15 Treatment of crow’s feet
Summary and Key Features
• Treatment of crow’s feet with botulinum toxin is safe and effective, with predictable cosmetic results
• Preoperative assessment of the periocular region, including analysis of dynamic and static rhytides, lower lid laxity, and upper lid ptosis, can improve the precision and safety of treatments
• A snap-test can be useful for measuring lower lid laxity
• Stretching the skin and side lighting can help avoid injection into superficial vessels and resultant ecchymoses
• Superficial injections into the dermis, combined with frequent needle changes, may reduce injection discomfort, ecchymoses, and / or spread into nearby lip elevators
• Adjunctive non-invasive procedures of the periocular region, including laser resurfacing, pigment laser treatments, and soft tissue augmentation, may be combined with crow’s feet injections for more comprehensive periorbital rejuvenation
Anatomy of ‘crow’s feet’ lateral orbital rhytides
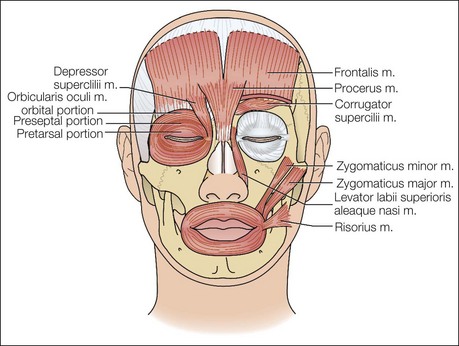
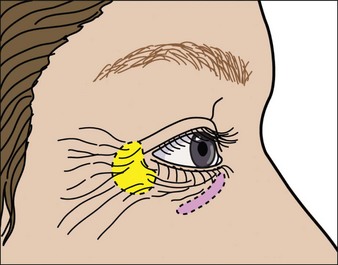
In addition, rhytides develop in the setting of hyperkinetic muscle contractions of the orbicularis oculi, an elliptical muscle that functions in closing the eyelids and protecting the globe by acting as the sphincter of the eye. The orbicularis oculi encircles the eye, with a predominantly vertical orientation at the lateral canthus, and has three distinct subparts: the orbital, palpebral, and lacrimal portions. The lacrimal portion of the muscle runs deep to the lacrimal sac and inserts on the upper and lower eyelids at the tarsal plates. Contraction of this part of the muscle draws the eyelids against the globe and compresses the lacrimal sac, thus assisting tear flow. The palpebral portion is the innermost aspect of the muscle and passes into the eyelid superficial to the septum from the bifurcation of the medial palpebral ligament to the lateral palpebral raphe. The palpebral portion is subdivided into preseptal and pretarsal components, and each portion is superficial to the corresponding named portion of the eyelid. Contraction of the palpebral portion of the orbicularis oculi provides less forceful involuntary closure of the eyelid, as with blinking. The orbital portion represents the outermost aspect of the muscle overlying the bony orbit, with origins at the nasal process of the frontal bone, frontal process of the maxilla, and the medial palpebral ligament. This portion of the muscle blends into surrounding musculature, interdigitating at its superior aspect with the frontalis muscle, corrugator supercilii, depressor supercilii, and procerus muscles, and at its inferior margins with the levator labii superioris alaeque nasi, levator labii superioris, and zygomaticus minor and major muscles (Fig. 15.1). By providing forceful eye closure and eyebrow depression, this outer aspect of the muscle pulls on overlying skin and contributes most to the formation of lateral orbital rhytides. The outer orbicularis is typically treated with botulinum toxin, although the preseptal aspect of the inferior palpebral portion of the orbicularis oculi can be treated in some situations as well. The zygomaticus muscles, both major and minor, can also contribute to inferior periorbital rhytides, as contraction of this muscle elevates skin superiorly into the periocular region. The zygomaticus major originates deep to the orbicularis oculi muscle at the zygomatic bone just anterior to the zygomaticotemporal suture line and courses diagonally where it inserts into the modiolus, lifting the corner of the mouth. The zygomaticus minor muscle courses from the zygomatic bone and inserts into the upper lip, where it causes upward and lateral elevation of the oral commissure. The risorius muscle originates from the connective tissue and fascia overlying the parotid gland, platysma, and runs horizontally towards the oral commissure, where it inserts into the modiolus. Contraction of this muscle pulls the mouth laterally, retracting the corners of the mouth.
