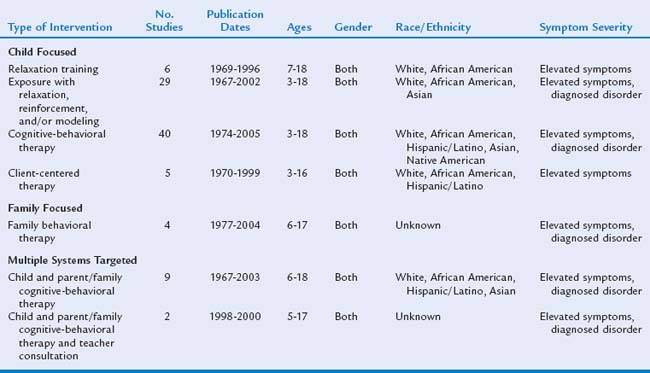
CHAPTER 8 Treatment and Management
8A. The Interdisciplinary Team Approach
In this chapter, we discuss the interdisciplinary team approach within health care and the field of developmental disabilities. We cover such topics as the history of interdisciplinary teams, including history in the field of developmental disabilities; the definition of a team; models of teamwork; factors that contribute to or present a challenge to interdisciplinary team collaboration; conceptual models used to evaluate interdisciplinary teams; and a review of the research on interdisciplinary teams. In referring to “disciplines,” we imply that the family is a discipline that has a specific body of knowledge to contribute as a member of the interdisciplinary team. Also, the term health care in the context of the interdisciplinary team approach does not mean solely medical care focusing on biological factors; it also includes behavioral factors, as well as physical and social environmental factors.1
HISTORY
Isolated models of interdisciplinary health care teams, as defined as professionals from two or more disciplines working together, have existed in the United States since the beginning of the 20th century. Complex social issues related to the effects of industrialization (e.g., poverty, overcrowded housing, child labor) began to come to attention in the early 1900s, and there was a recognition among some professionals that health care involved joining “medical care with social fact.”2 The first publication in the United States to introduce the concept of interdisciplinary care is attributed to Richard Cabot of Massachusetts General Hospital; in 1915, he wrote about the value of… teamwork of the doctor, educator and social worker in the clinical efficiency.”3
With World War I, and to a greater extent with World War II, rehabilitation teams emerged to address the needs of veterans. After World War II, there was a rapid expansion of knowledge in medicine, an increase in accompanying technology, and the emergence of new specialties.4 Simultaneously in the 1940s, a new body of knowledge known as group dynamics was emerging from the fields of social psychology, sociology, and anthropology.5 In the mid-1940s, knowledge from the fields of group dynamics, social psychology, and educational psychology were melded to develop the unstructured Training Group (T-Group) as an intensive learning experience in small-group behavior.6
In the early1960s, issues related to poverty became a major national focus, and the concept of “comprehensive care” provided by interdisciplinary teams evolved as a means of addressing both social and medical needs of the individual.4 Demonstration team-managed neighborhood health centers were established in underserved areas to provide comprehensive care, which included medical, social, and vocational services. These types of clinics rapidly expanded during the 1970s to more than 850 by 1980.7 At the same time, knowledge in the field of group dynamics/theory was expanding to such areas as the integration of personal learning and planned action for social improvement, phases of group development, communication in groups, and conditions that encourage group participation.5
In the equal rights climate of the 1960s, there emerged a professional interdisciplinary movement that embraced the team concept as an approach to improve health care delivery. The team concept was also viewed by some professionals as a means of achieving a greater equality in status of certain disciplines, which in turn would lead to improved health care delivery.4,8 For example, in 1971, Madeleine Leininger9 stated the following in an article about interdisciplinary education:… in our future conceptualizations of health education and service models, there is a need to consider ways to reduce and redistribute physician power so that other health disciplines and consumers can share in his power, decision-making, and the control of health matters and resources” (p 789).
The 1970s marked the integration of group theory principles into examining interdisciplinary health care teams.9–12 Also, aging of the population became of concern, and interdisciplinary teams began to increase within the field of geriatrics. During this period, the Department of Veterans Affairs implemented the Interdisciplinary Team Training in Geriatrics program, a clinically based educational program for both staff and students. The program eventually expanded beyond geriatrics and became the Interprofessional Team Training and Development Program.13 In the 1980s, the Bureau of Health Professions also began awarding Geriatric Education Center and Rural Health initiative grants to universities to teach collaborative teamwork practices to professionals in medical and health-related fields for working in the area of geriatrics and to students working in rural areas.
The 1990s were a time of changes in the health care environment, with increased reliance on primary care, disease prevention, evidence-based practice, and cost containment. Health care organizations incorporated organizational and management theory into their operations and adopted concepts of total quality management, total quality improvement, and continuous quality improvement.14 “Team” became a buzz word, and self-directed work groups emerged to address issues related to reducing costs and increasing productivity. In 1995, the Pew Health Professions Commission issued Critical Challenges: Revitalizing the Health Professions for the Twenty-First Century.15 This report presented a comprehensive analysis of the trends and strategies for successful outcomes in health care. One of the Commission’s recommendations for the future was team training and cross-professional education for all health professionals. In relation to this recommendation, the Commission expressed concern that model experiments involving team training and cross-professional education had stopped; the Commission urged that they be “rekindled” through “more sharing of clinical resources, more cross-teaching by professional faculties, more exploration of the various roles played by professionals and the active modeling of effective team integration in the delivery of efficient, high quality care” (p 22).
The beginning of the 21st century is an era in which teamwork is becoming a norm within health care organizations. With the Institute of Medicine’s 1999 report, To Err is Human: Building a Safer Health System,16 teamwork became to be viewed as crucial for ensuring patient safety, and a variety of medical team training programs began to emerge.17 After publication of the report, the Agency for Healthcare Research and Quality commissioned an evidence-based literature review regarding safety improvement, which included a review of Crew Resource Management (CRM) and its application to medicine.18 CRM, an approach to safety training focusing on effective team management, was developed by experts in aviation to improve the operation of flight crews and was beginning to be applied to high-stress decision-making health care environments such as the operating room, the labor and delivery suite, and the emergency room. Although additional evidence-base studies were indicated, it was concluded that CRM had tremendous potential applications in the health care field.18 By 2005, a variety of CRM-based medical training programs had been developed with the goal of reducing the number of medical errors through the application of teamwork skills training. A formal review of six of these medical training programs was commissioned by the Agency for Healthcare Research and Quality as part of a report on what federally funded programs had accomplished in understanding medical errors and implementing programs to improve patient safety over the 5 years since To Err is Human was published.17 Among the recommendations that resulted from the review was the recommendation that “the health care community develop a standard set of generic teamwork-related knowledge, skill and attitude competencies” (p 263).
As the team concept was gaining momentum in the actual delivery of health care, it was also gaining momentum in relation to the educational preparation of health care professionals. The 2001 Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century19 expressed concern that although health professionals were asked to work in interdisciplinary teams, they did not receive education together or receive training to develop team skills. A recommendation of Crossing the Quality Chasm was that a multidisciplinary summit of leaders within the health professions be held to identify strategies for restructuring educational programs. The summit was convened in 2002, and recommendations were issued in the 2003 report Health Professions Education: A Bridge to Quality.20 Resulting was an overarching vision for clinical education in the health professions: “All health professions should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics”(p 3). To achieve this vision, five core competencies for the areas identified were proposed as competencies that all clinical health professions should possess. The challenge ahead will be for the traditionally autonomous health professions to agree that these core competencies should indeed become part of the curricula for all clinical health professions.
HISTORY WITH REGARD TO CHILDREN WITH DEVELOPMENTAL DISABILITIES
The Children’s Bureau, established in 1912, was the first government agency to focus on providing services to all children, including children with mental retardation and disabilities. In 1954, the Children’s Bureau awarded a project grant to the Children’s Hospital in Los Angeles to establish an interdisciplinary diagnostic clinic for children with mental retardation. By 1956, the Children’s Bureau had 36 demonstration projects to provide services to children with mental retardation, develop new methods of service delivery, and provide training for professional workers.21
With the 1960s, there emerged an emphasis on focusing not only on the treatment of a specific disability but also on the child who happened to have the disability and on his or her family.22 Inspired by personal experience, President John F. Kennedy created a President’s Panel on Mental Retardation in 1961 to advise him on how the federal government could best meet the needs of children with mental retardation and of their families. In 1962, the Panel issued a report that included recommendations for more comprehensive and improved clinical services, as well as efforts to overcome serious problems of personnel in the field.23 Legislation signed into law by President Kennedy in 1963 and funding provided by Amendments to Title V of the Social Security Act is administered by the Health Resources and Services Administration of the Public Health Service Department of Health and Human Service and legislates maternal and child health programs. In 1965 led to the development of University Affiliated Facilities (UAFs) in medical centers to provide both comprehensive interdisciplinary services to children with mental retardation and interdisciplinary training in the evaluation and management of children with mental retardation. This was considered a major breakthrough to systematically address personnel needs for children with mental retardation. It was the first time that the Congress and the Executive Branch recognized the need for federal funds to assist in establishing a national network of interdisciplinary training programs centered on models of service.24 However during this period, the interdisciplinary team approach to service and training did not go without criticism on a variety of grounds. Many of the critics believed that the expense of the interdisciplinary approach was not warranted; that there was an excessive duplication in the evaluation; and poor team dynamics resulted from conflicts among disciplines, personal frictions, defense of territory, or domination by one discipline or team member.25
Legislation in 1972 expanded the service and training roles of UAFs to include both children with mental retardation and those with other developmental disabilities. The number of UAFs continued to grow, and by the mid-1970s, there were about 40 in 30 states. In 1976, a UAF Long Range Planning Task Force was established to reassess the original UAF concept and make recommendations as to their future direction and role. Their reassessment indicated that, overall, the original UAF concept was sound and experience had proved that the program concept was effective in meeting a significant social need.24 On the basis of the review, the Task Force made a number of recommendations to modernize and extend the program to serve individuals, both children and adults, with developmental disabilities in all states. The Task Force also reaffirmed the importance of training, both pre-service and in-service, as a role of the UAFs and endorsed a definition of interdisciplinary training, which had been developed by UAF training directors:
The reader is referred to the UAF Long Range Planning Task Force report The Role of Higher Education in Mental Retardation and Developmental Disabilities.24 The values and concepts related to interdisciplinary training and service described are as important today as they were in 1976.
The funding for the programs came from two sources the Administration for Developmental Disabilities and the Maternal and Child Health Bureau. The Maternal and Child Health Bureau programs maintained a stronger child and health focus than did those funded by the Administration for Developmental Disabilities. These programs became the Leadership Education in NeuroDevelopment and Related Disabilities (LEND). The LEND programs were developed by the Maternal and Child Health Bureau to improve the health status of infants, children, and adolescents with or at risk for neurodevelopmental and related disabilities and the health status of their families. This is accomplished through the training of professionals for leadership roles in the provision of health and related care, continuing education, technical assistance, research, and consultation.
WHAT IS A TEAM?
There are multiple definitions of what a team is; many of the definitions are based on different theoretical frames of reference. One definition, based on organizational design theory, that is frequently cited is that a “team” is a small number of people with complementary skills who are committed to a common purpose, performance goals, and approach for which they hold themselves mutually accountable.26 The four elements of this definition are as follows:
Although the term team is often used interchangeably with workgroup, it is viewed as different in several ways. Katzenbach and Smith31 identified both collective performance and mutual responsibility as two major ways in which teams differ from workgroups. In their view, a workgroup’s performance is a function of what its members do as individuals, and responsibility for performance is solely at the individual level. Drinka40 distinguished between the two on the basis of three factors present in health care teams, but not workgroups, that can negatively affect group process: presence of autonomous disciplines who are used to doing things independently of other disciplines; the ongoing nature of health care teams rather than being time-limited, as workgroups are; and the continual entering and leaving of members as a result of high staff turnover.
MODELS OF TEAMWORK
The composition, organization, and functioning of health care teams varies widely among institutions, medical specialties, and type of services offered.41 Many teams include a number of loosely associated personnel or a smaller number of highly interdependent professionals. Multiple terms are used in an attempt to describe the different models of current health care teams, including unidisciplinary, intradisciplinary, cross-disciplinary, multidisciplinary, interdisciplinary, intraprofessional, and transdisciplinary. The most common terms, often used interchangeably, are multidisciplinary, interdisciplinary, and transdisicplinary. All three models are based on the recognition that no one discipline has the breadth of knowledge and skills that are necessary to provide quality health care.
Unidisciplinary
This term in the past has not been included as a model of teamwork, because it was traditionally used to refer to one professional working independently in his or her specialty. Historically, in terms of the interdisciplinary approach, it also implied a professional who perceived himself or herself as have the knowledge and skills needed to identify and address all areas related to his or her field of focus. The well-known fable of “The Blind Men and the Elephant” has often been used as a metaphor in describing unidisciplinary functioning. Just as each man who was blind determined what the elephant was like on the basis of the individual part the man touched, each discipline perceives the individual in a unique, valid way and yet risks remaining “blind” to the total individual. With the emergence of single-discipline group practices, the term is also used at times to refer to two of more professionals in a discipline who share the same professional skills and training, have a common language, and function in a group.42 As a result of increased specialization within medicine, unidisciplinary, or what sometimes is referred to as intradisciplinary, has been used to describe a team of professionals in a discipline who have additional professional skills and training in varying specialty areas and, although they share some common language, have developed a language specific to their specialty. An example of a unidisciplinary team would be a pediatric urologist, a pediatric neurologist, and a pediatric orthopedist who communicate with each other and share information in the provision of care to an individual child.
Multidisciplinary
Some authorities also equate the multidisciplinary team model with “The Blind Men and the Elephant” in that each discipline “feels” or focuses on its own area. The difference with the multidisciplinary team is that there is some form of communication about the information that was obtained that potentially contributes to decision making with regard to the “whole.” There is, as a result, less chance for one person’s mistakes or biases to determine the course of events.43 However, the model can result in simply piecing information together on the basis of the individual discipline results, especially if the model is implemented without the opportunity for interaction between team members at a team meeting.38
Interdisciplinary
One of the strengths of the interdisciplinary model is the integration of the individual contributions of team members to address a common set of issues or problems.37,45–47 Another strength is the collaborative decision making that occurs to establish a holistic plan of care or recommendations.37,45,47 Over time, the team members also develop a “common language” that facilitates communication and collaborative decision making.36,37 The interdisciplinary team model, however, also presents several challenges, which are discussed separately.
