Chapter 26 Treatment of Spinal Metastatic Tumors
• Histology plays paramount role in determination of tumor treatment. After a thorough radiological evaluation of the extent of systemic and spinal disease, a percutaneous computed tomography–guided biopsy is frequently the next step in the diagnostic algorithm, because 10% to 20% of the spine metastases have no known primary source. Determination of tumor histological type is of critical importance in determining the appropriate subsequent treatment.
• Treatment of metastatic spine tumors optimally requires a multidisciplinary approach that involves surgeons, radiation and medical oncologists, radiologists, and rehabilitation medicine physicians. However, the general treatment goal of patients with spinal metastases is palliation, because spinal metastases usually signal advanced metastatic disease with little hope of cure. Mechanical instability and high-grade cord compression secondary to solid tumors may require surgical decompression and stabilization as part of the palliative plan as long as survival time anticipated from the systemic neoplastic disease is greater than 3 months.
• The choice of surgical strategy and approach for spinal metastases remains predicated on the surgeon’s comfort, training, and experience. The definition of mechanical instability in patients with metastatic spinal tumors has recently been elucidated by an expert panel. The same stability classification used in trauma should not be applied to metastatic cases. Movement-related pain or pain relieved with recumbence may be considered to be a symptom of instability. Lytic lesions, subluxation and progressive deformity, extension into the posterior elements, and lesions that occupy more than 50% of the vertebral body and are accompanied by loss of height are also judged to be associated with instability. These symptoms and signs of instability and progressive neurological compromise may lead the treatment team to recommend surgical stabilization.
• When a ventral surgical approach for decompression and stabilization is employed, an anterior plate spanning one level above and one level below the vertebrectomy defect is generally used in order to buttress the cage or cement reconstruction. In posterior decompression, lateral mass or pedicle instrumentation is usually employed, spanning at least two levels above and below the tumor.
• Stereotactic spinal radiosurgery may provide excellent tumor control rates in radioresistant tumors. Radiosensitive tumors, such as lymphoma, multiple myeloma, plasmacytoma, and small cell lung carcinoma may be treated with radiation therapy even in the presence of cord compression.
Physicians will make over 1.5 million new diagnoses of cancer in 2010 in the United States, and over 500,000 people are expected to die from cancer in 2010 [fact sheet 2010]. Five-year survival rates in patients with cancer have improved to 68% (1999-2005) from 50% (1975-1977) as treatment techniques have advanced [fact sheet 2010]. Spine metastases, the most common site of bone metastasis, occur in 30% to 90% of terminal cancer patients.1–3 As patients continue to live longer with cancer, it is likely that spine metastatic disease rates will continue to climb.
The most common primary tumors that give rise to spine metastases are breast, lung, and prostate cancers, reflecting the high prevalence of these tumors.3 These primary tumors may spread to the spine through the arterial or venous systems, by direct extension, or via cerebrospinal fluid (CSF). Hematogenous spread (arterial or venous) is thought to be the most common route by which primary tumors metastasize to the spine. Because the vertebral bodies have an extensive arterial blood supply, tumor cells from distant primary lesions can travel to the spine and initiate metastatic disease.4 Venous spread occurs by flow through Batson’s plexus, the longitudinal network of valveless veins that connects vertebral veins with many venous beds (caval, portal, azygous, intercostal, pulmonary, and renal). Primary tumors may also spread by direct extension; lung cancer can extend posteriorly to the thoracic spine or superiorly to the cervical spine. Pelvic or abdominal cancers (prostate, bladder, and colorectal) can locally invade the lumbar or sacral spine. Metastasis through the CSF can occur spontaneously or after surgery for brain lesions. Multicentric disease (i.e., tumor in multiple vertebrae) can result from any of these mechanisms of spread.
Presentation
Pain
Pain, the most common first presenting symptom of spine metastasis, can have different mechanisms depending on the tumor’s interaction with the bony spine or the neural elements, and 83% to 95% of patients with spinal metastases complain of pain. Because pain often precedes other neurological symptoms, it should be carefully evaluated by clinicians.5,6 If tumor compresses a nerve root, pain that is burning and radiates down the leg in a dermatomal distribution (radicular pain) is a common symptom. If tumor causes a pathological fracture or collapse of a vertebral body, that collapse can narrow the foramina and cause radicular pain, or it may cause mechanical pain. Mechanical pain typically is worse with loading of the spine during sitting or standing, and it often does not improve with anti-inflammatory medications. Local or biological pain may also be experienced by patients with spine metastases; it is usually described as a deep ache that is worse at night. This type of pain can improve with anti-inflammatory medications or corticosteroids, and it is likely due to inflammation in the spine due to the presence of tumor. Tenderness to palpation over the spine may be evident on physical examination due to local pain from periosteal stretching and inflammation. Treatment of spine metastases often includes a goal of treatment of the patient’s pain, and the type of pain a patient experiences may guide that treatment. Local pain is often palliated with radiation treatment; mechanical pain may be best addressed with bracing or surgical stabilization.