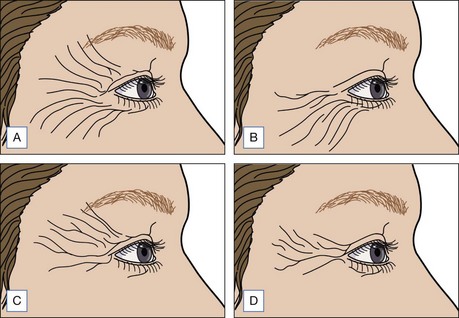
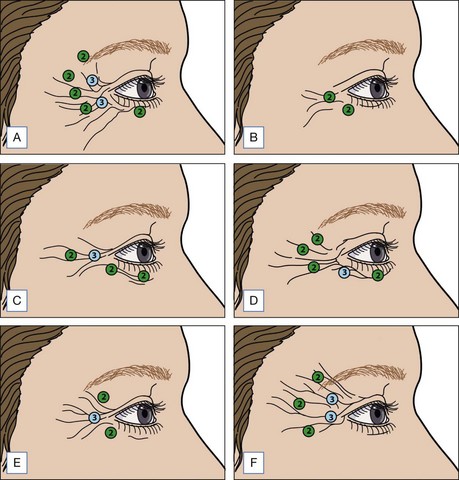
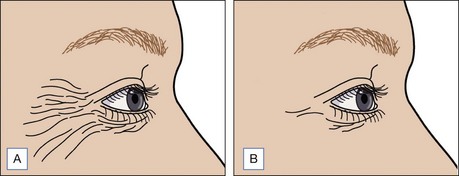
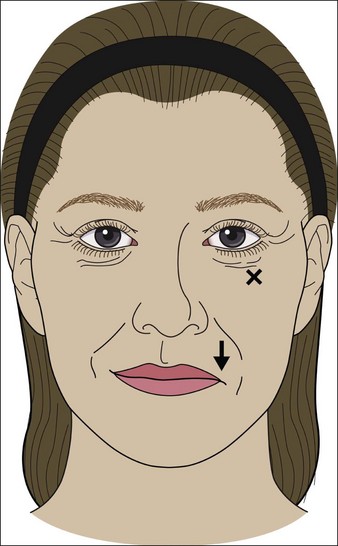
In an article by Kane et al, four lateral canthal rhytid patterns were identified, reflecting divergent muscle contraction patterns: (1) full-fan distribution of rhytides from the upper eyelid to the upper cheek, (2) rhytides of the lower lid / upper cheek, (3) rhytides of the upper eyelid skin down to the lateral canthus, and (4) central zone of rhytides at the lateral canthus only (Fig. 15.2). Although standard injection points can be helpful for beginner injectors, treatment should be individualized to take into account this diversity in lateral canthal rhytides, which may deviate from published patterns and require care and attention to understand, document, and address specifically. Some patients may exhibit right–left differences in the distribution and size of lateral canthal rhytides. Lateral canthal rhytides are generally classified as static, dynamic, or a combination of the two. Dynamic rhytides develop secondary to repeated muscle contractions, and remit during relaxation, and hence are most immediately amenable to treatment with botulinum toxin. Static rhytides, which are present in the absence of muscle contractions, may best be treated with soft tissue fillers or resurfacing procedures, and will be addressed later in this chapter. Alternatively, ongoing and repeated treatments with botulinum toxin may soften static rhytides over long time intervals, as reduction of coincident dynamic creases reduces the incidence of repeated microtrauma to the underlying collagen and elastin. Botulinum toxin treatments may also prevent the extension or deepening of static creases through a similar mechanism.