Transdisciplinary
The features most frequently identified in relationship to transdisciplinary teams are as follows:
Strengths of the transdisciplinary model include a high degree of interaction and coordination; increased agreement among team members about the acceptability of recommendations; enhanced opportunities for team members to learn from one another; decreased fragmentation of services; and increased continuity and consistency of services.43 Also, in the area of early intervention, limiting the number of people who come in contact with a very young child prevents duplication of services and unnecessary intrusion into family activities and routines.44 Although the high degree of interaction and coordination is a strength, it is also a potential challenge in that the required degree of role sharing and transfer may lead to role ambiguity, role conflict, and role release to the extent of loss of professional identity.43
Transdisciplinary has also been used to refer to teams of multiskilled health practitioners who are trained to provide a wide range of services in a specific field, such as geriatrics, apart from training in a traditional discipline.38 This approach to the provision of health care has also been referred to as a pandisciplinary model, in which a single new discipline’s role spans all areas of competence relevant to a specific field.42 Unfortunately, in many ways, the pandisciplinary model brings teamwork full circle back to an unidisciplinary approach in which practitioners from one discipline assume that they have all the knowledge and skills needed to provide services in a particular field.
Each model of teamwork described has its strengths and challenges. Some professionals advocate one model over, implying that the particular model is better than others. It is more constructive to think of the models as points along a continuum of approaches, all of which have the common goal of providing high-quality services to children with developmental disabilities and to their families. Different programs serving children with developmental disabilities and their families use different models along this continuum to reach the common goal. For a program that provides ongoing services to a large number of children with medically complex health needs that necessitate the involvement of multiple medical specialties, the multidisciplinary team model may be the only feasible model. However, in a program that provides diagnostic and treatment services for children of varying ages with a broad range of developmental disabilities, the interdisciplinary team approach may be the model by which services are provided for older children, and the transdiciplinary model, by which services are provided for very young children and their families.
In the interdisciplinary and transdisciplinary model, and frequently in the multidisciplinary model, decision making involves face-to-face interaction. A new type of team, the virtual team, is emerging in the health care field. Virtual teams have been used in business for some time and consist of geographically or organizationally dispersed members who use technologies to perform team tasks.48 Rather than communication during face-to-face meetings, communication and decision making are accomplished through such technologies as email or video teleconferencing. Within health care, with the increasing demands for productivity and changing reimbursement, traditional models of teamwork may no longer be as functional as they once were and may be replaced by virtual teams.49,50 According to a developing body of knowledge about virtual teams, virtual teams apparently go through the same stages of team development and confront the same interpersonal process issues that exist in teams that meet face to face.51,52
FACTORS THAT CONTRIBUTE TO INTERDISCIPLINARY TEAM COLLABORATION
As discussed under the definition of a team, three important factors are complementary skills (discipline skills, problem-solving and decision-making skills, and interpersonal skills), commitment to a common purpose, and mutual accountability. Closely related to these factors are the concepts of shared leadership roles and shared power.31,33,37,39 Shared leadership means that each team member, depending on the situation, assumes the role of either team leader or team member.53 Historically, interdisciplinary teams tended to have one member who was designated the team leader upon whom the onus was placed for the success or failure of the team. A large body of literature emerged addressing leadership roles and styles of successful and unsuccessful team leaders. Slowly the responsibility for success or failure of interdisciplinary teams in achieving their goals shifted also to team members, and literature focusing on the attributes and behaviors of effective team members began to emerge.38 As the concept of shared leadership evolved, the concept of shared power among team members, regardless of educational or professional preparation, also evolved.39 Power and status within the interdisciplinary team was historically accorded to the physician, who usually was also the team leader.9,37,54 However, other hierarchies also exist not only between other disciplines but also within disciplines, on the basis of educational preparation (e.g., doctoral, master’s, bachelor’s degrees).37,55 Shared power is viewed as a means to bestow each team member equal status within the interdisciplinary team. This concept is especially important if family members are truly to be members of the interdisciplinary team.
Among the additional factors that have been identified as contributing to interdisciplinary team collaboration are individual or personal attributes. Simply placing someone in a team will not make him or her an effective team member. The reality is that some people are egocentric and do not have the collective orientation to be team members.56 Some of the individual attributes identified as enhancing interdisciplinary team function are flexibility and adaptability31,34 and the abilities to view diverse perspectives as learning opportunities, to engage in critical thinking, and to synthesize information adaptability.57
Another factor that is frequently mentioned as contributing to interdisciplinary team collaboration is the development of “common language” among the team members. Individual disciplines speak different languages that contain very discipline-specific terminology, jargon, and acronyms,37 which become even more difficult to understand the more specialized a discipline becomes.58 The process of developing a common language takes time and evolves from communication and learning that occurs as the team works together. It involves recognizing that, for disciplinary knowledge explicit and accessible to other disciplines, it must be translated into a language that other people will understand.36 However, members of other disciplines must be comfortable enough within the team to ask for clarification when they do not understand members of another discipline. Another problem of “common language” that often takes a longer time to surface occurs when two or more disciplines use a common term and thus think they are communicating, when in reality they are not because they define the term differently in subtle ways.
Just as members of different disciplines speak different languages, they differ in other ways. It has been suggested that viewing disciplines as culturally diverse groups will result in a better understanding of and respect for the diverse perspectives of the disciplines.57,59 Some of the ways in which disciplines, like cultures, may differ are in their theoretical orientation and assumptions (e.g., biomedical, behavioral, and biopsychosocial)37,60; their mode of thinking (e.g., divergent/inductive vs. convergent/deductive)55,61; and values (e.g., saving life vs. quality of life).60,61 Also involved is developing an understanding of such areas as the education, levels of practice, areas of expertise, and roles of the individual disciplines.37,42,62 By learning about one another, team members not only develop a better general understanding of one another but are able to identify the specific roles and responsibilities of individual team members, how they interface with each other, and where their disciplines overlap.42,60
FACTORS THAT PRESENT CHALLENGES FOR INTERDISCIPLINARY TEAM COLLABORATION
The organizational structures in which interdisciplinary teams operate are vital to their survival and significantly affect their performance.39,63–65 In an era in which teamwork is becoming a norm within health care organizations, there is concern that many health care organizations may not be ready or able to support interdisciplinary teams as the norm in service provision.35,66 The interdisciplinary approach requires an organizational structure that values the interdisciplinary team approach and is able to support the approach fiscally. Increased emphases on fee-generating services and productivity are already having affecting the provision of interdisciplinary team services in organizations in which this approach to service provision has been used, especially in which health care team services cannot also be covered by facility charges.67 The fee-for-service structure and current reimbursement policies are real barriers to the interdisciplinary team approach68 and are being questioned if the team model, although based on “best practices,” is financially viable.67 Settings in which the interdisciplinary approach is used to serve children with developmental disabilities and their families are facing the same emphases on fee-generating services and productivity as are other settings that provide services through the interdisciplinary approach. The issue of reimbursement for services has created the hierarchy of disciplines that can generate fees and disciplines that cannot; those that cannot are at risk of no longer being included in the provision of services to the degree they once were. Also, one of the advantages of the interdisciplinary team approach has been the team meetings, which provide team members the opportunity to learn from one another, share information, and participate in collaborative decision making and planning. Current payment policies, however, do not cover the time involved in team meetings.68 As a result, some settings that had been based on an interdisciplinary team model of services have had to retrench to the multidisciplinary model.
A second challenge to the interdisciplinary team collaboration is the current status of interdisciplinary education. Although interdisciplinary training has been promoted in areas such as developmental disabilities, geriatrics, rehabilitation, and primary care for underserved populations since the 1960s, it has never been widely incorporated into disciplinary training. Disciplinary education is viewed as a means of socializing a student to his or her future roles within the discipline. This role socialization has often been considered a major barrier to interdisciplinary teamwork because it is conducted in isolation from other disciplines.9,35,42,54,58,63 Not only is it conducted in isolation but also students are not necessarily rewarded for looking beyond their discipline for knowledge. Frequently, students are awarded grades on written assignments on the basis of their knowledge of disciplinary literature rather than their ability to integrate congruent or noncongruent knowledge from other disciplines into their assignment.
Ducanis and Golin63 identified three elements of interdisciplinary or team training: cognitive information, affective and experiential learning, and clinical competence. Within universities, there have been isolated models of interdisciplinary training that have especially addressed the areas of cognitive information and experiential learning, but for the most part they have not been widely incorporated.15,19 As with the implementation of the interdisciplinary team approach within health care organizations, interdisciplinary education requires a university structure that values the interdisciplinary education and is willing to support the approach fiscally.42,54 In addition, universities have been challenged with integrating additional emerging discipline-specific knowledge areas into already crowded curricula; when faced with this situation, faculty members are more likely to support discipline-specific knowledge than interdisciplinary knowledge.54
CONCEPTUAL MODELS USED TO EVALUATE INTERDISCIPLINARY TEAMS
Multiple conceptual models have been used to study and evaluate interdisciplinary teams. In some models, originating from group process theory, teams are viewed as evolving through various developmental stages. One of these models was developed by Drinka40 and identifies the stages as forming, “norming,” confronting, performing and leaving. Another model, developed by Lowe and Herranen,69 identifies the stages as becoming acquainted, trial and error, collective indecision, crisis, resolution, and team maintenance. One of the differences in the models is that the first model recognizes that team membership does not remain constant and, as team members leave and new team members enter, there is an effect on team performance. In additional models, teams are viewed in terms of group problem solving as an indicator of group effectiveness,62,70 the social climate of the groups,71 group interactions and relational norms,65 or role behavior and conflict.54
As organizational theory began to be applied to interdisciplinary teams, models were developed in which teams were also viewed in terms of processes in different areas. In one model, teams are viewed in terms of the areas of establishing trust, developing common beliefs and attitudes, empowering team members, having effectively managed team meetings, and providing feedback about team functioning.33 Other models integrate multiple theoretical perspectives into the model. For example, a model developed by Bronstein34 focuses on team processes in the areas of interdependence, newly created professional activities, flexibility, collective ownership of goals, and reflection on process. All these models focus on team process as indicators of team performance, with the assumption that an effectively functioning interdisciplinary team will provide quality services. However, it has been suggested that process measures really do not reflect team outcome and are important primarily for team training purposes when the intent is to identify performance issues and provide feedback to assist the individual in improving his or her behavior.35
REVIEW OF THE RESEARCH ON INTERDISCIPLINARY TEAMS
Several articles have included extensive reviews of the literature regarding interdisciplinary team care. The majority of these reviews concluded that there is little evidence of the effectiveness of interdisciplinary teams.45,53,60,68,72,73 These reviews of the literature also indicated the following:
Interestingly, the implementation of the interdisciplinary team approach on the basis of assumption is not unique in relation to the team approach. An example is the CRM approach to teamwork skills training, which serves as the basis for a variety of medical training programs focusing on reducing medical errors. The CRM has been used since 1980 to improve the operation of flight crews, despite the lack of definitive evidence that CRM decreases aviation errors.18 In addition, despite years of research regarding team performance in the military and corporate world, very little is known about the factors of that determine effective team performance.56
Schofield and Amodeo73 conducted an extensive review of the literature related to interdisciplinary teams in health care and human services settings. Not only did they conclude that there is limited evidence regarding the effectiveness of interdisciplinary teams, but the review also provided information regarding the fields from which the articles originated and the types of articles that have been written about interdisciplinary teams. From abstracts, Schofield and Amodeo identified 224 articles that potentially focused on the interdisciplinary approach to the provision of services. The majority of articles were in the fields of rehabilitation, geriatrics, health services, and mental health services; fewer than 25 articles were found in the field of developmental disabilities. After they eliminated articles that used the terms multidisciplinary or interdisciplinary without additional explanation, there were 138 potentially useful articles. Of theses articles:
Although concluding that there is little evidence regarding the effectiveness of interdisciplinary teams, the authors of these literature reviews acknowledged that research regarding interdisciplinary teams is complex and presents several challenges.68,72,74 For one thing, no two teams appear to be alike. The structure of interdisciplinary teams varies greatly between settings and, at times, within settings in terms of structure (e.g., composition of disciplines and number of team members).68 In addition, interdisciplinary teams function in clinical settings in which it is more difficult to use rigorous research designs.72 Third, the concept of the interdisciplinary team is to use the knowledge and skills of a number of disciplines to address a range of needs rather than an outcome in one area. As a result, the outcome of interdisciplinary team care becomes multidimensional and is more difficult to measure.72
Today there is an emphasis on cost containment, productivity, and evidence-based practice. If the interdisciplinary team approach is to survive this era, the approach based on assumption can no longer be justified. Research regarding the effectiveness of the interdisciplinary team approach needs to be better conceptualized, employ more sophisticated research designs when possible, and focus on both process and outcome.35,73 Studies must also clearly define what is meant when the terms multidisciplinary and interdisciplinary are used73 and must capture individual and team-level performance.35 Some of the specific challenging questions for future research include the following:68
1 U.S. Department of Health and Human Services. Healthy People 20010, 2nd ed. Washington, DC: U.S. Government Printing Office, 2000.
2 Brown TM. An historical view of health care teams. In: Agich GJ, editor. Responsibility in Health Care. Dordrecht, Holland: D. Reidel; 1982:3-21.
3 Cabot R. Social Service and the Art of Healing. New York: Moffat, Yard & Company, 1915.
4 Keith RA. The comprehensive treatment in rehabilitation. Arch Phys Med Rehabil. 1991;72:269-274.
5 Royer JA. Historical overview: Group dynamics and health care teams. In: Baldwin DC, Rowley BD, editors. Interdisciplinary Health Team Training. Lexington: University of Kentucky, Center for Interdisciplinary Education in Allied Health; 1982:12-28.
6 Benne KD, Bradford L, Gibb J, et al. The Laboratory Method of Changing and Learning. Palo Alto, CA: Science and Behavior Books, 1975.
7 Lefkowitz B. The health center story: Forty years of commitment. J Ambul Care Manage. 2005;28:295-303.
8 Purtilo RG. Interdisciplinary health care teams and health care reform. J Law Med Ethics. 1994;22:121-126.
9 Leininger M. This I believe … about interdisciplinary education for the future. Nurs Outlook. 1971;19:787-791.
10 Wise H, Beckard R, Rubin I, et al. Making Health Teams Work. Cambridge, MA: Ballinger, 1973.
11 Wise H, Rubin I, Beckard R. Making health teams work. Am J Dis Child. 1974;127:537-542.
12 Kane RA. The interprofessional team as a small group. Soc Work Health Care. 1975;1(1):19-31.
13 Reuben DB, Levy-Storms L, Yee MN, et al. Disciplinary split: A treat to geriatrics interdisciplinary team training. J Am Geriatr Soc. 2004;52:1000-1006.