Neurological Dysfunction
The second most common group of symptoms that patients with spinal metastases complain of is neurological deficit.7 Weakness in upper or lower extremities may result from epidural compression of the spinal cord, individual nerve roots, or the cauda equina by tumor. Tumor or fractured bone fragments may impinge on neural structures, and patients may also complain of autonomic problems including bowel, bladder (usually urinary retention), or sexual dysfunction. Asking patients directly about these problems should be routine, as the symptoms might not be revealed on initial history gathering. Without treatment, motor dysfunction usually progresses to paralysis. Dermatomal changes in sensation, including anesthesia, hyperesthesia, and parasthesia, usually occur with motor dysfunction and pain. Patients with spinal cord compression may complain of sensory abnormalities in a band-like distribution across the chest or abdomen. Myelopathy also results in hyperreflexia from chronic spinal cord compression. Diagnosis before these neurological deficits occur is important because neurological prognosis is related to the amount of neurological function at the time of diagnosis.4 Pain is usually experienced before a neurological deficit, but because of the extremely common prevalence of back pain in the general population, metastatic spine disease can be missed until deficit occurs. Any patient with a known history of cancer and a new complaint of back or neck pain should be thoroughly evaluated for spinal metastatic disease. As the thoracic spine is the most common location for metastasis to the spine, and degenerative problems there are less common, pain in the thoracic spine should cue clinicians to consider a neoplastic process in patients with new-onset thoracic pain.
Diagnosis
Patients with a newly diagnosed spinal lesion require a thorough diagnostic workup, which begins with a history and physical examination. Patients without cancer diagnosis require a standard evaluation and management of back pain, which would likely include initial observation and conservative treatment without extensive imaging or invasive diagnostic procedures. However, certain signs and symptoms may increase the probability of a neoplastic process and merit a more aggressive initial evaluation. Fatigue and unintended weight loss may result from a systemic process such as cancer. Furthermore, history of human immunodeficiency virus (HIV), chronic inflammatory conditions, smoking, hazardous occupational exposures, and familial cancer history increases the likelihood of a neoplasm. Nocturnal or morning back pain elevates the suspicion for neoplasm, and progressive pain during the course of the day is generally more indicative of degenerative lesions. In patients with a previous diagnosis of cancer, any back pain or neurological deficit should prompt a diagnostic evaluation in order to determine if the patient harbors any metastatic lesions. Prior to any decision regarding treatment, a thorough oncological staging evaluation must be performed according to the histology-specific protocols. Hematological, electrolyte, endocrinological, and cancer marker aberrations may aid in the diagnosis of tumor histological type and stage.
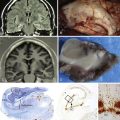
Imaging Studies
Plain radiographs often serve as an initial imaging evaluation of a patient with back pain, owing to their low cost and widespread availability. These studies may help in identifying significant abnormalities such as compression fractures, scoliosis, large lytic or sclerotic osseous lesions, and radiopaque extraossous lesions. However, in order to be apparent on plain radiographs, the lesions must reach a significant size, thereby making these studies a fairly insensitive modality in tumor diagnosis.8 Although radiographs may be an appropriate initial study in patients without history of cancer, they should not be used as a screening or diagnostic modality in patients with an elevated suspicion of spine tumors.
Universal nuclear body scans have become a standard component of histological staging for certain cancers. Nuclear scintigraphy (bone scan) permits detection of osseous remodeling throughout the skeletal system and has been reported to have 62% to 89% sensitivity in detection of spinal metastases.9 However, it is not specific for neoplasms and cannot differentiate tumors from regions of infection and inflammation. Furthermore, in order for a neoplasm to be detected on a bone scan, active osseous remodeling must be taking place, which is not always the case in sclerotic neoplasms. Single-photon emission computed tomography (SPECT) permits improved differentiation of neoplastic from inflammatory processes, because it detects the metabolic components of the lesion.10,11 It allows three-dimensional imaging of the lesion with sensitivity and specificity superior to standard bone scans. Finally, positron emission tomography (PET) using fluoride-18 (18F-PET) and 18F-fluorodeoxyglucose (18FDG-PET) provides a sensitive screening modality for neoplastic lesions through the body. 18F-PET detects regions of fluoride uptake and thereby skeletal remodeling. 18FDG-PET detects regions of high glucose uptake in the skeletal system and the soft tissues, thereby detecting hypermetabolic lesions that may signify a neoplastic, degenerative, inflammatory, or infectious process. However, correlation with concomitant MRI and CT scans generally allows high diagnostic specificity. Furthermore, 18FDG-PET has been shown to be a highly sensitive and specific screening modality in patients with solid tumors harboring spinal lytic and mixed lesions.12 The decreased sensitivity of 18FDG-PET in detection of sclerotic lesions may be associated with the acellular and therefore low metabolic nature of these lesions. PET imaging may also aid in the selection of biopsy targets in the setting of multiple lesions, because lesions with higher metabolic activity will likely produce higher diagnostic yield due to their high cellularity.