Preoperative assessment
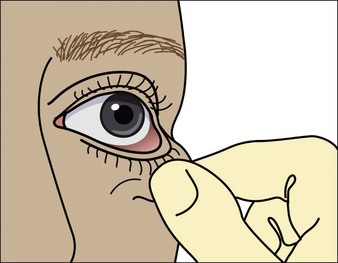
Pre-existing ocular conditions such as persistent or intermittent tearing, dry eyes, or previous LASIK surgery may be associated with increased risk of dry eyes after botulinum toxin treatment. As patients may not volunteer the use of over-the-counter medications, it may be informative to question them specifically regarding the use of eye drops for dry eyes. If there is a concern that decreased tear production may exist before treatment, a Schirmer’s test can measure tear production using calibrated strips of filter paper placed within the lower eyelid, or a rose bengal test can employ a dye to detect corneal scratches associated with dry eye. Injection treatments around the eye may be modified in the context of systemic conditions with ocular manifestations, including Graves’ disease, Hashimoto’s thyroiditis, Sjögren’s syndrome, and other collagen vascular diseases. A lower eyelid ‘snap-test’ can estimate the risk for development of ectropion or scleral show after infraorbital toxin injections. The snap is assessed by pulling gently downward and outward on the lower eyelid and then quickly releasing; a rapid return to the rest position without requiring an eyelid blink suggests a fully functional orbicularis muscle and a low risk of excessive eye rounding after botulinum toxin injections (Fig. 15.3). A positive test is defined as a slow return to baseline, with the eyelid staying in a distracted position until the patient blinks, or until several seconds elapse and the lid very slowly resumes its normal apposition against the globe.
Treatment
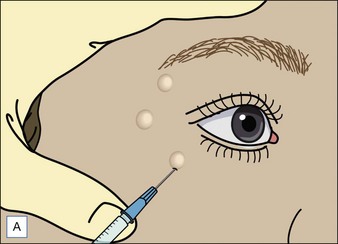
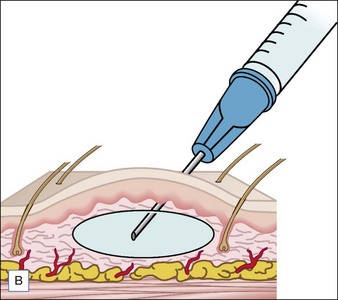
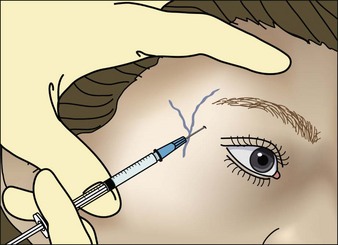
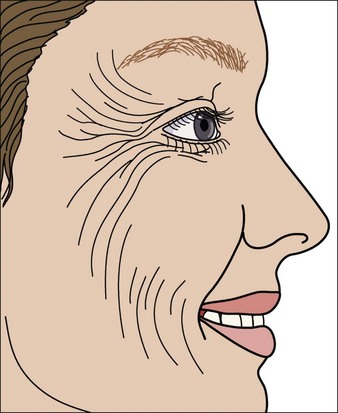
Although treatment of crow’s feet with botulinum toxin has only recently been approved for abobotulinumtoxinA and is currently pending for onabotulinumtoxinA, it is a highly effective and frequently sought after procedure. When performing injections in the periocular region, the patient is typically seated upright or slightly reclined. Although some physicians may find standing on the same side as the treatment area more natural, others may choose to stand on the opposite side so that the needle is pointed away from the eye, and yet others may stand facing the patient. To minimize the risk of ecchymoses, injections are placed as a wheal superficially into the dermis rather than deep into the muscle (Fig. 15.4). Cleansing the skin with alcohol prior to treatment, in addition to side lighting and stretching of the skin, may help to identify any superficial vessels along the treatment area (Fig. 15.5). Injections should be performed meticulously and slowly, with the needle changed frequently to prevent it from becoming blunt. The hand is typically braced to avoid inadvertent sideways motion or deeper placement, both of which may predispose to trauma and bruising. It goes without saying that the needle tip should be aimed to minimize the risk of inadvertently spearing the globe. Some injectors prefer to insert the needle head on vertically, and others insert the needle from the side, almost tangential to the skin, occasionally tenting the skin. Vertical injections are associated with a marginal higher risk of deeper than desired placement, and lateral injections course through more dermis, thus being at greater likelihood of perforating a small blood vessel. Overall, superficial injections no more than 2–3 mm deep minimize the risk of spread or direct injection into nearby lip elevators, including the zygomaticus minor and major muscles. Smaller volumes may aid with precision and prevention of migration; on the other hand, more dilute solutions may enable a wider radius of action, and reduce the number of injections needed.