14 Drinka TJK. Applying learning from self-directed work teams in business to curriculum development for interdisciplinary geriatric teams. Educ Geront. 1996;22:433-450.
15 Pew Health Professions Commission. Critical Challenges: Revitalizing the Health Professions for the Twenty-First Century. Berkeley, CA: University of California at Berkeley, Center for Health Professions, 1995.
16 Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press, 2000.
17 Baker DP, Gustafson S, Beaubien JM, et al. Medical team training programs in health care. In: Advances in Patient Safety: From Research to Implementation. Volume 4: Programs, Tools, and Products (AHRQ Publication No. 050021 [4]). Rockville, MD: Agency for Healthcare Research and Quality; 2005:253-267. pp. (Available at: http://www.ahrq.gov/qual/advances; accessed 10/23/06.)
18 Pizzi L, Goldfarb NI, Nash DB. Crew resource management and its application in medicine. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment: Number 43(AHRQ Publication No. 01-E058). Rockville, MD: Agency for Healthcare Research and Quality; 2001:501-509. (Available at: http://www.ahrq.gov/clinic/ptsafety; accessed 10/23/06, Chapter 44.)
19 Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press, 2001.
20 Institute of Medicine. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press, 2003.
21 Peppe KK, Sherman RG. Nursing in mental retardation: Historical perspective. In: Curry JB, Peppe KK, editors. Mental Retardation: Nursing Approaches to Care. St. Louis: CV Mosby; 1978:3-18.
22 Sheridan MD. The Handicapped Child and His Home. London: National Children’s Home, 1965.
23 The President’s Panel on Mental Retardation: A Proposed Program for National Action to Combat Mental Retardation. Washington, DC: Superintendent of Documents, 1962.
24 UAF Long Range Planning Task Force. The Role of Higher Education in Mental Retardation and Other Developmental Disabilities. Washington, DC: Department of Health, Education and Welfare, 1976.
25 Chamberlin HR. The interdisciplinary team: Contributions by allied medical and nonmedical disciplines. In: Gabel S, Erickson MT, editors. Child Development and Developmental Disabilities. Boston: Little, Brown; 1980:435-470.
26 Katzenbach JR, Smith DK. The Wisdom of Teams. Boston: Harvard Business School Press, 1993.
27 Cowell J, Michaelson J. Flawless teams. Executive Excellence. 2000;17(3):11.
28 Hrickiewicz M. What makes teams successful? Health Facil Manage. 2001;14(3):4.
29 Stahelski AJ, Tsukuda RA. Predictors of cooperation in health care teams. Small Group Res. 1990;21:220-233.
30 Poulton BC, West MA. The determinants of effectiveness in primary health care teams. J Interprof Care. 1999;13:7-18.
31 Katzenbach JR, Smith DK. The discipline of teams. Harv Bus Rev. 1993;71(2):111-120.
32 Sands RG, Stafford RG, McClelland M. “I beg to differ”: Conflict in the interdisciplinary team. Soc Work Health Care. 1990;14(3):55-72.
33 Dukewits P, Gowan L. Creating successful collaborative teams. J Staff Dev. 1996;17(4):12-16.
34 Bronstein LR. A model for interdisciplinary collaboration. Soc Work. 2003;48(3):113-116.
35 Baker DP, Salas E, King H, et al. The role of teamwork in the professional education of physicians: Current status and assessment recommendations. J Qual Patient Safety. 2005;31:185-202.
36 De Wachter M. Interdisciplinary teamwork. J Med Ethics. 1976;2:52-57.
37 Pearson PH. The interdisciplinary team process, or the professionals’ Tower of Babel. Dev Med Child Neurol. 1983;25:390-397.
38 Frattali CM. Professional Collaboration: A Team Approach to Health Care. Clinical Series No. 11. Rockville, MD: National Student Speech Language Hearing Association, 1993.
39 Orchard CA, Curran V, Kabene S. Creating a culture for interdisciplinary collaborative professional practice. Med Educ Online. 2005;10:11. (Available at: http://www.med-ed-online.org; accessed 10/24/06.)
40 Drinka TJ. Interdisciplinary geriatric teams: Approaches to conflict as indicators of potential to model teamwork. Educ Gerontol. 1994;20:87-103.
41 Ellingston LL. Communication, collaboration, and teamwork among health care professionals. Commun Res Trends. 2002;21(3):3-21.
42 Satin DG. A conceptual framework for working relationships among disciplines and the place of interdisciplinary education and practice: Clarifying muddy waters. Gerontol Geriatr Educ. 1994;14(3):3-24.
43 McCollum JA, Hughes M. Staffing patterns and team models in infancy programs. In: Jordan JB, editor. Early Childhood Education: Birth to Three. Reston, VA: Council for Exceptional Children; 1988:130-146.
44 Briggs MH. Team decision-making for early intervention. Infant Toddler Interv Transdiscip J. 1991;1(1):1-9.
45 Wiecha J, Pollard T. The interdisciplinary eHealth team: Chronic care for the future. J Med Internet Res. 2004;6(3):e22. (Available at: http://www.jmir.org/2004/e22/; accessed 10/24/06.)
46 Meeth LR. Interdisciplinary studies: A matter of definition. CHANGE. 1978;10(7):10.
47 Hall P, Weaver L. Interdisciplinary education and teamwork: A long and winding road. Med Educ. 2001;35:867-875.
48 Maruping LM, Agarwal R. Managing team interpersonal process through technology: A task-technology fit perspective. J Appl Psychol. 2004;89:975-990.
49 Cole KD. Organizational structure, team process, and future directions of interprofessional health care teams. Gerontol Geriatr Educ. 2003;24(2):35-49.
50 Rothschild SK, Lapidos S. Virtual integrated practice: Integrating teams and technology to manage chronic disease in primary care. J Med Syst. 2003;27(1):85-93.
51 Vroman K, Kovacich J. Computer-mediated interdisciplinary teams: Theory and reality. J Interprof Care. 2002;16:159-170.
52 Furst S, Reeves M, Rosen B, et al. Managing the life of virtual teams. Acad Manage Exec. 2004;18(2):6-20.
53 McCallin A. Interdisciplinary team leadership: A revisionist approach for an old problem? J Nurs Manage. 2003;11:364-370.
54 Aaronson WE. Interdisciplinary health team role taking as a function of health professional education. Gerontol Geriatr Educ. 1991;12(1):97-110.
55 Drinka TJK. From double jeopardy to double indemnity: Subtleties of teaching interdisciplinary geriatrics. Educ Gerontol. 2002;28:433-449.
56 Driskell JE. Collective behavior and team performance. Hum Factors. 1992;34:277-288.
57 Vincenti VB. Family and consumer sciences university faculty perceptions of interdisciplinary work. Fam Consum Sci Res J. 2005;34(1):81-104.
58 Garner HG. Challenges and opportunities of teamwork. In: Orelove FP, Garner HG, editors. Teamwork: Parents and Professionals Speak for Themselves. Washington, DC: Child Welfare League of America; 1998:11-29.
59 Clark P. Values in health care professional socialization: Implications for geriatric education in interdisciplinary teamwork. Gerontologist. 1997;37:441-451.
60 Simpson G, Rabin D, Schmitt M, et al. Interprofessional health care practice: Recommendations of the National Academies of Practice expert panel on health care in the 21st century. Issues Interdiscip Care: Natl Acad Pract Forum. 2001;3(1):5-19.
61 Qualls SH, Czirr R. Geriatric health teams: Classifying models of professional and team functioning. Gerontologist. 1988;28:372-376.
62 Christensen C, Larson JR. Collaborative medical decision making. Med Decis Mak. 1993;13(4):339-346.
63 Ducanis AJ, Golin AK. The Interdisciplinary Health Care Team: A Handbook. Germantown, MD: Aspen, 1979.
64 Butterill D, O’Hanlon J, Book H. When the system is the problem, don’t blame the patient: Problems inherent in the interdisciplinary inpatient team. Can J Psychiatry. 1992;37:168-172.
65 Amundson SJ. The impact of relational norms on the effectiveness of health and service teams. Health Care Manag (Frederick). 2005;24:216-224.
66 Cashman SB, Reidy P, Cody K, et al. Developing and measuring progress toward collaborative, integrated, interdisciplinary health care teams. J Interprof Care. 2004;18:183-196.
67 Melzer SM, Richards GE, Covington MW. Reimbursement and costs of pediatric ambulatory diabetes care by using the resource-based relative value scale: Is multidisciplinary care financially viable? Pediatr Diabetes. 2004;5:133-142.
68 Cooper BS, Fishman E. The Interdisciplinary Team in the Management of Chronic Conditions: Has Its Time Come? Baltimore: John Hopkins University, Partners for Solutions, 2003.
69 Lowe JI, Herranen M. Understanding teamwork: Another look at the concepts. Soc Work Health Care. 1981;7(2):1-11.
70 Whorley LW. Evaluating health care team performance: Assessment of joint problem-solving action. Health Care Superv. 1996;14(4):71-76.
71 Brock D, Barker C. Group environment and group interaction in psychiatric assessment meetings. Int J Soc Psychiatry. 1990;36:111-120.
72 Schmitt MH, Farrell MP, Heinemann GD. Conceptual and methodological problems in studying the effects of interdisciplinary geriatric teams. Gerontologist. 1988;28:753-764.
73 Schofield RF, Amodeo M. Interdisciplinary teams in health care and human service settings: Are they effective? Health Soc Work. 1999;24:210-219.
74 Opie A. Thinking teams thinking clients: Issues of discourse and representation in the work of health care teams. Sociol Health Illness. 1997;19:259-280.
8B. Family-Centered Care and the Medical Home
Societal changes have affected the relationship between families, children, and pediatricians.1,2 Technological advances, the growing prevalence of chronic disease in children, increasing empowerment of patients as consumers, and public access to information once available only through professionals, as well as the decreasing frequency of longitudinal patient-physician relationships, have affected the capability of the existing health care system to meet the needs of children and their families. If primary authority for clinical decision making in behalf of children is delegated to the pediatrician on the basis of professional expertise, there is a risk of minimizing the family’s lived experience; therefore, from many perspectives, traditional roles are no longer preferred. Instead, many families and pediatricians desire a relationship in which the contributions of each is valued. These role changes, along with acknowledgement that the health care system is failing to produce desired outcomes despite dramatically spiraling costs, urge redesign.3 Efforts to improve the quality of health care have focused on transforming biomedically dominated care processes to those guided by patients’ and families’ unique needs and values. In this chapter, we address relationship-focused quality improvement strategies by exploring the concept of family-centered care, examining selected evidence linking family-centered care to outcomes for children and families, discussing how family-centered care is applied in the medical home model within pediatric primary health care settings, and suggesting future directions in family-centered care practices and research.
HISTORICAL FOUNDATIONS OF THE FAMILY-CENTERED CARE CONCEPT
Family-centered care is one of several terms referring to a patient-centric view of the patient-physician relationship, and this concept is a relatively recent social movement. Although the concept began gaining momentum largely through the advocacy led by parents of children with special health care needs (CSHCN) in the 1980s, aspects of its underlying principles can be found in philosophical writings on the patient-physician relationship from ancient through contemporary times.3–5 Through the years, the concept has been discussed under the guise of different labels, including client-centered therapy,6 patient-centered care,4,7 and relationship-centered care.8 The common theme is that successful caregiving requires not only accurately diagnosing disease but also valuing the importance of human interactions in health care experiences and the legitimacy of the patient’s beliefs and preferences. Patient centeredness is frequently described by contrasting it to physician or system centeredness; the difficulty in attaining the required paradigm shift is highlighted by comparison to the inversion of thinking necessary to view the sun rather than the earth as the center of the universe.9 In a system-centered model, care processes are structured to facilitate the function of health care professionals to serve patients; patients must adapt to the constraints of the system. When a patient-centered model is used, the opposite is true: The system accommodates the individual. In pediatrics, patient-centered care is typically referred to as family-centered care to acknowledge that children’s well-being is inextricably linked to that of their families. A family-centered approach requires recognition that families have the most expertise about their child and, therefore, that they have the right and the responsibility to collaborate in medical decision making in behalf of their child.9,10 The following sections highlight some of the historical forces that have shaped the concept of family-centered care, including policy changes affecting family presence during hospitalizations, epidemiological changes in children’s health, broadening views of health determinants, and growing numbers of families raising CSHCN. Theoretical benefits of family-centered care, as well as empirical evidence regarding the efficacy of its use, are examined later in the chapter.
Changes in Hospital Policies Affecting Families Rights and Responsibilities
Even until the late 1950s, most medical professionals believed that visits from parents to their hospitalized children would inhibit effective care. Observations that children cried more in the presence of a parent or became distressed when their parent left led physicians and nurses to interpret parental visits as harmful for children.11 As a result, parents were regularly excluded from partnership in medical decision making about their children. By the 1970s, because of accumulating evidence that episodes of separation from their parents had the potential to harm children’s psychological well-being,12–14 U.S. hospital policies began allowing parents to stay with their children during admissions.15 Newborns began rooming in with their mothers instead of group nurseries, and fathers were permitted in the delivery room to support mothers during labor.16 The restrictive hospital policies before the 1970s that curtailed the family’s ability to comfort a hospitalized child (or other family member) provide an example of strategies that maintained institutional and staff control and exemplify system-centered models of health care delivery.
Epidemiological Changes in Children’s Health and Broadening Views of Health Determinants
In the 1970s, health services researchers brought attention to the growing prevalence of children’s psychosocial difficulties. Haggerty and colleagues called this growing challenge “the new morbidity” in their 1975 publication, Child Health and the Community,17 and conceptualized the interdependence of the family, the community, and children’s health. The authors asserted that for pediatricians to remain relevant to the well-being of children, pediatric training and practice would have to shift from focusing solely on the individual child to examining broader contextual aspects, including the family. The shift in thinking that Haggerty and colleagues’ work prompted, together with the rising tide of consumerism, undoubtedly fostered child health professionals to begin exploring the value of encouraging parents to be partners in medical decision making.
Further support for the importance of the family to children’s health came in 1977 in Engel’s classic article presenting the biopsychosocial medical model.18 His argument for a new paradigm of medical thinking that moved beyond a solely biomedical view to one that incorporated the inseparability of social and psychological influences on human health lent further support to Haggerty and colleagues’ argument that pediatricians needed to shift their focus beyond the child to the family context in order to foster children’s health.