Percutaneous CT-guided biopsy is a frequent step in the diagnostic algorithm, because 10% to 20% of the spine metastases have no known source and determination of tumor histological type is of paramount importance in determining the appropriate treatment.13 Furthermore, in patients with distant cancer history a biopsy may be required in order to rule out a second malignancy. Modern large-bore needle biopsy techniques have excellent diagnostic yield and are generally performed as an outpatient procedure. Caution must be exercised when interpreting negative biospsies of blastic lesions, because they may be falsely negative owing to their acellular nature. Such patients may merit additional follow-up in order to monitor these lesions clinically and radiographically.
Metastases that originate from hypervascular primary tumors generally require preoperative digital subtraction angiography and embolization. Angiography allows evaluation of the vascularity and the blood supply of the tumor and delineation of the location of the artery of Adamkiewitz. Renal, thyroid, hepatocellular, neuroendocrine tumors and tumors that contain “angio” or “hemangio” in their name should generally undergo angiography and embolization when possible. Complete and even partial preoperative embolization of vascular tumors has been shown to significantly decrease intraoperative blood loss.14–16
Management
Advances in modern surgical technique, radiation delivery technology, and pharmacotherapy have extended the life expectancy and improved the life quality of cancer patients. Today, treatment of metastatic spine tumors requires a multidisciplinary approach that involves surgeons, radiation and medical oncologists, radiologists, and rehabilitation medicine physicians. However, the general treatment goal of patients with spinal metastases is palliation, because spinal metastases usually signal advanced metastatic disease with little hope of cure. Thus, patients succumb to systemic complications of visceral metastases and successful treatment of metastatic spinal tumors has not been convincingly shown to extend survival. The explicit goals of treatment of spinal metastatic tumors include preservation or restoration of neurological function, spinal stability and pain control, with minimal hospital stay and morbidity.
Modern treatment paradigms must incorporate surgical, radiation, and chemotherapeutic treatment options. One of the suggested treatment frameworks incorporates four considerations: neurological, oncological, mechanical, and systemic (NOMS).17 Spinal metastases frequently present with epidural extension resulting in cord and nerve root compression. The degree of epidural extension may dictate the possible treatment options, with patients with high-grade cord compression and myelopathy usually requiring surgical decompression. Several grading schemes have been used in the metastatic literature in order to describe the degree of epidural tumor extension. The Weinstein-Boriani-Biagini staging system divides the vertebral body into 12 radiating zones and five concentric layers in the axial plane.18 However, this system was initially designed to describe primary spinal tumors, and its application in the treatment of spinal metastases relies on the assumption that similar surgical principles may be applied to primary and metastatic tumors. A 6-point scale devised specifically for the purpose of describing the degree of epidural spinal cord compression secondary to spinal metastases was recently validated by the Spinal Oncology Study Group (SOSG).19 In this scale, the grade of 0 is assigned to bone only lesions, grade 1 is assigned to lesions with epidural extension but without cord compression, grade 2 is assigned to lesions causing cord compression but with CSF still visible around the cord, and grade 3 is assigned to lesions causing cord compression without CSF visible around the cord. Grade 1 lesions are further subdivided into three categories depending on the degree of epidural extension. Grades 2 and 3 tumors may result in neurological deficits and myelopathy and, with the exception of very radiosensitive tumors, generally require surgical decompression.
Tumor histological type plays a crucial role in appropriate selection of therapy. Small cell lung carcinoma and hematological malignancies such as lymphoma and plasmacytoma are exquisitely sensitive to radiation therapy and chemotherapy, and therefore usually do not require surgical decompression.20 Solid metastatic tumors display a range of radiosensitivity, with breast cancer being moderately sensitive, colon and non-small cell lung carcinomas being moderately resistant, and thyroid, renal, melanoma, and sarcoma metastases being highly radioresistant. The degree of radiosensitivity and the aggressive nature of the tumors should play an important role in determining the type of radiation treatment and the degree of surgical intervention that the patient will receive. Thus, a radiosensitive tumor without high-grade cord compression may respond well to conventional external beam radiation therapy (cEBRT) and not require surgical intervention, but a radioresistant tumor will likely require an operation in order to decompress the spinal cord and to provide adequate space between the tumor and the cord in order to deliver stereotactic radiosurgery (SRS). Of course, each patient and each case of metastatic tumor must be analyzed on its individual clinical characteristics and the collective evaluation and experience of the treating team of physicians and surgeons.