For standard treatment of periorbital rhytides, injections are commonly placed 1.5 cm from the lateral canthus or 1 cm lateral to the bony orbital rim. Some injectors place the injection on or even inside the orbital rim with equal effect and no increase in side effects. The injected dose and pattern is adjusted to account for individual patient preference, as well as the strength and size of the orbicularis oculi muscle (Figs 15.6, 15.7). In general, 6–18 units of onabotulinumtoxinA (Botox®) are injected per side as three to four injections along a 90–180° arc, spaced at 1–1.5 cm intervals, as recommended in the studies by Matarasso & Matarasso and by Lowe et al. In the latter study, evaluating the safety and efficacy of 6, 12, and 18 units of onabotulinumtoxinA (Botox®) in the treatment of crow’s feet, there was no statistically significant difference in the efficacy or safety profile among the tested doses. In the trials by Lowe and co-workers, at 4 weeks post-treatment 89% of patients in the 6-unit group and 95% of patients in the 12- and 18-unit group had an improvement of at least 1 point from baseline on the Facial Wrinkle Scale; these authors also noted that a second injection of the same dose resulted in a longer duration of action compared with the first injection, with up to half of the patients still one grade above baseline 16 weeks after the second injection. Notably, like many such small, relatively underpowered studies, this research was susceptible to type II error, i.e. the failure to detect small real differences that may have been statistically and clinically significant. In general, smaller doses may be sufficient for women with minimal movement of the lateral canthal rhytides, whereas certain men, patients with stronger muscles, and those with larger faces may need higher cumulative doses. In patients with protuberant globes, lowering the dose may reduce the risk for ectropion or incomplete eyelid closure. When injecting lower malar crow’s feet, especially those that blend into the diagonal rhytides of the mid and lateral cheeks, extreme caution should be exercised as direct injection or spread into the zygomaticus major and minor muscles can cause ipsilateral facial paralysis and lip ptosis. In order to prevent such complications, injections below the level of the superior zygomatic arch should be avoided. Again, discussing with patients why far lower infraorbital rhytides cannot be safely injected with toxin may reduce their disappointment when these persist after treatment.
Adjunctive treatments
For instance, botulinum toxin pretreatment of the periorbital region has been shown to impede recurrence and severity of dynamic rhytides after laser resurfacing. In a prospective, randomized, placebo-controlled study by Yamauchi et al, of 33 patients receiving either 18 units of onabotulinumtoxinA (Botox®) or saline into the periorbital region followed 2–6 weeks later by erbium–YAG resurfacing, patients receiving onabotulinumtoxinA (Botox®) demonstrated a more significant reduction in periorbital rhytides as well as textural and pigmentary changes. In a separate study by Zimbler et al, in which 10 patients were pre-treated on one side of the face with onabotulinumtoxinA (Botox®) 1 week prior to laser resurfacing, the greatest improvement in facial rhytides was observed in the crow’s feet region that had been pre-treated with onabotulinumtoxinA (Botox®). Ideally, pre-treating patients with botulinum toxin and then repeating treatment well into the postoperative period could enhance and prolong the aesthetic effects of laser resurfacing. In the same manner, the effects of soft tissue augmentation in the periorbital region may last longer when muscle activity is inhibited with botulinum toxin. Prominent periorbital hollows may disappear after volume replacement with hyaluronic acids fillers, thus contributing to global facial rejuvenation and the beneficial effect of rhytid reduction induced by toxin injections (Fig. 15.8). Given that areas of volume loss often develop in regions with greater movement, a comprehensive strategy that combines soft tissue augmentation and chemodenervation may optimize patient outcomes.