Children with Special Health Care Needs and Their Families
Increasing recognition of the growing proportion of CSHCN and the ability of the U.S. health care system to successfully meet their needs spurred public organizers and government policy makers to improve the lives of these children and their families. In the U.S., key agencies that pioneered the CSHCN and family-centered care movement included the Maternal and Child Health Bureau (MCHB), the Association for the Care of Children’s Health (ACCH), Association of University Centers of Excellence in Disabilities, and the American Academy of Pediatrics (AAP). As a division of the Health Resources and Services Administration of the U.S. federal government’s Department of Health and Human Services, MCHB has long been charged with improving all children’s, women’s, and families’ health and is the designated organization that allocates funds from the federal Social Security Title V Act. ACCH, a now-defunct public organization originally formed in the 1960s, advocated along with MCHB for children’s health care system improvements. In the 1980s and 1990s, both organizations, along with the AAP and Association of University Centers of Excellence in Disabilities, were instrumental in broadening the conceptualization of children’s chronic disabling health conditions beyond one divided into specific disease categories to a more general category labeled children with special health care needs, defined as:
Those children who have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health care-related services of a type or amount beyond that required by children generally.19
Former Surgeon General C. Everett Koop’s 1987 Conference on Children with Special Health Care Needs disseminated the first widely acknowledged definition of family-centered care in the United States.20 This definition, formulated before the conference by parents, professionals, and policy makers active in the ACCH and MCHB, was published as a monograph, “Family-centered Care for Children with Special Health Care Needs,” that came to be commonly known as “Big Red” because of the red color of the cover.21 The ACCH made further refinements of the “Big Red” definition in 1994,9 which resulted in the key principles of family-centered care listed in Table 8B-1.22 Although the ACCH eventually disbanded, the Institute for Family-Centered Care, established in 1992, assumed the role that ACCH played and continues to disseminate information to promote the practice of family-centered care through annual conferences, information publications, guidelines for hospitals, and consultations to individual health organizations.23 MCHB also continues to include family-centered care into its improvement mandates for CSHCN:
From Shelton TL, Stepanek JS: The key elements of family-centered care. In Family-Centered Care for Children Needing Specialized Health and Developmental Services, 3rd ed. Bethesda, MD: Association for the Care of Children’s Health, 1994, p vii.
The overall national agenda is to provide and promote family-centered, community-based, coordinated care for CSHCN and to facilitate the development of community-based systems of services for such children and their families.24
The concept of family-centered care has undergone further refinements by researchers interested in early intervention services for CSHCN. Dunst and colleagues found that early intervention professionals and programs employing an empowering or enabling helpgiving relationship model more effectively achieve desirable child and family outcomes. The work of Dunst and colleagues has focused on outcomes, including family self-determination, decision-making capability, control, and self-efficacy and has precipitated a deeper understanding of the family-centered concept.25 They have extended the notion of family-centered care from one of simply incorporating parents in the delivery of health care to their children to the broader ideals of family-empowerment and marshalling community supports that are individualized by child and family need instead of imposing help from menu-driven service systems. Family empowerment has been explained as follows: “Family empowerment refers to families acquiring the capacity to exercise power. It makes them not just into actors, but into agents capable of shaping the conditions in which they live as they would want to shape them.”26 Dunst and colleagues proposed employing a conceptual framework of helpgiving relationships that empowers families by promoting family competency to identify and manage their child’s needs. Their model of empowerment requires specific conditions for both families and professionals. They require that families have (1) an increased understanding of their child’s needs, (2) the ability to deploy competencies to meet those needs, and (3) self-efficacy (a belief that they are capable) to do so.27 Among the conditions for help givers in their model are that professionals (1) have a proactive stance (help givers believe help seekers are already competent or have the capacity to become competent), (2) create opportunities for competence to be displayed (help givers provide enabling experiences to help seekers), and (3) allow help seekers to use their competencies to access resources and attribute success to their own actions, not the professional’s. In essence, Dunst and colleagues suggested that viewing the relationship from a strengths-based perspective rather than a deficit one is a more effective way to achieve desired outcomes for CSHCN and their families.
The multidisciplinary research group at McMaster University in Ontario, Canada also has done extensive work on refining the concept of family-centered care as it relates to CSHCN (note that they use the word service in place of the word care). In a summary of the theoretic and research literature,28 Rosenbaum attempted to organize the sometimes disparate meanings of family-centered service by dividing the concept into a three-level framework consisting of (1) basic premises or assumptions, (2) guiding principles, and (3) elements or key service provider behaviors. The basic premises are beliefs, values, and ideals about families and together form the backbone of the concept of family-centered service. Each premise has several guiding principles directed to professionals to help them ground their interactions with families. The elements are specific provider behaviors that follow from the assumptions and guiding principles. The addition of the key elements was an attempt to approach a definition that included measurable behaviors. Their conceptualization is summarized in Table 8B-2.
TABLE 8B-2 Premises, Principles, and Elements of Family-Centered Service
| Premises (Basic Assumptions) | ||
| Parents know their children best and want the best for their children. | Families are different and unique. | Optimal child functioning occurs within a supportive family and community context. The child is affected by the stress and coping family members. |
| Guiding Principles (“Should” Statements) | ||
| Each family member should have the opportunity to decide the level of involvement theywish in decision-making for their child. | Each family and family member should be treated with respect (as individuals). | The needs of all family members should be considered. |
| Parents should have the ultimate responsibility for the care of their children. | The involvement of all family members should be supported and encouraged. | |
| Elements (Key Service Provider Behaviors) | ||
| Service Provider Behaviors | Service Provider Behaviors | Service Provider Behaviors |
|---|---|---|
| To encourage parent decision-making | To respect families | To consider psychosocial needs of all members |
| To assist in identifying strengths | To support families | To encourage participation by all members |
| To provide information | To listen | To respect coping styles |
| To assist in identifying needs | To provide individualized service | To encourage use of community supports |
| To collaborate with parents | To accept diversity | To build on strengths |
| To provide accessible services | To believe and trust parents | |
| To share information about the child | To communicate clearly |
Adapted from Rosenbaum P: Family-Centered Service. Phys Occup Ther Pediatr 18(1):1-20, 1998.
SELECTED RESEARCH EVIDENCE REGARDING FAMILY-CENTERED CARE
Summary of Evidence
Our discussion to this point has focused on the development of the concept of family-centered care. Now we turn to an examination of the empirical evidence regarding this process of care. At first glance, in view of the convincing arguments of the many stakeholders interested in disseminating family-centered care improvements throughout the health care system, the reader might conclude that shifting existing care processes to those that are more family-centered is the most desirable method to successfully support families as they adapt to raising a child with special health care needs. However, before widespread dissemination of any improvement strategy, it is desirable to explore the intervention for the possibility of lack of desired benefit or even potential to harm.29 In addition, understanding how organizational structure affects patient outcomes is important but suffers from a lack of available methods of studying this aspect of care.30 Furthermore, despite the existing literature on family-centered and patient-centered care, commentaries and qualitative studies continue to point out that parents and professionals have limited or conflicting ideas about the meaning and scope of these concepts.31–34
Before discussing the research regarding family-centered care interventions and outcomes, an example involving the “Mr. Yuk” sticker in the childhood poisoning prevention campaign illustrates the importance of empirical evaluation of interventions. “Mr. Yuk,” created by the Pittsburgh Poison Center at the Children’s Hospital of Pittsburgh in 1971, was based on a logical assumption that applying these bright green stickers with a scowling face to bottles of medicines and other potentially toxic substances would help discourage children from ingesting the contents. Distributing these stickers to parents of young children became routine practice in most ambulatory child health care settings after clinicians incorporated the expert recommendation to do so. However, at least two studies35,36 done in the 1980s long after the intervention was entrenched suggested that “Mr. Yuk” stickers do not effectively keep toddlers away from potential poisons and may even attract children to them. One of the studies did note, however, that the stickers might work for older children or as part of a larger poisoning prevention campaign, highlighting the importance of tailoring interventions.36
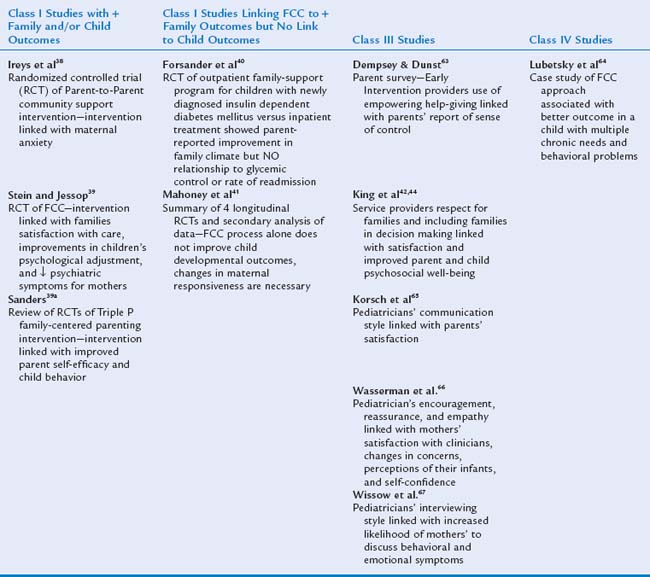
Research linking family-centered care to desired outcomes is available but challenging to summarize as a whole because of the heterogeneity of the definitions of the concept, study populations, focus of investigation, and methodological quality across studies. Furthermore, a complete review of the existing literature on family-centered care is beyond the scope of this chapter. With these limitations in mind, we have chosen to explore several articles linking family-centered care and outcomes and summarized several other articles according to quality of study methodology in Table 8B-3. Evidence is listed alphabetically by author’s names in columns based on the commonly used categorization scheme that organizes studies according to strength of the methodological quality.37 Class I evidence is considered the strongest for drawing valid conclusions between interventions and outcomes and results from randomized controlled trials. Class II evidence is second most powerful and includes nonrandomized trials, before-and-after evaluations, and studies in which participants serve as their own controls. Class III evidence refers to cross-sectional and case-control designs. Class IV evidence, derived from the weakest study designs, pertains to descriptive studies, case reports, and expert opinion. Note that classes III and IV evidence hold value in that they provide starting points for further study and suggested practices in the absence of higher classes of data.
Selected Class I Evidence Regarding Family-Centered Care and Outcomes
Randomized controlled trials of components of family-centered care summarized in the two left columns of Table 8B-3 are described in further detail. Ireys and colleagues evaluated the effect of referral to parent-to-parent support for mothers caring for children with chronic illness and found that mothers in the intervention group had lower anxiety levels, as measured by the Beck Depression Inventory and the Psychiatric Symptom Index.38 Stein and Jessop showed that in a longitudinal family-centered support program for families of CSHCN (the Pediatric Ambulatory Care Treatment Study), the group receiving intervention showed greater satisfaction with care, improvements in children’s psychological adjustment, and fewer psychiatric symptoms for mothers.39 In Australia, Sanders demonstrated in multiple studies the effectiveness of a family-centered parenting intervention, the Positive Parenting Program (Triple-P) for problematic child behaviors.39a Another study done in Sweden with children with newly diagnosed insulin-dependent diabetes mellitus showed associations between outpatient family-centered care processes and parent-reported improvement in family climate but failed to show a relationship to children’s glycemic control or rate of readmission.40 The last report mentioned in the randomized controlled trials in Table 8B-3 is a summary of class I studies that failed to show a simple link between care processes and child outcomes.41 Instead, the authors argued that only if interventions addressed maternal responsiveness were they successful in improving children’s developmental outcomes.
Using the three-level framework conceptualization of family-centered care noted in Table 8B-2, researchers in the Ontario group documented an association between family-centered care for CSHCN and their families in Canadian children’s rehabilitation centers and outcomes such as parent satisfaction with services,42,43 as well as improved parent and child psychosocial well-being.44 In these and other studies listed in Table 8B-3 in the two right columns, the investigators used methods that make it difficult to draw firm conclusions between family-centered care and outcomes. Furthermore, criticisms of using satisfaction and psychosocial well-being as outcomes are derived from the bias presumed inherent in subjective data and the observation that the measurement of traits is more psychometrically reliable than the measurement of states (i.e., satisfaction). In a summary of selected evidence, Rosenbaum found five randomized controlled trials evaluating family-centered care and provided a summary of other pertinent publications, most of who authors had used methods in the class II to class IV categories.28 Shields and associates published a Cochrane Colloquium review protocol for meta-analysis of family-centered care for hospitalized children in 2003 (updated in 2004) but have not begun collecting studies based on the protocol.45 We were not able to find any other publications of controlled trials or meta-analyses pertaining to family-centered care, despite an extensive search.
Other Selected Evidence Regarding Receipt of Family-Centered Care and CSHCN
MCHB, in collaboration with the National Center for Health Statistics of the Centers for Disease Control and Prevention, surveyed a nationally representative sample of more than 100,000 households across the country to measure the health and well-being of U.S. children.46,47 The National Survey of Children’s Health (NSCH), administered to families by telephone, included more than 38,000 families across the United States that had at least one child with special health care need and included questions to measure the six core outcomes listed in Table 8B-4. To assess the progress in achieving their national agenda for CSHCN, the survey included questions regarding families’ perceptions that their care was family-centered. Prevalence estimates from this study showed that 12.8% of children (9.3 million) younger than 18 years need a special health care issue to be addressed. Approximately one third of the families surveyed indicated that they were dissatisfied by the lack of critical elements of family centeredness. Questions regarding family centeredness emphasized the extent to which care provided by the child’s physicians and nurses focused on the family’s needs and not simply the child’s medical condition. Areas addressed included whether the professional (1) met information needs, (2) made the parent feel like a partner, (3) was sensitive to family values and culture, (4) spent enough time, and (5) listened to family concerns. One third of the families reported being usually or always dissatisfied with at least one family-centered aspect of their child’s care. Furthermore, families of such children living in poverty and from minority groups were more likely to be dissatisfied with these aspects of care. Although the data were based on self-report and collected cross-sectionally, which precluded causal conclusions, this study provides an important starting point from which to design more in-depth evaluations of family-centered aspects of the health care system and family health care provider interactions.
TABLE 8B-4 Maternal and Child Health Bureau Core Outcomes for CSHCN
|
All families of CHSCN will have adequate public and/or private health insurance to pay for the services they need.
|
CSHCN, children with special health care needs.
From McPherson M, Weissman G, Strickland BB, et al: Implementing community-based systems of services for children and youths with special health care needs: How well are we doing? Pediatrics 113:1538–1544, 2004.