Metastatic tumors frequently invade and weaken the vertebral bodies and pedicles, thereby undermining the mechanical stability of the spine. Radiation therapy and chemotherapy cannot restore spinal stability, and patients who manifest evidence of instability require instrumented stabilization, regardless of tumor histological type or their neurological status. The definition of mechanical instability in patients with metastatic spinal tumors remains controversial. Previous definitions of spinal instability in the setting of metastatic disease relied on the three-column spinal model developed by Denis and attempted to modify this model in order to apply it to cancer patients.21 However, the Denis model was developed to define instability in the setting of spinal trauma and the mechanics and the extent of injury to the osseous and ligamentous structures, as well as the healing potential, are drastically different in the settings of trauma and spinal metastases. Activity-related neck or back pain is generally accepted as one of the defining symptoms of mechanical instability. The SOSG expert panel has recently defined spine instability as “loss of spinal integrity as a result of a neoplastic process that is associated with movement-related pain, symptomatic or progressive deformity, or neural compromise under physiological loads.”22 The panel developed a 6-point Spine Instability Neoplastic Score (SINS), which incorporates multiple radiographic parameters in addition to the presence of mechanical pain (Table 26.1). Junctional tumor location was considered to be the most unstable, followed by the mobile (C3-C6, L2-L4), semirigid (T3-T10), and rigid spine (S2-S5). Movement-related pain or pain relieved with recumbence was considered to be a symptom of instability. Lytic lesions, subluxation and progressive deformity, extension into the posterior elements, and lesions that occupy more than 50% of the vertebral body and are accompanied by loss of height were also judged to be associated with instability.
| Location | |
| Junctional (occiput-C2, C7-T2, T11-L1, L5-S1) | 3 |
| Mobile spine (C3-C6, L2-L4) | 2 |
| Semirigid (T3-T10) | 1 |
| Rigid (S2-S5) | 0 |
| Pain | |
| Yes | 3 |
| Occasional pain but not mechanical | 1 |
| Pain-free lesion | 0 |
| Bone lesion | |
| Lytic | 2 |
| Mixed (lytic/blastic) | 1 |
| Blastic | 0 |
| Radiographic spinal alignment | |
| Subluxation/translation present | 4 |
| De novo deformity (kyphosis/scoliosis) | 2 |
| Normal alignment | 0 |
| Vertebral body collapse | |
| >50% collapse | 3 |
| <50% collapse | 2 |
| No collapse with >50% body involved | 1 |
| None of the above | 0 |
| Posterolateral involvement of spinal elements | |
| Bilateral | 3 |
| Unilateral | 1 |
| None of the above | 0 |
| Status | Total Score |
| Stable | 0-6 |
| Indeterminate | 7-12 |
| Unstable | 13-18 |
Adapted from Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine. 2010;35(22):E1221-1229.
Surgery
The most convincing data supporting surgical decompression resulted from a prospective randomized trial conducted by Patchell and associates.23 The trial included patients with solid metastatic spinal tumors causing spinal cord compression, which was defined as any degree of cord displacement. The patients had to have at least one neurological sign or symptom, which may have been pain, and could not be paraplegic longer than 48 hours. The trial excluded patients with radiosensitive tumors such as hematological and germ cell malignancies and patients with previous radiation that precluded the study radiation dose. Patients were randomized to two trial groups: the first group received 30 Gy fractionated radiation therapy and the second group first underwent surgical decompression followed by radiation. The study was stopped at the midpoint of the enrollment owing to the clear superiority of the surgery group in the ability to ambulate, duration of ambulation, maintenance of continence, decreased use of opioids and corticosteroids, and extended survival. The limitations of the study include randomization of patients with instability to the radiation arm as well as the surgery arm, outdated spinal stability criteria, low benchmark for ambulation (only four steps), and lack of requirement for instrumented stabilization in the surgery arm.