A patient presents to you requesting treatment of her crow’s feet (Fig. 15.9). How do you counsel this patient?
Complications
Pearl 9
When bruising occurs, treatment with pulsed-dye laser at non-bruising fluences can speed resolution.
Although rare, lip ptosis can occur after botulinum toxin injections for crow’s feet (Fig. 15.10). This can result either from direct intramuscular injection or spread of toxin into the zygomaticus major, zygomaticus minor, levator labii superioris alaeque nasi, or levator labii superioris muscles, all of which have fibers that blend with the orbicularis oculi muscle. Lip ptosis has been estimated to occur in far less than 1% of treated patients and is characterized by an inability to elevate the corner of the mouth. Patients who have undergone facial surgery prior to treatment may be at increased risk of inadvertent injection or diffusion into the lip elevators due to aberrant muscle fiber realignment or planes of dissection. Although there is no treatment for this complication, Lowe et al reported in 2002 that muscle function should normalize by 6 weeks post-injection, much sooner than the recurrence of periorbital rhytides, but when the injection is placed too far inferior or deeply and the bulk of toxin is injected into the zygomaticus major the ill effects can last as long as 4 months.
Alam M, Barrett KC, Hodapp RM, et al. Botulinum toxin and the facial feedback hypothesis: can looking better make you feel happier? Journal of the American Academy of Dermatology. 2008;58(6):1061–1072.
Ascher B, Rzany BJ, Grover R. Efficacy and safety of botulinum toxin A in the treatment of lateral crow’s feet: double-blind, placebo-controlled, dose-ranging study. Dermatologic Surgery. 2009;35(10):1478–1486.
Kane MA. Classification of crow’s feet patterns among Caucasian women: the key to individualizing treatment. Plastic and Reconstructive Surgery. 2003;112:S33–S39.
Lowe NJ, Ascher B, Heckmann M, et al. Double-blind, randomized, placebo-controlled, dose-response study of the safety and efficacy of botulinum toxin type A in subjects with crow’s feet. Dermatologic Surgery. 2005;31(3):257–262.
Lowe NJ, Lask G, Yamauchi P, et al. Bilateral, double-blind, randomized comparison of 3 doses of botulinum toxin type A and placebo in patients with crow’s feet. Journal of the American Academy of Dermatology. 2002;47(6):834–840.
Matarasso SL, Matarasso A. Treatment guidelines for botulinum toxin type A for the periocular region and a report on partial upper lip ptosis following injections to the lateral canthal rhytids. Plastic and Reconstructive Surgery. 2001;1:208–214.
Prager W, Wissmuller E, Kollhorst B. Comparison of two botulinum toxin type A preparations for treating crow’s feet: a split-face, double-blind, proof-of-concept study. Dermatologic Surgery. 2010;36:2155–2160.
Yamauchi PS, Lask G, Lowe NJ. Botulinum toxin type A gives adjunctive benefit to periorbital laser resurfacing. Journal of Cosmetic and Laser Therapy. 2004;6(3):145–148.
Zimbler MS, Holds JB, Kokoska MS, et al. Effect of botulinum toxin pretreatment on laser resurfacing results: a prospective, randomized, blinded trial. Archives of Facial Plastic Surgery. 2001;3(3):165–169.