THE MEDICAL HOME
History and Definition of the Medical Home Concept
The AAP has called for children to have a “medical home” since the 1960s.48 The original 1967 AAP definition referred to a single location of all medical information about a patient, especially children with chronic disease or disabling conditions.49 The idea evolved over the next 35 years to the current one, which emphasizes a concept broader than the notion of a single location. Now the medical home is conceptualized as a quality approach to providing cost-effective primary health care services in which families, health care providers, and related professionals work as partners to identify and access medical and nonmedical services to help children and their families achieve their maximum potential. In 2002, the AAP published a more definitive operational definition clarifying specific activities within each of seven medical home domains: accessible, family-centered, continuous, comprehensive, coordinated, compassionate, and culturally effective (see Appendix, Chapter 8B for a more complete description of the domains).50–52 Despite progress in clarifying the concept, significant challenges to establishing medical homes for all children remain; an important one is the lack of an adequate reimbursement structure for physicians’ services provided in a medical home. The next section describes a model that has been used to study the implementation of the medical home concept.
Efforts to Promote the Medical Home Concept
The MCHB funded the National Initiative for Children’s Healthcare Quality (NICHQ) to conduct multistate learning collaboratives to help disseminate the medical home concept throughout the United States.52 NICHQ staff and faculty, state Title V leaders, and private practices constituted two consecutive 15-month Medical Home Learning Collaboratives, the first occurring in 2003 to 2004 and the second in 2004 to 2005. The first collaborative included 30 practices in 12 states: Colorado, Connecticut, Florida, Louisiana, Michigan, New York, North Carolina, Ohio, Oklahoma, Utah, Virginia, and Wisconsin. The second consisted of nine states and multiple practices in the District of Columbia, Illinois, Maine, Maryland, Minnesota, Pennsylvania, Texas, Vermont, and West Virginia. The Learning Collaboratives studied the recommended best practices for making changes to enhance care for CSHCN. They employed NICHQ’s framework for improvement, which is based on a synthesis of models from the Institute for Healthcare Improvement’s Breakthrough Series Model,53 the Model for Improvement,54–56 and the Chronic Care Model.57 NICHQ’s model for improvement highlights the need for four key components of practice Microsystems: a clinical information system, effective decision support, a well-designed delivery system emphasizing planned care, and expert support for both family and developmentally appropriate child self-management. The model, schematically represented in Figure 8B-1, also highlights the key role of organizational leadership and the importance of linking health services and community resources.58 The second collaborative used process information regarding what did or did not work from the first learning experience and assessed resulting outcomes occurring as a result of incorporating medical home principles in primary care practices.
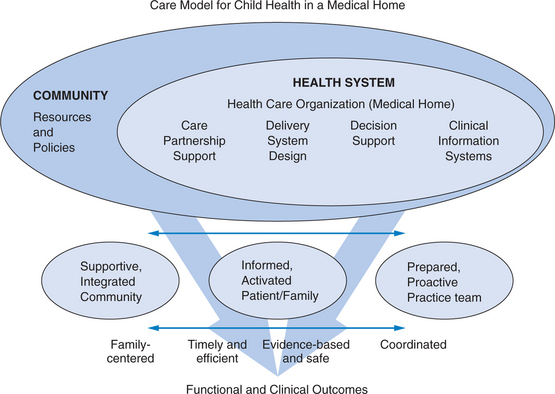
FIGURE 8B-1 The care model for child health in a medical home.58
(Adapted from Wagner’s Chronic Care Model in Wagner EH: Chronic disease management: What will it take to improve care for chronic illness? Effect Clin Prac 1:2-4, 1998. Reprinted with permission from National Initiative for Children’s Healthcare Quality.)
Select Evidence Regarding Elements of the Medical Home and Outcomes
Documented outcomes from the second NICHQ Medical Home Learning Collaborative included an increase in implementation of medical home concepts in the practices, an improvement in participation of parents in their children’s care, a decrease in unplanned hospitalization rates for CSHCN, a reduction in emergency department visits, decreases in numbers of missed school and work days, and an increase in capability of Title V organizations to implement, spread, and sustain medical home concepts within practices. A report on the implementation process and outcomes can be accessed at NICHQ’s Web site.58
A descriptive study with a screening tool to identify CSHCN59 in primary care settings revealed that the screener has the potential to identify a vulnerable group of children who need comprehensive and coordinated care. An example study of care coordination’s effect on outcomes demonstrated that care coordination was accepted by families and resulted in increased services, but the authors were not able to link the process of coordinating care with the outcomes.60
Practical Suggestions for Practitioners Wishing to Implement a Medical Home
NICHQ, the AAP National Center for Medical Home Initiatives for Children with Special Health Care Needs (http://www.medicalhomeinfo.org/), and the Center for Medical Home Improvement (http://www.medicalhomeimprovement.org/) have a wealth of information available for practitioners interested in implementing components of a medical home in their practice or who desire to advocate at a systems level for children with special health care needs. NICHQ has organized specific suggestions by area of focus, including community, health care organization, care partnership support, delivery system design, decision support, and clinical information systems, and these suggestions are listed in Table 8B-5. The AAP National Center for Medical Home Initiatives and Georgetown University collaborated on a report outlining specific methods for creating improvements in communication between primary care practitioners and subspecialists.61 The report contains practical suggestions and non-copyrighted form templates (a medical home-based care plan; an emergency information form for a child with special health care needs; a family-centered health care plan; a referral fax-back form; and examples of disease-specific forms, such as an action asthma plan) that practitioners can use to implement components of the medical home in their practices. In additiony, example templates for cataloguing resources and for tracking referral responses are included in Appendix, Chapter 8B.
TABLE 8B-5 Ideas for Improvement in Care for CSHCN Found on the NICHQ Web Site
| Community |
CSHCN, children with special health care needs; NICHQ, National Initiative for Children’s Healthcare Quality.
From Medical Home Initiatives for Children with Special Needs Project Advisory Committee: The medical home. Pediatrics 110:184-186, 2002.
Practitioners who have implemented quality improvements in their practices indicate that working with other practitioners who are similarly interested is a key to their success.62 They also typically identify individual practice staff members who will help outline the existing workflow and who will be responsible for delegated tasks (e.g., deciding who will distribute forms to families, where families will complete them—at home, in the office waiting room, in the physician office exam room, over the Web—and who will ensure that forms are replenished). Creating (and documenting) a standardized approach to information flow provides a way for all office staff to remain invested in the process and facilitates orientation for new employees.
Example of Use of the “Plan, Do, Study, Act” Method of Quality Improvement
Using the “plan, do, study, act” method of improvement that originated within the business field55,55a,56 allows practitioners to identify a specific problem area in need of improvement and create a new solution or process (“plan”), implement change on a small scale (“do”), measure the impact of implementing the change (“study”) and permanently implement the change with modifications as necessary identified in the measurement process (“act”). For example, a practitioner may recognize that he or she is not routinely receiving feedback after referring a child for consultation and decide that he or she wants to prioritize improving the referral communication process:
1 Leslie L, Rappo P, Abelson H, et al. Final report of the FOPE II Pediatric Generalists of the Future Workgroup. Pediatrics. 2000;106(suppl 5):1199-1223.
2 Starr P. The social transformation of American medicine. New York: Basic Books, 1982.
3 Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press, 2001.
4 Brown JB, Stewart M, Weston WW, et al. Introduction. In: Stewart M, Brown JB, Weston WW, et al, editors. Patient-Centered Medicine: Transforming the Clinical Method. 2nd ed. Oxford, UK: Radcliffe Medical Press; 2003:3-15.
5 McWhinney IR. The evolution of clinical method. In: Stewart M, Brown JB, Weston WW, editors. Patient-Centered Medicine: Transforming the Clinical Method. 2nd ed. Oxford, UK: Radcliffe Medical Press; 2003:17-30.
6 Rogers CR. Significant aspects of client-centered therapy. Am Psychol. 1946;1:415-422.
7 Gerteis M, Edgman-Levitan S, Daley J. Through the Patient’s Eyes. Understanding and Promoting Patient-Centered Care. San Francisco: Jossey-Bass, 1993.
8 Tresolini CP. The Pew-Fetzer Task Force: Health Professions Education and Relationship-Centered Care. San Francisco: Pew Health Professions Commission, 1994.
9 Shelton TL, Stepanek JS. Family-Centered Care for Children Needing Specialized Health and Developmental Services, 3rd ed., Bethesda, MD: Association for the Care of Children’s Health; 1994:1-120.
10 Hostler SL. Family centered care. Pediatr Clin North Am. 1991;38:1545-1560.
11 Johnson BH. The changing role of families in health care. Child Health Care. 1990;19:234-241.
12 Spitz RA. Hospitalism, an inquiry into the genesis of psychiatric conditions in early childhood. Psychoanal Study Child. 1945;1(53):74-82.
13 Bowlby J. Maternal care and mental health. Bull World Health Organ. 1951;3:355-533.
14 Klaus MH, Kennell JH. Maternal-Infant Bonding: The Impact of Early Separation or Loss on Family Development. St. Louis: CV Mosby, 1976.
15 Seagull EAW. The child’s rights as a medical patient. J Clin Child Psychol. 1978;7:202-205.
16 Tanner JL. Training for family-oriented pediatric care. Issues and options. Pediatr Clin North Am. 1995;42:193-207.
17 Haggerty RJ, Roghmann KJ, Pless IB. Child Health and the Community. New York: Wiley, 1975.
18 Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129-136.
19 McPherson M, Arango P, Fox H, et al. A new definition of children with special health care needs. Pediatrics. 1998;102:137-140.
20 Koop CE. Surgeon General’s Report: Children with Special Health Care Needs. Rockville, MD: U.S. Department of Health and Human Services, 1987.
21 Shelton T, Jepson E, Johnson BH. Family-centered care for children with special health care needs. Washington, DC: Association for the Care of Children’s Health, 1987.
22 Shelton TL, Stepanek JS. The key elements of family-centered care, 3rd ed. Bethesda, MD: Association for the Care of Children’s Health, 1994. Family-Centered Care for Children Needing Specialized Health and Developmental Services, p vii
23 The Institute for Family Centered Care: About Us. (Available at: http://www.familycenteredcare.org/about/index.html; accessed 10/24/06.)
24 Maternal and Child Health Bureau: Achieving and Measuring Success: A National Agenda for Children with Special Health Care Needs 2006. (Available at: http://www.mchb.hrsa.gov/programs/specialneeds/measuresuccess.htm; accessed 10/24/06.)
25 Dunst CJ, Trivette CM, Deal AG. Enabling and empowering families. In: Dunst CJ, Trivette CM, Deal AG, editors. Supporting and Strengthening Families: Methods, Strategies, and Practices. Cambridge, MA: Brookline Brooks, 1994.
26 Kordesh R. Irony and Hope in the Emerging Family Policies: A Case for Family Empowerment Associations. University Park, PA: Pennsylvania State University, Institute for Policy Research and Evaluation, 1995.
27 Dunst CJ, Trivette CM, Davis M, et al. Effective Help-Giving Practices. In: Dunst CJ, Trivette CM, Deal AG, editors. Supporting and Strengthening Families: Methods, Strategies, and Practices. Cambridge, MA: Brookline Books; 1994:171-186.
28 Rosenbaum P. Family-Centred Service. Phys Occup Ther Pediatr. 1998;18(1):1-20.
29 Donabedian A. The quality of care: How can it be assessed? JAMA. 1988;260:1743-1748.
30 Aiken LH, Sochalski J, Lake ET. Studying outcomes of organizational change in health services. Med Care. 1997;35(11 suppl):NS6-NS18.
31 Knafl K, Breitmayer B, Gallo A, et al. Parents’ view of health care providers: An exploration of the components of a positive working relationship. Child Health Care. 1992;21(2):90.
32 Gillespie R, Florin D, Gillam S. How is patient-centred care understood by the clinical, managerial and lay stakeholders responsible for promoting this agenda? Health Expect. 2004;7:142-148.
33 Blue-Banning M, Summers JA, Frankland HC, et al. Dimensions of family and professional partnerships: Constructive guidelines for collaboration. Except Child. 2004;70:167-184.
34 Loewy EH. In defense of paternalism. Theor Med Bioeth. 2005;26:445-468.
35 Fergusson DM, Horwood LJ, Beautrais AL, et al. A controlled field trial of a poisoning prevention method. Pediatrics. 1982;69:515-520.
36 Vernberg K, Culver-Dickinson P, Spyker DA. The deterrent effect of poison-warning stickers. Am J Dis Child. 1984;138:1018-1020.
37 McKibbon A, Hunt D, Richardson WS, et al. Introduction: The philosophy of evidence-based medicine. In: Guyatt G, Rennie D, editors. Users’ Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. Chicago: AMA Press; 2002:3-12.
38 Ireys HT, Chernoff R, DeVet KA, et al. Maternal outcomes of a randomized controlled trial of a community-based support program for families of children with chronic illnesses. Arch Pediatr Adolesc Med. 2001;155:771-777.
39 Stein RE, Jessop DJ. Does pediatric home care make a difference for children with chronic illness? Findings from the Pediatric Ambulatory Care Treatment Study. Pediatrics. 1984;73:845-853.
39a Sanders MR. Triple P-Positive Parenting Program: Towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev. 1999;2(2):71-90.
40 Forsander GA, Sundelin J, Persson B. Influence of the initial management regimen and family social situation on glycemic control and medical care in children with type I diabetes mellitus. Acta Paediatr. 2000;89:1462-1468.
41 Mahoney G, Boyce G, Fewell RR, et al. The relationship of parent-child interaction to the effectiveness of early intervention services. Top Early Child Spec Educ. 1998;18(1):5.
42 King G, Cathers T, King S, et al. Major Elements of parents’ satisfaction and dissatisfaction with pediatric rehabilitation services. Child Health Care. 2001;30:111-134.
43 Law M, Hanna S, King G, et al. Factors affecting family-centred service delivery for children with disabilities. Child Care Health Dev. 2003;29(5):357-366.
44 King G, King S, Rosenbaum P, et al. Family-centered caregiving and well-being of parents of children with disabilities: Linking process with outcome. J Pediatr Psychol. 1999;24:41-53.
45 Shields L, Pratt J, Flenady VJ, et al. Family-centred care for children in hospital [protocol]. Cochrane Database Syst Rev. (1):2006. CD1–21
46 van Dyck PC, Kogan M, McPherson MG, et al. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004;158:884-890.
47 McPherson M, Weissman G, Strickland BB, et al. Implementing community-based systems of services for children and youths with special health care needs: How well are we doing? Pediatrics. 2004;113:1538-1544.