Several grading systems have been devised in order to tailor the extent of surgical intervention to the expected survival of the patient. Tomita and colleagues proposed a 10-point scale that considered three prognostic factors: tumor histological type, the extent of visceral metastases, and the number of skeletal metastases.24 They recommended that patients with slowly growing tumors (breast, thyroid) and moderately growing tumors (renal, uterus) and solitary spine metastases undergo en bloc tumor excision. Patients with rapidly growing tumors (lung, stomach) and patients with more extensive visceral and skeletal burden were recommended a spectrum of intralesional excision, palliative decompression, or supportive care. Tokuhashi and co-workers proposed a similar scale which in addition to the above-mentioned factors included the general performance status of the patient and the extent of neurological deficits.25 They used these factors in order to estimate the expected survival and recommended that patients with longer than 1-year survival should undergo excisional surgery (goal of en bloc spondylectomy), and patients with expected survival between 6 months and 1 year should undergo palliative surgery (piecemeal cord decompression and stabilization).
The choice of surgical strategy and approach for spinal metastases remains predicated on the surgeon’s comfort and training. The vertebral body represents the most common site of spinal metastases. Thus, anterior approaches often provide the most direct access to these tumors. The transcervical approach provides direct access to the subaxial cervical spine and most spine surgeons are facile with this approach. The transoral and transmandibular approaches have been traditionally used in order to access the craniocervical junction and the atlantoaxial spine; however, recently transnasal and transcervical approaches have also been employed in order to access these regions. Manubriotomy, sternotomy, or the trapdoor approach may be required in order to provide ventral access to the upper thoracic spine (T1-T4). However, the great vessels and mediastinal contents generally complicate ventral access to the upper thoracic spine. The above-mentioned complex anterior approaches to the craniocervical junction and the upper thoracic areas are generally used in order to treat primary tumors, since the palliative nature of metastatic tumor treatment rarely justifies the potential morbidity of these approaches. A thoracotomy provides direct vertebral body access at the T5-L1 levels.26,27 Access to T5-T7 usually requires sacrifice of the rib one level above the target vertebral level, and access to T8-L1 requires sacrifice of the rib two levels above. In order to visualize T11-L1 vertebral bodies, the diaphragm usually has to be reflected. The retroperitoneal approach provides ventral access to L2-L5 and sacral regions. Head and neck, thoracic, general, and vascular surgeons may be required to provide these ventral approaches, and are recommended if the patient had previous radiation, anterior surgery, or extensive tumor burden ventral to the spine.
Patients with limited lung capacity and previous neck, thoracic, or abdominal surgery or radiation may not be optimal candidates for anterior approach surgery. Posterior approaches provide direct access to the spinal cord and thereby allow direct decompression without extensive osseous work.28,29 While the posterior approach is rarely employed in order to access cervical vertebral bodies, costotransversectomy and transpedicular approaches provide access to the thoracic and lumbar vertebral bodies. In the thoracic spine, nerve roots below T2 may be sacrificed in order to obtain posterolateral access to the anterior column. In the lumbar spine, the nerve roots must be preserved and may be retracted medially in order to provide ventral access.
Combined anterior and posterior approaches may be implemented in order to achieve circumferential cord decompression and spinal reconstruction. Although en bloc tumor resection may be achieved via a posterior approach in the lumbar spine, a combined anterior-posterior approach is generally required in the thoracic spine. Combined approaches are generally associated with higher surgical morbidity.30
Vertebral body reconstruction may be accomplished with the help of Steinman pins with polymethylmethacrylate (PMMA), PMMA in a chest tube, mesh or expandable titanium cages, or polyetheretherketone (PEEK) cages.31 When a ventral approach is employed, an anterior plate spanning one level above and one level below the vertebrectomy defect is generally used in order to buttress the cage or cement reconstruction. In posterior decompression, posterolateral lateral mass or pedicle instrumentation is usually employed, spanning at least two levels above and below the tumor.
Vertebroplasty/Kyphoplasty
Vertebroplasty involves injection of PMMA into the vertebral body through a percutaneously placed transpedicular needle. During kyphoplasty, prior to PMMA injection, a balloon is inflated inside the vertebral body in order to attempt to restore vertebral body height. Both procedures have been shown to successfully control back pain in patients with spinal metastases. The suggested mechanisms of action include thermoablation of pain receptors secondary to the heat dissipated by the injected cement and to partial restoration of stability in a fractured vertebral body. Patients with back pain but without cord compression or gross instability that requires surgical stabilization may undergo vertebroplasty or kyphoplasty in order to provide pain relief in conjunction with radiation or medical therapy. Although successful tumor treatment with radiation may provide eventual pain control after several weeks, vertebroplasty generally has an instantaneous or rapid onset of effect. Extravasation of the cement into the vasculature or into the spinal canal represents the largest proportion of procedure-related complications. Furthermore, cement may embolize into the lungs and other distal organs. However, these are generally radiographic findings without clinical consequences. In a series of 56 patients, 84% reported significant or complete pain relief without significant complications related to the procedure.32 Furthermore, prophylactic vertebroplasty may be performed in patients undergoing stereotactic radiosurgery.33 This may be an appropriate treatment in patients with lytic lesions that occupy a large portion of the vertebral body who are at high risk for fracture after radiation treatment.
