of Müller’s muscle is then clamped with a straight hemostat at its base and is excised (Fig. 13-12). Pulling the conjunctival flap downward with a cotton-tipped applicator brings the stump of Müller’s muscle into view and facilitates cauterization of any bleeding areas.
Comments
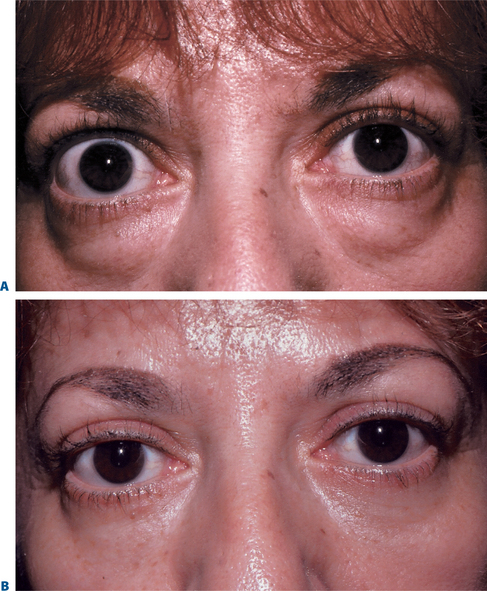
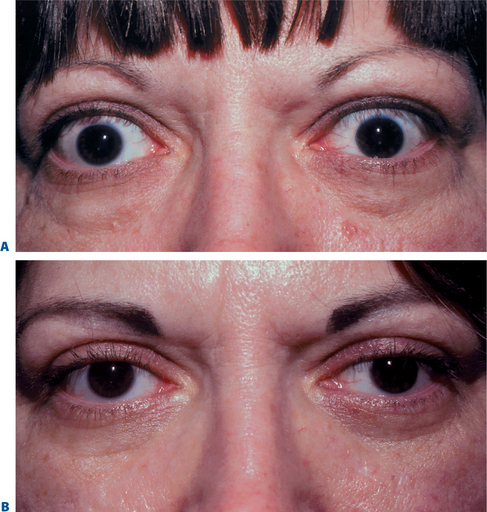
The excision of Müller’s muscle and levator aponeurosis in the manner described is a highly successful technique for treating thyroid-related retraction of the upper eyelid (Figs 13-14 and 13-15). The procedure is based on the theory of the physiologic and anatomic origin of the condition. It is a relatively simple technique that does not alter the major anatomic relationship in the eyelid by the implantation of a foreign body or by distortion of the tissues.
With the patient sitting up at various times during the procedure, the surgeon can make adjustments by progressively recessing Müller’s muscle and levator aponeurosis until the desired eyelid level and arch are achieved. Overcorrection can be recognized during the surgery and dealt with by reattaching the recessed tissues to tarsus or skin.
Results
I have performed this procedure on close to 1000 upper eyelids. The results have been studied in several previously reported publications.1–4 The success rate of bringing the upper eyelid close to a normal level is approximately 90 percent.
In approximately 10 percent of cases, the eyelid is retracted or ptotic and requires secondary surgery. If the eyelid continues to be retracted, secondary treatment with an external levator recession is recommended. If the eyelid is ptotic, I perform a full thickness resection ptosis procedure over the ptotic areas5 or I employ an external approach and perform a levator aponeurosis advancement technique similar to that described in Chapter 10.
1 Putterman AM, Urist M. Surgical treatment of upper eyelid retraction. Arch Ophthalmol. 1972;87:401-405.
2 Chalfin J, Putterman AM. Muller’s muscle excision and levator recession in upper lid: Treatment of thyroid-related retraction. Arch Ophthalmol. 1979;97:1487-1491.
3 Putterman AM. Surgical treatment of thyroid-related upper eyelid retraction. Trans Am Acad Ophthalmol Otolaryngol. 1981;88:507-512.
4 Putterman AM, Fett DR. Muller’s muscle in the treatment of upper eyelid retraction: a 12-year study. Ophthalmic Surg. 1986;17:361-367.
5 Bassin R Putterman AM: Full Thickness resection ptosis procedure (in press).