48 Sia C, Tonniges TF, Osterhus E, et al. History of the medical home concept. Pediatrics. 2004;113:1473-1478.
49 American Academy of Pediatrics Council on Pediatric Practice. Pediatric Records and a “medical home.”. In: Standards of Child Care. Evanston, IL: American Academy of Pediatrics; 1967:77-79.
50 Committee on Children with Disabilities. Care Coordination: Integrating Health and Related Systems of Care for Children with Special Health Care Needs. Pediatrics. 1999;104:978-981.
51 Council on Children with Disabilities. Care coordination in the medical home: Integrating health and related systems of care for children with special health care needs. Pediatrics. 2005;116:1238-1244.
52 Medical Home Initiatives for Children with Special Needs Project Advisory Committee. The medical home. Pediatrics. 2002;110:184-186.
53 National Initiative for Children’s Healthcare Quality: NICHQ Medical Home Learning Collaborative. (Available at: http://www.nichq.org/NR/rdonlyres/83AFF39E-BF99-40B3-8803-442623776043/0/MHLC_2_Final_Report_Final.pdf; accessed on April 2, 2006.)
54 Institute for Healthcare Improvement: The Breakthrough Series: Institute for Healthcare Improvement’s Collaborative Model for Achieving Breakthrough Improvement. (Available from: http://www.ihi.org/NR/rdonlyres/BCA88D8F-35EE-4251-BB93-E2252619A06D/0/BreakthroughSeriesWhitePaper2003.pdf.; accessed 10/24/06.)
55 Institute for Healthcare Improvement: Improvement Methods. (Available at: http://www.ihi.org/IHI/Topics/Improvement/ImprovementMethods/HowToImprove/; accessed 10/24/06.)
55a Deming WE. The New Economics for Industry, Government, Education, 2nd ed. Cambridge, MA: MIT Press, 2000.
56 Langley GL, Nolan KM, Nolan TW, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco: Jossey-Bass, 1996.
57 Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Effect Clin Prac. 1998;1:2-4.
58 National Initiative for Children’s Healthcare Quality: NICHQ Medical Home Learning Collaborative. (Available at: http://www.nichq.org/NICHQ/Topics/Chronic Conditions/; accessed 10/24/06.)
59 Farmer JE, Marien WE, Frasier L. Quality improvements in primary care for children with special health care needs: Use of a brief screening measure. Child Health Care. 2003;32:273-285.
60 Smith K, Layne M, Garell D. The impact of care coordination on children with special health care needs. Child Health Care. 1994;23:251.
61 Antonelli R, Stille C, Freeman L: Enhancing Collaboration between Primary and Subspecialty Care Providers for Children and Youth with Special Health Care Needs. Washington, DC: Georgetown University Center for Child and Human Development. (Available at: http://gucchd.georgetown.edu/files/products_publications/PrimarySpecialityCollaboration.pdf; accessed 10/24/06.)
63 Dempsey I, Dunst CJ. Helpgiving styles and parent empowerment in families with a young child with a disability. J Intellect Dev Disabil. 2004;29:40-51.
64 Lubetsky MJ, Mueller L, Madden K, et al. Family-centered/interdisciplinary team approach to working with families of children who have mental retardation. Ment Retard. 1995;33:251-256.
65 Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication. 1. Doctor-patient interaction and patient satisfaction. Pediatrics. 1968;42:855-871.
66 Wasserman RC, Inui TS, Barriatua RD, et al. Pediatric clinicians’ support for parents makes a difference: an outcome-based analysis of clinician-parent interaction. Pediatrics. 1984;74:1047-1053.
67 Wissow LS, Roter DL, Wilson ME. Pediatrician interview style and mothers’ disclosure of psychosocial issues. Pediatrics. 1994;93:289-295.
68 Medical home helpful Web sites. Pediatrics. 2004;113(5):1548.
8C. Psychopharmacological Management of Disorders of Development and Behavior
Prescriptions of psychotropic medications have dramatically increased since the mid-1990s.1 This includes stimulants, antidepressants, and, more recently, mood stabilizers and atypical antipsychotic medications. Nonpsychiatric practitioners (pediatricians, family physicians) continue to prescribe the majority of psychotropic medications, often because of lack of available child psychiatry consultation.2 One concern about this practice is that the evidence base for the clinical usefulness of these medications has not kept pace with practice patterns. In addition, training for primary care clinicians in the management of psychiatric disorders is scant, in spite of the fact that they are often responsible for that management.3 This chapter focuses on general principles of psychotropic medication use, major categories of psychotropic medications, and their basic mechanisms of action. We review common indications and the evidence supporting that use. Finally, we describe the guidelines for medication use in general and in specific disorders, along with any controversies about their use.
GENERAL PRINCIPLES OF PSYCHOTROPIC MEDICATION USE IN CHILDREN AND ADOLESCENTS
Although it is essential to determine a diagnosis before medication is instituted, it is often the target symptoms that are responsive to medication. The symptoms should be of sufficient severity and interfere with the child’s or adolescent’s daily functioning within his or her family, peer group, and school. In addition, the clinician needs to be aware that certain target symptoms may originate from different causes, and the medication must address the underlying disorder. For example, treating the target symptom depression with antidepressant medications in a patient with bipolar disorder may exacerbate the depression, instead of reducing it.
Careful monitoring of the efficacy of medications for behavioral disorders requires systematic review of the target symptoms over time. This can include narrative observations from parents and teachers. The use of rating scales for the particular target symptom can be very helpful.67 Such rating scales can also be useful for monitoring side effects. Many such rating scales are proprietary and can be purchased; many are available online without charge.
Understanding the meaning of medications to the child and adolescent patients and their families is also important.4 The clinician should explore parents’ attitudes and expectations about medication before instituting a treatment. Children are often apprehensive about taking medications. This is often related to their developmental level of understanding. Adolescents may initially rebel against the idea of taking medications and also worry about the effects, both positive and negative, of medications.
MEDICATIONS FOR ATTENTION-DEFICIT/HYPERACTIVITY DISORDER
Stimulants
Stimulants remain the most commonly prescribed medication for behavioral disorders.5 Psychostimulants are thought to exert their influence on the catecholamine system by reuptake inhibition, enhanced release, or both.6 Amphetamines affect reuptake inhibition, enhanced release, and storage. Methylphenidate appears to work primarily through presynaptic reuptake inhibition of dopamine and norepinephrine.
The effectiveness of stimulants for the short-term treatment of ADHD is well documented.6 By 1996, 161 randomized controlled trials had been published, including 5 in preschool-aged patients, 150 in school-aged patients, 7 in adolescents, and 9 in adults (American Academy of Child and Adolescent Psychiatry practice parameters, 20026). The finding of improvement in the patients randomly assigned to receive stimulants was robust in comparison with the finding in patients assigned to receive placebo. Studies consistently noted a positive response for core ADHD symptoms, reduced aggression, and improved behavioral compliance. Methylphenidate is the best studied, but dextroamphetamine and amphetamines salts are also reported to be efficacious.6 Stimulant medications are FDA approved for use with ADHD (minimum age of 3 for dextroamphetamine, minimum age of 6 for methylphenidate). Although the majority of the studies were short term, lasting less than 12 weeks, longer term trials of up to 24 months also revealed stable long-term improvements, as long as medication was taken.7 Of interest is that during a naturalistic followup over 24 to 60 months, there appeared to be a gradual increase in noncompliance with treatment and fewer physician visits per year.8
GUIDELINES FOR USE
Once the diagnosis of ADHD is established according to accepted practice and baseline measures indicate that the severity of the disorder warrants a medication trial, clinicians must educate the parents or guardians and the patient about the treatment plan. At the first visit and all subsequent visits, the patient’s height, weight, and vital signs should be documented.6
Multiple stimulant preparations are available. Newer longer acting preparations of methylphenidate and mixed salts of amphetamine have been shown to be effective.9 There is limited evidence for choosing one stimulant over another. One study demonstrated that of a group of patients given both methylphenidate and dextroamphetamine, 40% responded to both, 26% responded best to methylphenidate, and 35% responded best to dextroamphetamine.10 Clinicians often employ longer-acting preparations after establishing tolerability with immediate-release stimulants. Fewer total daily doses per day appear to improve adherence. In addition, longer acting preparations eliminate the need for school-time dosing. Many longer acting preparations have been introduced since the mid-1990s. Although all contain the same active drug, these formulations differ pharmacologically because of modified-release technology. Many of these take advantage of a bead drug release technology or, in the case of methylphenidate XR (Concerta), a novel, osmotically driven delivery system. In addition, a dermal administration system (Daytrana) has recently been approved. The dermal administration allows for a short-term presence of the one isomer of methylphenidate that is rapidly metabolized in its first pass through the liver, but it is not clear that this fact alters the effects of methylphenidate.
If possible, it is advisable to start a medication trial on a Saturday, so that parents or caregivers can observe the effect or side effects. For optimum effect, the child or adolescent should be seen regularly by the physician to review the effect of the dose trial; the physician should use global parent’s or caregiver’s report and patient’s report, along with standard rating scales. The treatment of ADHD practice parameters from the American Academy of Child and Adolescent Psychiatry provides the reader with many other tips for initiation of stimulants.6 The dose ranges of medication for ADHD are as listed in Table 8C-1.
Comorbid psychiatric disorders complicate the treatment of ADHD with stimulants. Anxiety occurs in 25% of clinic-referred patients with ADHD.11 Results of a multisite study revealed that children with ADHD with and without anxiety responded similarly to methylphenidate on all study outcome domains.6,12 Treatment of ADHD and comorbid tic disorders remains challenging. Results of randomized controlled studies by several groups have suggested that stimulants can be safely and effectively prescribed in ADHD patients with comorbid tic disorders.13,14 Tics may emerge in 9% of children treated with stimulants but persist in fewer than 1%.15 One study revealed that the combined use of methylphenidate and clonidine led to reduction in tic severity, reduction in impulsivity, and improvement in attention.16 Management of ADHD and comorbid mood disorders remains challenging and not well studied. ADHD often manifests with concurrent mood disorders (6% to 38% of patients).7,17 Few studies have assessed treatment of comorbid ADHD and depression. In most, methylphenidate has been combined with a selective serotonin reuptake inhibitor (SSRI) with positive results.18 There is a suggestion that stimulants can worsen moods in patients with bipolar disorder,19 but this is not yet clear; the differential of juvenile mania and ADHD continues to be examined. Finally, studies of the treatment of ADHD and comorbid substance abuse suggest that stimulant medication have a protective effect against later substance abuse by adolescents.20
ADVERSE EFFECTS AND THEIR MANAGEMENT
The most frequent and troublesome immediate side effects include insomnia, anorexia, headache, irritability, weeping, tachycardia, and elevated blood pressure (Table 8C-2). Many of the symptoms diminish over a period of weeks. The 2002 American Academy of Child and Adolescent Psychiatry practice parameters describe commonly employed methods of managing these side effects.6 The effect of stimulants on long-term growth, particularly height, has been controversial. In the multisite study on treatment of ADHD, subjects at 24 months showed slower growth velocity than did nonmedicated children (about a half inch per year slower).8 However, the children in the study were initially taller than average. It is unclear whether the medicated children catch up. Overall, children who stayed on stimulants did better globally, but the tradeoff might be the slight reduction in growth velocity.
| Adverse Effect | Management Strategies |
|---|---|
| Insomnia |
Adapted from Greenhill LL, Pliszka S, Dulcan MK, et al: Practice parameters for the use of stimulant medications in the treatment of children, adolescents and adults. J Am Acad Child Adolesc Psychiatry 41(2 suppl):26S-49S, 2002.
CURRENT CONTROVERSIES
There continue to be concerns that stimulants are overprescribed. When the diagnosis is carefully established, according to some authors, undertreatment remains the major concern.21 The treatment of preschoolers has increased, according to one survey, by 169%.22 There has been only a small number of randomized controlled studies of stimulants in this population.23 It appears that these medications are efficacious, but this age group is also more prone to side effects.23 The long-term effect of stimulants also remains controversial. One of the longest running multisite studies has shown that the symptoms in patients who started taking stimulants were similar to those of patients who were unmedicated.8 This appears to be mostly related to compliance with medication, and patients who continued to use stimulant medication maintained their global improvements. The significance of a concern related to cardiac and emotional side effects of a particular long-acting methylphenidate preparation is uncertain. There has also been concern about long-acting mixed salts of amphetamine. Carefully obtaining informed consent for all patients is prudent, and avoiding these medications in patients with structural cardiac disorders is recommended. One study revealed that children starting methylphenidate had white blood cell changes that increased the risk of cancer. The numbers of children studied were small, and previous animal studies and one surveillance study of cancer related to methylphenidate did not demonstrate the relationship. Further study is necessary to determine whether this finding is a concern.
Atomoxetine
Atomoxetine was the first nonstimulant medication approved for the treatment of ADHD. It is a highly selective norepinephrine reuptake inhibitor that may also have dopaminergic effects in the prefrontal cortex. Atomoxetine has FDA approval for the treatment of ADHD in children, adolescents, and adults. The drug manufacturer provides most of the evidence base for atomoxetine. Results of several large studies indicate it is significantly better than placebo across several measures.24 It also appeared to be comparable in efficacy with methylphenidate in one study to date.25
The most common side effects reported in children and adolescents include sedation, dizziness, change in appetite, and mood instability. Mood instability may be more common in patients who have a bipolar spectrum disorder along with comorbid ADHD. At the time of this writing, the FDA was also considering adding a “black box warning” because of a slight increase in suicidal behavior.26 An independent review of this issue is lacking. Premarket studies documented a slight increase in blood pressure and pulse.25 Drug interactions are also of concern, particularly with agents that are CYP2D6 inhibitors, such as fluoxetine or paroxetine. Two cases of hepatic toxicity have been reported, both of which resolved with stopping the medication. Seven cases of suicidal thoughts were found on reanalyses of the existing studies. It is important to monitor patients for suicidal tendencies.
α-Adrenergic Agents
α-Adrenergic medications such as clonidine and guanfacine are commonly prescribed for patients with ADHD who have comorbid tics, insomnia, or aggression. The α-adrenergic drugs affect central presynaptic and postsynaptic α2-adrenergic receptors and mediate cognition and attention through norepinephrine.27 Clonidine appears to have more potent mixed receptor effects than does guanfacine.28 Possible indications for the α-adrenergic drugs include tic disorders, ADHD, sleep disturbances caused by stimulants, aggression, and hyperarousal from posttraumatic stress disorder.