Adjuvant Therapies
Radiation Therapy
Modern radiation therapy allows precise and safe delivery of radiation to spinal tumors, and available treatments range from conventional fractionated schemes to high-dose stereotactic radiosurgery. Maranzano and Latini prospectively evaluated 209 patients with a wide range of primary histological types that received cEBRT with a dose of 30 Gy in two fractionation schemes. Seventy-six percent of patients were ambulatory after treatment, with 51% of nonambulatory patients regaining ambulation.34 Importantly, the results varied dramatically, depending on the histological type, with breast, lymphoma, and plasmacytoma responding to radiation much better than liver, bladder, or renal cancers. Thus, cEBRT remains an important treatment component for radiosensitive tumors, whether used as primary treatment or as a postoperative adjunct. Because cEBRT delivers radiation to a wide field surrounding the tumor, it is important to wait at least 2 to 4 weeks prior to initiating postoperative radiation in order to avoid wound-healing complications. Furthermore, preoperative cEBRT has been shown to be associated with significant elevation in the wound complication rate.
Tumors that display poor response to conventional fractionated schemes generally respond well to single-fraction high-dose therapy delivered during spinal stereotactic radiosurgery treatments. Gerszten and associates used CyberKnife technology to treat 60 renal cell carcinoma spinal metastases, most of which failed cEBRT.35 Pain control was achieved in 89% of the treated cases. Subsequently, a larger series that included 93 renal metastases, treated by the same group, displayed an 87% radiographic tumor control rate.36 The same series also included 38 melanoma lesions, which showed 96% pain control and 75% radiographic control rates. Furthermore, Yamada and colleagues prospectively followed 103 radioresistant metastatic tumors treated with image-guided radiation therapy (IGRT).37 The overall actuarial tumor control rate was 90% after a median follow-up of 15 months, with tumors receiving 24-Gy single-fraction treatments showing better control rates than tumors that received lower doses. Spinal stereotactic radiotherapy allows delivery of high doses of tumoricidal radiation with outstanding spatial precision, generally requiring as little as 2 mm between the cord and the tumor. Furthermore, patients may undergo spinal stereotactic radiosurgery shortly before or after surgery without the wound complications associated with cEBRT.38
Chemotherapy
Advancements in chemotherapeutic agents have played a large role in prolongation of survival and occasional cure of many cancers. However, spine metastases generally appear to be resistant to chemotherapy and represent a manifestation of advanced cancer with multiple systemic metastases. However, certain tumor histological types such as superior sulcus tumors, germ cell tumors, high-risk neuroblastomas, Ewing’s sarcomas, and osteogenic sarcomas have been shown to benefit from neoadjuvant chemotherapy followed by resection.39–41 Neoadjuvant therapy with etoposide and cisplatin has dramatically improved the potential for negative-margin resection of superior sulcus non-small cell lung tumors and has improved survival.39
In patients with breast or prostate cancer antihormone therapy has been shown to successfully treat patients with appropriate hormone receptors expressed by their tumors. Letrozole, anastrozole, and exemestane, which are aromatase inhibitors, and tamoxifen, which is a selective estrogen receptor modulator (SERM), have been effective against breast tumors.42 Androgen suppression with gonadotropin-releasing hormone (GnRH) and flutamide has been successful in treating men with prostate cancer.43 Unfortunately, spine metastases generally occur during or after treatment with these agents and are therefore tumor clones that are resistant to hormone therapy.
Bisphosphonates
Cancer patients frequently have poor bone quality secondary to radiation, chemotherapy, long-term glucocorticoid therapy, decreased activity, and advanced age. Furthermore, many spine metastases manifest as lytic vertebral lesions, thereby predisposing patients to pathological fractures. Bisphosphones, which inhibit osteoclastic activity and suppress bone resorption, have been shown to reduce the fracture risk, relieve local pain, and decrease hypercalcemia in patients with breast cancer, multiple myeloma, and other lytic histological types.44
Corticosteroids
Corticosteroids remain an integral part of pharmacotherapy in patients with spinal metastases. Their anti-inflammatory effects provide pain relief in patients with biological tumor-related back pain. Furthermore, they may reduce cord edema secondary to cord compression and have been shown to improve neurological function in animal models of metastatic cord compression.45,46 Initial animal studies used very high doses (96 mg/day), but further studies failed to show a difference in functional outcome after treatment with high (100 mg) and low (10 mg) doses.47 Furthermore, in lymphoma and multiple myeloma patients, corticosteroids play a role in oncolytic treatment of the tumors.
Fisher C.G., DiPaola C.P., Ryken T.C., et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine. 2010;35(22):E1221-E1229.
Fourney D.R., Gokaslan Z.L. Anterior approaches for thoracolumbar metastatic spine tumors. Neurosurg Clin North Am. 2004;15(4):443-451.
Gerszten P.C., Burton S.A., Ozhasoglu C., Welch W.C. Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine. 2007;32(2):193-199.
Gokaslan Z.L., York J.E., Walsh G.L., et al. Transthoracic vertebrectomy for metastatic spinal tumors. J Neurosurg. 1998;89(4):599-609.
Patchell R.A., Tibbs P.A., Regine W.F., et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648.
Tomita K., Kawahara N., Kobayashi T., et al. Surgical strategy for spinal metastases. Spine. 2001;26(3):298-306.
Please go to expertconsult.com to view the complete list of references.
1. Wong D.A., Fornasier V.L., MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine. 1990;15(1):1-4.
2. Cobb C.A.3rd, Leavens M.E., Eckles N. Indications for nonoperative treatment of spinal cord compression due to breast cancer. J Neurosurg. 1977;47(5):653-658.
3. Constans J.P., de Divitiis E., Donzelli R., et al. Spinal metastases with neurological manifestations. Review of 600 cases. J Neurosurg. 1983;59(1):111-118.
4. Arguello F., Baggs R.B., Duerst R.E., et al. Pathogenesis of vertebral metastasis and epidural spinal cord compression. Cancer. 1990;65(1):98-106.
5. Bach F., Larsen B.H., Rohde K., et al. Metastatic spinal cord compression. Occurrence, symptoms, clinical presentations and prognosis in 398 patients with spinal cord compression. Acta Neurochir (Wien). 1990;107(1-2):37-43.
6. Posner J.B. Back pain and epidural spinal cord compression. Med Clin North Am. 1987;71(2):185-205.
7. Greenberg H.S., Kim J.H., Posner J.B. Epidural spinal cord compression from metastatic tumor: results with a new treatment protocol. Ann Neurol. 1980;8(4):361-366.
8. Gabriel K., Schiff D. Metastatic spinal cord compression by solid tumors. Semin Neurol. 2004;24(4):375-383.
9. Peterson J.J., Kransdorf M.J., O’Connor M.I. Diagnosis of occult bone metastases: positron emission tomography. Clin Orthop Relat Res. 2003(Suppl 415):S120-S128.
10. Savelli G., Maffioli L., Maccauro M., et al. Bone scintigraphy and the added value of SPECT (single photon emission tomography) in detecting skeletal lesions. Q J Nucl Med. 2001;45(1):27-37.
11. Gates G.F. SPECT imaging of the lumbosacral spine and pelvis. Clin Nucl Med. 1988;13(12):907-914.
12. Laufer I., Lis E., Pisinski L., et al. The accuracy of [18F]fluorodeoxyglucose positron emission tomography as confirmed by biopsy in the diagnosis of spine metastases in a cancer population. Neurosurgery. 2009;64(1):107-113. discussion 113-104
13. Cahill D.W. Surgical management of malignant tumors of the adult bony spine. South Med J. 1996;89(7):653-665.
14. Sundaresan N., Choi I.S., Hughes J.E., et al. Treatment of spinal metastases from kidney cancer by presurgical embolization and resection. J Neurosurg. 1990;73(4):548-554.
15. Olerud C., Jonsson H.Jr., Lofberg A.M., et al. Embolization of spinal metastases reduces preoperative blood loss. 21 patients operated on for renal cell carcinoma. Acta Orthop Scand. 1993;64(1):9-12.
16. Manke C., Bretschneider T., Lenhart M., et al. Spinal metastases from renal cell carcinoma: effect of preoperative particle embolization on intraoperative blood loss. AJNR Am J Neuroradiol. 2001;22(5):997-1003.
17. Bilsky M., Smith M. Surgical approach to epidural spinal cord compression. Hematol Oncol Clin North Am. 2006;20(6):1307-1317.
18. Yao K.C., Boriani S., Gokaslan Z.L., Sundaresan N. En bloc spondylectomy for spinal metastases: a review of techniques. Neurosurg Focus. 2003;15(5):E6.
19. Bilsky M.H., Laufer I., Fourney D.R., et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13(3):324-328.
20. Bacci G., Savini R., Calderoni P., et al. Solitary plasmacytoma of the vertebral column. A report of 15 cases. Tumori. 1982;68(3):271-275.
21. Cybulski G.R. Methods of surgical stabilization for metastatic disease of the spine. Neurosurgery. 1989;25(2):240-252.
22. Fisher C.G., DiPaola C.P., Ryken T.C., et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine. 2010;35(22):E1221-E1229.