There are few controlled studies of the α-adrenergic drugs.29 The number of patients in each study is relatively small. One multisite study demonstrated effectiveness of clonidine and of clonidine plus methylphenidate for the treatment of tics and ADHD.30 A similar study of guanfacine also demonstrated improvement in patients with ADHD and tics.
GUIDELINES FOR USE
Common side effects for both agents include dry mouth, sedation, fatigue, dizziness, weakness, hypotension, and bradycardia. In addition, there are reports of depressive symptoms with clonidine.31 When abrupt withdrawal of α adrenergics occurs, rebound hypertension may occur. Therefore, it is advisable to taper both medications gradually, at a rate of 0.05 mg every 3 to 5 days for clonidine and 0.5 mg every 3 to 5 days for guanfacine.
ANTIDEPRESSANTS
Antidepressants, particularly the SSRIs, are increasingly used worldwide in the pediatric population.3 However, research regarding the efficacy and safety for children and adolescents has yielded mixed results and remains inadequate.
SSRIs increase the amount of serotonin in the synaptic cleft. Tricyclic antidepressants block the reuptake inactivation of serotonin and norepinephrine. Newer, so-called novel antidepressants affect serotonin, norepinephrine, and dopamine in varying ways. All of these immediate effects lead to subsequent changes at the level of neurotransmitters that reduce depressive symptoms.32
There are multiple indications for the use of antidepressants, some with FDA approval and some off label.69,70 Table 8C-3 and Table 8C-4 outline these indications.
Selective Serotonin Reuptake Inhibitors
The evidence base for the treatment of depression in children and adolescents is improving.33 The Treatment of Adolescent Depression Study clearly showed the benefit of both fluoxetine and the combination of fluoxetine and cognitive behavioral therapy.34 In addition, the study demonstrated the reduction in suicidal behavior for the course of the study. Table 8C-3 lists the research base to date for the treatment of juvenile depression with antidepressants.
OTHER INDICATIONS
At this time, the strongest evidence for efficacy with the SSRIs is with obsessive-compulsive disorder.33 Five randomized, controlled trials have yielded results indicating positive response in comparison to placebo. Also, treatment of other mixed anxiety disorders with these medications is supported. Table 8C-4 lists evidence to date for use of antidepressants in a variety of psychiatric conditions.
Novel Antidepressants
This category includes venflaxine, bupropion, and mirtazapine. The evidence for the efficacy of these newer antidepressants for any condition is scant.32 Several small studies of bupropion for ADHD that have yielded positive results.35 One study yielded negative results for venlafaxine in major depression.36 Two open label studies of juveniles with ADHD demonstrated some improvement on certain ADHD rating scales.37 With regard to other novel antidepressants, there have been no randomized controlled trials, but there have been some open label trials for depression and insomnia.38
Tricyclic Antidepressants
Of the 13 studies of tricyclic antidepressants for major depression, none yielded positive findings.33 Clomipramine has been well studied for obsessive-compulsive disorder, and three studies have yielded positive findings indicating its efficacy for obsessive-compulsive disorder. Imipramine has been established as an effective medication for enuresis. Imipramine, amitriptyline, and desipramine have all been found to be effective for ADHD.39
Guidelines for Use
Once the decision is made, in collaboration with parents or guardians, to initiate a trial of an antidepressant, the clinician needs to review the current FDA warnings and guidelines for their use.40 The black box warning describes the possible risk of increased suicidal behavior in patients who are taking antidepressants. In addition, the FDA has provided guidance to enhance the monitoring of patients who have begun taking antidepressants. The current recommendations are four weekly face-to-face contacts for the first month, biweekly contacts for the second month, and another contact at 12 weeks. Subsequent frequency of followup is guided by clinical necessity. The American Academy of Child and Adolescent Psychiatry and the American Psychiatric Association have created a guide for clinicians and one for parents of children who are being treated with antidepressants.41 The guide discusses the potential deleterious effect of the FDA warning on the treatment of depression in children and adolescents by primary care clinicians. The risk of untreated major depression leading to suicide clearly exceeds the relatively small risk of these medications for inducing suicidal behavior in juveniles. Without treatment, the consequences of depression are extremely serious.
The antidepressant drug of first choice is not clear. Fluoxetine is the only antidepressant approved by the FDA for treatment of depression in pediatric patients. Off-label prescribing of antidepressants is both common and consistent with clinical practice. Of the approximately 30% to 40% of children and adolescents who do not respond to an initial medication, a substantial number respond to an alternative.41
SSRIs, novel antidepressants, and tricyclic antidepressants should all be initiated at low dosages to avoid adverse effects. The dosages should be slowly titrated to monitor for adverse effects, particularly behavioral activation or manic symptoms. Family members should contact their clinician when any of the following emerge: patients express new or more frequent thoughts of wanting to die or hurt themselves; signs of increased anxiety/panic, agitation, aggression, or impulsivity; or evidence of involuntary restlessness, elation, or increased energy. Table 8C-4 lists dosage ranges.
Adverse Effects
Table 8C-5 lists common side effects of antidepressants. Common adverse effects of the SSRIs include nausea, decreased appetite and weight loss, insomnia, sedation, sweating, and sexual dysfunction. More rare side effects include behavioral activation or manic symptoms, allergic reactions, and increased suicidal behavior.
Current Controversies
With the introduction of the FDA black box warning, there appears to be a trend of a reduced number of prescriptions of SSRIs and novel antidepressants. Primary care physicians and clinicians have become more anxious about prescribing these medications. It is clear, however, from worldwide research that introduction of these medications has led to reductions in suicide rates in countries in which the medications are prescribed.42 The concern is that the black box warning will result in even more delay in appropriate treatment of major depression, which in turn could possibly result in more suicide deaths.
The efficacy of SSRIs for major depression appears to be emerging, despite some negative studies. More needs to be done in this area to ensure that these medications are clearly more efficacious than placebo. One of the challenges seems to be discriminating unipolar disorders from bipolar disorders. Apparently, up to 40% of patients who ultimately have bipolar disorder present first with a depressive episode.43 It is clinically challenging to make this differentiation. However, antidepressants taken by patients with bipolar disorder can lead to exacerbation in mood symptoms.44,45 More research needs to be done to help with this distinction. In general, clinicians need to be extremely vigilant when treating adolescents and children with antidepressants, especially in the first weeks after initiation of treatment.
ANTIPSYCHOTICS
Patients with psychotic symptoms were the intended users of antipsychotic agents, both typical and atypical. However, clinicians more widely prescribe these drugs for other indications such as aggressive behavior in juveniles, pervasive developmental disorders, severe ADHD, tic disorders, and certain mood disorders.1
Typical antipsychotics preferentially block dopamine D2 receptors in the mesolimbic, mesocortical, and nigrostriatal areas. “Atypical “antipsychotics have a weaker affinity for dopamine D2 receptors and varying affinity for other dopamine receptors. There also is a greater specificity for the mesocortical and mesolimbic areas. There is a stronger affinity for serotonergic receptors, which seems to result in differences in the side effect profile between the two groups, as well as enhanced efficacy for symptoms of schizophrenia.46
Common indications, both FDA approved and off label, are listed in Table 8C-6. Some of the typical agents are approved for use in psychosis in children and adolescents, severe behavior disorders, ADHD, and severe anxiety. Pimozide and haloperidol are approved for Tourette syndrome. The use of these medications for a variety of other disorders is supported by a limited evidence base. Research has documented the effectiveness of typical antipsychotics, such as haloperidol, in schizophrenia, autistic disorders, tic disorders, conduct disorder, and mental retardation.33 Research has also demonstrated the effectiveness of atypical antipsychotics, such as risperidone, in tic disorders, conduct disorder, autism, and mental retardation.33 To date, the best evidence for efficacy of these agents is with autism.47 These agents have also been studied for the treatment of pediatric bipolar disorder.1
Guidelines for Use
In view of the limited evidence base just described, it is important to establish the specific diagnosis and target symptoms thought to be responsive to these agents.48 Methods of tracking improvements need careful consideration. This may include rating scales, parents’ and teachers’ reports, patient’s reports, and clinician’s observation. Baseline medical evaluations for patients taking these medications include a recent physical examination, with documentation of height, weight (and body mass index), blood pressure, heart rate, temperature, and electrocardiographic measurements. A baseline investigation for abnormal involuntary movements should be conducted (with a standard measure), and any preexisting extrapyramidal symptoms should be documented. In addition, standard laboratory evaluation should include a comprehensive hepatic panel, fasting glucose measurement, fasting lipid profile, complete blood cell count with differential, and possibly prolactin level measurement. Other evaluations to consider include electroencephalography, especially if clozapine is being considered.
Because of the side effects of these medications, careful informed consent is required from both patient and parent or guardian. This discussion should include describing the off-label use of most of these agents. The dosage ranges for each agent are presented in Table 8C-6. The choice of agents is most often based on side effect profile. Lower initial dosing, until tolerance of the medication is established, is essential. Once the patient has started taking the medication, regular scheduled followup is imperative, and constant monitoring of the efficacy of the medication and side effects is necessary. Patients should be encouraged to maintain regular exercise and consider a nutrition consultation. After a period of 6 to 12 months of steady improvement in clinical symptoms, the clinician might consider reducing the dosage to find the lowest effective dosage.49 For patients with conditions refractory to these agents, it is prudent to consider assessing for rarer central nervous system disorders.48
Adverse Effects
Table 8C-6 lists the common adverse effects of this category of medications. The most common concern with typical antipsychotics is the development of extrapyramidal symptoms such as dystonia, tremor, and other parkinsonian symptoms. In addition, these agents can induce involuntary and persistent dyskinetic movements and tardive dyskinesia. Atypical agents, in general, do not cause the same degree of extrapyramidal symptoms. The side effect of most concern in this category has been weight gain and the possible induction of type 2 diabetes.50
Current Controversies
Since the mid-1990s, clinicians have increased their prescribing of atypical antipsychotics for the multiple indications listed previously. The evidence base for use of these medications for most of the disorders is weak.33 The significant weight gain documented with most of these agents is of great concern, and the risk of obesity is significantly elevated whenever these medications are initiated.46 The long-term benefits of the medications need to be considered against these very serious medical complications.
MOOD STABILIZERS
Medications that treat at least one mood state of bipolar disorder without worsening the other mood state are called mood stabilizers.51 This category includes lithium and many of the anticonvulsants. Although the atypical antipsychotics have properties of mood stabilization, they are not included in this category at this time.
The mechanism of action of lithium remains unknown. It appears to act through augmentation of the serotonergic system, affecting the second messenger system and upregulating a neuroprotective protein. It also may increase gray matter, as evidenced by neuroimaging.52
The mechanism of actions of anticonvulsants are also unknown; however, they appear to enhance γ-amino butyric acid (GABA) and decrease glutamate. These medications also increase neuroprotective factors.53
Table 8C-7 lists the indications to date of mood stabilizers in the treatment of child and adolescent psychopathology.
Guidelines for Use
When mood stabilizers are used in the treatment of mania, depression, or aggression, it is crucial that the specific target symptoms be defined. Algorithms now exist for choosing medications for the treatment of juvenile bipolar disorder on the basis of the evidence and expert consensus.54 Baseline rating scales for tracking mania, depression, or aggression are available.55 In addition, longitudinal and prospective mood charting is very helpful in determining the effect of these medications on the targeted symptoms. Once the decision to prescribe these medications is made, the following should be completed: physical examination, vital sign measurements, height and weight measurements, and specific laboratory tests. For lithium, a complete blood cell count with differential; blood urea nitrogen, creatinine, and electrolyte measurements; thyroid profile; and pregnancy test are necessary. In addition, an electrocardiogram should be obtained; if clinically necessary, an electroencephalogram should also be obtained. For the anticonvulsants, all of these procedures should be completed, with the addition of a hepatic profile and lipid profile.
Adverse effects of lithium and the anticonvulsants are listed in Table 8C-7. It is also important to be wary of specific drug interactions.
Current Controversies
Increasingly, clinicians are prescribing mood stabilizers for many children and adolescents who have symptoms of mania but do not fulfill the diagnostic criteria for bipolar disorder.55,56 Frequently, the main target symptom is irritability and rage. Although some studies have indicated the efficacy of these medications for this symptom, the risk of significant side effects must be considered. In addition, the frequency of treating patients with more than one medication for their emotional disorder is increasing. However, if the diagnosis of bipolar disorder is accurate, the risks of not aggressively treating these individuals include worsening or progressing of the condition.55
ANXIOLYTICS
The evidence base for the usefulness of benzodiazepines for anxiety is limited.33 There have been few randomized controlled trials.57 In addition, there is a high placebo response rate, and the active medications are often not significantly better than placebo.
Current Controversies
There is inadequate study of the long-term use of benzodiazepines in children and adolescents. The risk of dependence and abuse with these medications is high. There does seem to be a role for these medications in the short-term management of anxiety. Their role in reducing acute agitation in adolescents is not as clear. The induction of disinhibited behavior continues to be a reported concern, although this is not carefully documented in studies of these adolescents.58
RATIONAL POLYPHARMACY
Children and adolescents often have more than one psychiatric diagnosis; comorbidity is the rule, not the exception. In patients with multiple diagnoses or one diagnosis of a condition refractory to monotherapy, polypharmacy may be warranted. The mechanisms of actions of these combined treatments are not known. There are no current approved indications for combined agents. One report reviewed studies of rates of polypharmacy in the United States.59 Psychiatric inpatient facilities have higher rates of polypharmacy prescriptions than do outpatient facilities and pediatric offices.1,59 In all populations, stimulants plus another agent seem to be the most frequent form of polypharmacy.1,59 In addition, there has been an increase in the rates of prescribing atypical antipsychotics.1,59 The most significant concern with polypharmacy is the increased risk of adverse events. Drug-drug interactions are a particular concern.
Although there is some evidence for the efficacy for combined stimulant and α-adrenergic treatment of ADHD and tic disorders, research in this area is limited.60 In addition, there are reports on the treatment of ADHD and depression with stimulants and SSRIs.61
NONSTANDARD AND ALTERNATIVE THERAPIES
Alternative therapies, such as vitamins and herbal medications, are gaining increasing attention because of their widespread use. Despite the limited study of these agents, they continue to be of interest to parents of children with psychiatric disorders. Reviews have indicated that there is evidence for few of these agents of their effectiveness in children and adolescents.62
Omega-3 fatty acids have been studied in adults for mood disorders and in children and adolescents for ADHD. Preliminary investigations have generally not demonstrated any clear benefits.33 However, further study of these agents may be useful.