23. Patchell R.A., Tibbs P.A., Regine W.F., et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648.
24. Tomita K., Kawahara N., Kobayashi T., et al. Surgical strategy for spinal metastases. Spine. 2001;26(3):298-306.
25. Tokuhashi Y., Matsuzaki H., Oda H., et al. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine. 2005;30(19):2186-2191.
26. Fourney D.R., Gokaslan Z.L. Anterior approaches for thoracolumbar metastatic spine tumors. Neurosurg Clin North Am. 2004;15(4):443-451.
27. Gokaslan Z.L., York J.E., Walsh G.L., et al. Transthoracic vertebrectomy for metastatic spinal tumors. J Neurosurg. 1998;89(4):599-609.
28. Wang J.C., Boland P., Mitra N., et al. Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1(3):287-298.
29. Fourney D.R., Abi-Said D., Lang F.F., et al. Use of pedicle screw fixation in the management of malignant spinal disease: experience in 100 consecutive procedures. J Neurosurg. 2001;94(suppl 1):25-37.
30. Xu R., Garces-Ambrossi G.L., McGirt M.J., et al. Thoracic vertebrectomy and spinal reconstruction via anterior, posterior, or combined approaches: clinical outcomes in 91 consecutive patients with metastatic spinal tumors. J Neurosurg Spine. 2009;11(3):272-284.
31. York J.E., Walsh G.L., Lang F.F., et al. Combined chest wall resection with vertebrectomy and spinal reconstruction for the treatment of Pancoast tumors. J Neurosurg. 1999;91(Suppl 1):74-80.
32. Fourney D.R., Schomer D.F., Nader R., et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 2003;98(Suppl 1):21-30.
33. Gerszten P.C., Germanwala A., Burton S.A., et al. Combination kyphoplasty and spinal radiosurgery: a new treatment paradigm for pathological fractures. J Neurosurg Spine. 2005;3(4):296-301.
34. Maranzano E., Latini P. Effectiveness of radiation therapy without surgery in metastatic spinal cord compression: final results from a prospective trial. Int J Radiat Oncol Biol Phys. 1995;32(4):959-967.
35. Gerszten P.C., Burton S.A., Ozhasoglu C., et al. Stereotactic radiosurgery for spinal metastases from renal cell carcinoma. J Neurosurg Spine. 2005;3(4):288-295.
36. Gerszten P.C., Burton S.A., Ozhasoglu C., Welch W.C. Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine. 2007;32(2):193-199.
37. Yamada Y., Bilsky M.H., Lovelock D.M., et al. High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys. 2008;71(2):484-490.
38. Rock J.P., Ryu S., Shukairy M.S., et al. Postoperative radiosurgery for malignant spinal tumors. Neurosurgery. 2006;58(5):891-898. discussion 891-898
39. Rusch V.W., Giroux D.J., Kraut M.J., et al. Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Clin Oncol. 2007;25(3):313-318.
40. Sandberg D.I., Bilsky M.H., Kushner B.H., et al. Treatment of spinal involvement in neuroblastoma patients. Pediatr Neurosurg. 2003;39(6):291-298.
41. Ilaslan H., Sundaram M., Unni K.K., Dekutoski M.B. Primary Ewing’s sarcoma of the vertebral column. Skeletal Radiol. 2004;33(9):506-513.
42. Morandi P., Rouzier R., Altundag K., et al. The role of aromatase inhibitors in the adjuvant treatment of breast carcinoma: the M.D. Anderson Cancer Center evidence-based approach. Cancer. 2004;101(7):1482-1489.
43. Conti P.D., Atallah A.N., Arruda H., et al. Intermittent versus continuous androgen suppression for prostatic cancer. Cochrane Database Syst Rev. 2007(4):CD005009.
44. Hillner B.E., Ingle J.N., Berenson J.R., et al. American Society of Clinical Oncology guideline on the role of bisphosphonates in breast cancer. American Society of Clinical Oncology Bisphosphonates Expert Panel. J Clin Oncol. 2000;18(6):1378-1391.
45. Turner S., Marosszeky B., Timms I., Boyages J. Malignant spinal cord compression: a prospective evaluation. Int J Radiat Oncol Biol Phys. 1993;26(1):141-146.
46. Delattre J.Y., Arbit E., Rosenblum M.K., et al. High dose versus low dose dexamethasone in experimental epidural spinal cord compression. Neurosurgery. 1988;22(6 Pt 1):1005-1007.
47. Vecht C.J., Haaxma-Reiche H., van Putten W.L., et al. Initial bolus of conventional versus high-dose dexamethasone in metastatic spinal cord compression. Neurology. 1989;39(9):1255-1257.