Uses of melatonin, an exogenous hormone, include a variety of psychiatric disorders. Preliminary studies on a small number of subjects have suggested that melatonin may be appropriate treatment for a variety of sleep disorders. Children with development disabilities may be particularly responsive.63 Doses of melatonin have varied from 1 to 3 mg/day. It generally appears to be safe. The most common side effects include nightmares, headaches, morning sedation, mild depression, and decreased libido.
Researchers of St. John’s wort in adult depression have found effectiveness in mild to moderate, but not severe, depression.64 To date, there are no published data concerning the use of St. John’s wort in children and adolescents. Side effects with this agent are limited, with reports of fatigue, restlessness, and headache.
FUTURE DIRECTIONS
The evidence base for pharmacological treatments for child psychiatric disorders is limited but improving. The importance of advancing knowledge is clear. One exhaustive epidemiological study documented the high rates of childhood psychiatric disorders.65 Twenty percent of children and adolescents suffer from a significant emotional disorder. Half of all lifetime cases of emotional disorder begin by age 14, and 75%, by age 24. Of those ill children and adolescents, only about 30% receive treatment. Lack of access to care from qualified mental health professionals remains a large, unmet need. The projected need for child psychiatrists is not keeping up with the projected increase of at-risk children and adolescents. It is likely that nonpsychiatry clinicians, such as primary care physicians and nurse practitioners, will need to fill these gaps.66 Currently, there is great variability between clinicians and between different communities with regard to standards of psychopharmacological care for children and adolescents. There is a clear need for more well-defined standards of care. Practice parameters currently exist but are based mainly on clinical opinion and limited research. One exciting research initiative is the Child and Adolescents Clinical Trials Network (CAPTN).67 This is a nationwide collection of investigators representing the entire prescribing community, enrolling a few patients at each site, which leads to a large overall number. Multiple investigators will use this network for variety of psychopharmacological studies in children and adolescents. This network may be able to address the absence of long-term safety data for most psychotropic agents in use. In addition, the efficacy of polypharmacy should be studied.
1 Jensen PS, Vinod SB, Vitiello B, et al. Psychoactive medication prescribing practices for U.S. children: Gaps between research and clinical practice. J Am Acad Child Adolesc Psychiatry. 1999;38:5.
2 Olfson M, Marcus SC, Weissman M, et al. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry. 2002;41:5.
3 Williams J, Klinepeten K, Palmes G, et al. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2005;114:601-606.
4 Rappaport N, Chubinski P. The meaning of psychotropic medications for children, adolescents and their families. J Am Acad Child Adolesc Psychiatry. 2000;39:9.
5 Safer DJ, Zito JM. Pharmacoepidemiology of psychotropic medications in youth. In: Rosenberg D, Davanzo PA, Gershon S, et al, editors. Pharmacotherapy for Child and Adolescent Psychiatric Disorders. New York: Marcel Dekker; 2002:23-50.
6 Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameters for the use of stimulant medications in the treatment of children, adolescents and adults. J Am Acad Child Adolesc Psychiatry. 2002;41(2 suppl):26S-49S.
7 A 14-month randomized clinical trial of treatment strategies for attention deficit hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999;56:1073-1086.
8 MTA Cooperative Group, National Institute of Mental Health Multimodal Treatment Study of ADHD followup. 24-Month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics. 2004;113:754-761.
9 Biederman J, Spencer T, Wilen T. Evidence-based psychotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7:77-97.
10 Elia J, Borcheding B, Rapoport J, Keysor C. Methylphenidate and dextroamphetamine treatments of hyperactivity: Are there true non-responders? Psychiatry Res. 1991;36:141-155.
11 Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depression, anxiety and other disorders. Am J Psychiatry. 1991;148:564-577.
12 Diamond IR, Tannock R, Schachar RJ. Response to methylphenidate in children with ADHD and comorbid anxiety. J Am Acad Child Adolesc Psychiatry. 1999;38:402-409.
13 Castellanos FX, Giedd JN, Eliz J, et al. Controlled stimulant treatment of ADHD and comorbid Tourette’s syndrome: Effects of stimulants and dose. J Am Acad Child Adolesc Psychiatry. 1997;36:589-596.
14 Law SF, Schachar RJ. Do typical clinical doses of methylphenidate cause tics in children treated for attention-deficit hyperactivity disorder? J Am Acad Child Adolesc Psychiatry. 1997.
15 Liplin PH, Goldstein IJ, Adesman AR. Tics and dyski-nesias associated with stimulant treatment in attention deficit hyperactivity disorder. Arch Pediatr Adolesc Med. 1994;148:859-861.
16 The Tourette’s Syndrome Study Group. Treatment of ADHD in children with tics: A randomized controlled trial. Neurology. 2002;58:527-536.
17 Pliszka SR. Comorbidity of attention deficit hyperactivity disorder with psychiatric disorder: an overview. J Clin Psychiatry. 1998;59(suppl 7):50-58.
18 Findling RL. Open-label treatment of comorbid depression and attentional disorders with co-administration of serotonin reuptake inhibitors and psychostimulants in children, adolescents and adults: A case series. J Child Adolesc Psychopharmacol. 1996;3:1-10.
19 Biederman J, Klein RG, Pine DS, et al. Resolved mania is mistaken for ADHD in prepubetal children. J Am Acad Child Adolesc Psychiatry. 1998;37:1091-1096.
20 Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity beget later subtance abuse? a meta-analytic review of the literature. Pediatrics. 2003;111:179-185.
21 Jensen P, Kettle L, Roper MT, et al. Are stimulants overprescribed? Treatment of ADHD in four US communities. J Am Acad Child Adolesc Psychiatry. 1999;38:797-804.
22 Zito JM, Safer DJ, dosReis S, et al. Trends in prescribing of psychotropic medications to preschoolers. JAMA. 2000;283:1025-1030.
23 Firestone P, Musten LM, Pisterman S, et al. Short-term side effects of stimulant medications are increased in preschool children with attention-deficit/hyperactivity disorder: A double-blind, placebo-controlled study. J Child Adolesc Psychopharmacol. 1998;8:13-25.
24 Spencer T, Heiligenstein JH, Biederman J. Results from 2 proof-of-concept, placebo-controlled studies of atomoxetine in children with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2002;63:1140-1147.
25 Michelson D, Faries D, Wernike J. Atomoxetine in the treatment of children and adolescents with attention deficit/hyperactivity disorder: A randomized, placebo-controlled, dose response study. Pediatrics. 2001;108(5):E83.
26 U.S. Food and Drug Administration: Public Health Advisory on Atomoxetine. September 29, 2005. (Available at: http://www.fda.gov/bbs/topics/news/2005/new01237.html; accessed 10/27/06.)
27 Hunt RD, Capper L, O’Connell P. Clonidine in child and adolescent psychiatry. J Child Adolesc Psychopharmacol. 1990;1:87-101.
28 Arnstein AF, Steere JC, Hunt RD. The contribution of alpha 2-noradrenergic mechanisms of prefrontal cortical cognitive function. Potential significance for attention-deficit hyperactivity disorder. Arch Gen Psychiatry. 1996;53:448-455.
29 Joshi SV. Psychostimulant, atomoxetine, and alpha-agonists. In: Steiner H, editor. Handbook of Mental Health Interventions in Children and Adolescents: An Integrated Developmental Approach. San Francisco: Jossey-Bass; 2004:258-287.
30 Tourette’s Syndrome Study Group. Treatment of ADHD in children with tics: A randomized controlled trial. Neurology. 2002;58:527-536.
31 Steingard R, Biederman J, Spenser T, et al. Comparison of clonidine response in the treatment of attention deficit hyperactivity disorder with and without comorbid tic disorders. J Am Acad Child Adolsc Psychiatry. 1993;32:350-353.
32 Emsle GJ, Walkup JT, Pliska SR. Non-tricyclic antidepressants: Current trends in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38:517-528.
33 McClellan JM, Werry JS. Evidence-based treatments in child and adolescent psychiatry: An inventory. J Am Acad Child Adolesc Psychiatry. 2003;42:12.
34 Treatment for Adolescents with Depression (TADS) Team. Fluoxetine, cognitive-behavioral therapy and their combination for adolescents with depression. JAMA. 2004;292:807-820.
35 Connors CK, Casat CD, Gualtieri CT, et al. Bupropion hydrochloride in attention deficit disorder with hyperactivity. J Am Acad Child Adolesc Psychiatry. 1996;35:1314-1321.
36 Mandoki M, Tapia MR, Tapia MA, et al. Venlafaxine in the treatment of children and adolescents with major depression. Psychopharmacol Bull. 1997;33:149-154.
37 Findling RL. Open label treatment of comorbid depression and attention deficit disorder. J Child Adolesc Psychopharmacol. 1996;6:165-175.
38 Emslie G, Portteus A, Kumar E, et al. Antidepressants: SSRIs and novel atypical antidepressants-An update on psychopharmacology. In: Steiner H, editor. Handbook of Mental Health Interventions in Children and Adolescents: An Integrated Developmental Approach. San Francisco: Jossey-Bass; 2004:318-362.
39 Geller B, Reising D, Leonard H, et al. Critical review of tricyclic antidepressant use in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38:513-516.
40 U.S. Food and Drug Administration: FDA Public Health Advisory: Suicidality in Children and Adolescents Being Treated with Antidepressant Medication, October 15, 2004. (Available at: http://www.fda.gov/cder/drug/antidepressants/SSRIPHA200410.htm; accessed 10/27/06.)
41 American Psychiatric Association, American Academy of Child and Adolescent Psychiatry: The Use of Medication in Treating Childhood and Adolescent Depression: Information for Physicians, January 2005. (Available at: http://www.parentsmedguide.org/physicansmedguide.pdf; accessed 10/27/06.)
42 American College of Neuropsychopharmacology, Executive Summary Preliminary Report of the Task Force on SSRI and Suicidal Behavior in Youth. January, 2004.
43 Geller B, Fox LW, Clark KA. Ratio and predictors of prepubertal bipolarity during followup of 6- to 12-year-old depressed children. J Am Acad Child Adolesc Psychiatry. 1994;33:461-468.
44 Carlson GA. The bottom line. J Child Adolesc Psychopharmacol. 2003;13:115-118.
45 Biederman J, Mick E, Prince J, et al. Therapeutic dilemmas in the pharmacotherapy of bipolar depression in the young. J Child Adolesc Psychopharmacol. 2000;10:185-192.
46 Findling R, Schulz S, Reed M, et al. The antipsychotics. A pediatric perspective. Pediatric Clin North Am. 1998;45:1205-1232.
47 McCracken JT, McGough J, Shah B. Risperidone in children with autism and serious behavioral problems. N Engl J Med. 2002;347:314-321.
48 McClellan J, Werry J. Practice parameters for the assessment and treatment of children and adolescents with schizophrenia. J Am Acad Child Adolesc Psychiatry. 2001;40(7 suppl):4S-23S.
49 DeJong S, Ginliano A, Frazier J. Antipsychotic medication. In: Steiner H, editor. Handbook of Mental Health Interventions in Children and Adolescents: An Integrated Developmental Approach. San Francisco: Jossey-Bass; 2004:413-464.
50 Food and Drug Administration: Warning about hyperglycemia and atypical antipsychotic drugs. FDA Patient Safety News Show #28, June, 2004. (Available at: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/printer.cfm?id=229; accessed 10/27/06.)
51 Keck P, McElroy S. Redefining mood stabilization. J Affect Disord. 2003;73:163-169.
52 Moore G, Bebchuk J, Wilds I, et al. Lithium-induced increase in human brain grey matter. Lancet. 2000;356:1241-1242.
53 Manji H, Moore G, Chen G. Clinical and preclinical evidence for the neurotropic effects of mood stabilizers: Implications for the pathophysiology and treatment of manic-depressive illness. Biol Psychiatry. 2000;48:740-754.
54 Paruluri M, Henry D, Devieneni B, et al. A pharmacotherapy algorithm for stabilization and maintenance of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2004;43:859-867.
55 Paruluri M, Birmaher B, Naylor M. Pediatric bipolar disorder: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2005;44:846-871.
56 Carlson GA, Kelly KL. Mania symptoms in psychiatrically hospitalized children. What do they mean? J. Affect Disord. 1998;51:123-125.
57 Simeon J, Knott V, Thatte S, et al. Pharmacotherapy of childhood anxiety disorder. Clin Neuropharmacol. 1992;15:229-230.
58 Thienemann M. Medications for pediatric anxiety. In: Steiner H, editor. Handbook of Mental Health Interventions in Children and Adolescents: An Integrated Developmental Approach. San Francisco: Jossey-Bass; 2004:288-317.
59 Duffy F, Narrow W, Rae D, et al. Concomitant pharmacotherapy among youths treated in routine psychiatric practice. J Child Adolesc Psychopharmacol. 2005;15:12-25.
60 Wilens T, Spencer T, Swanson J, et al. Combining methylphenidate and clonidine: A clinically sound medication option. J Am Acad Child Adolesc Psychiatry. 1999;38:614-619.
61 Kratochvil C, Newcorn J, Arnold L, et al. Atomoxetine alone or combined with fluoxetine for treating ADHD with comorbid depression or anxiety symptoms. J Am Acad Child Adolesc Psychiatry. 2005;44:915-924.
62 Rojas N, Chan E. Old and new controversies in the alternative treatment of attention-deficit hyperactivity disorder. Ment Retard Dev Disabil Res Rev. 2005;11:116-130.
63 Smits M, Nagtegaal E, Vander H, et al. Melatonin for chronic sleep onset insomnia in children-A randomized placebo-controlled trial. J Child Neurol. 2001;16:86-92.
64 Shatkin J, Davanzo P. Atypical and adjunctive agents. In: Rosenberg D, Davanzo PA, Gershon S, et al, editors. Pharmacotherapy for Child and Adolescent Psychiatric Disorders. New York: Marcel Dekker; 2002:597-634.
65 Kessler R, Berglund P, Dember O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593-602.
66 Satcher D: Surgeon General Agent-National Action Agenda for Children’s Mental Health. January 2001.
67 March J: The Child and Adolescent Psychiatry Trials Network. Washington, DC: National Institute of Mental Health and American Academy of Child and Adolescent Psychiatry, 2005.
68 Emslie GJ, Rush AJ, Weinberg WA, et al. A double blend, randomized, placebo controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry. 1997;54:1031-1037.
69 Emslie GJ, Heilgenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents: A placebo controlled randomized clinical trial. J Am Acad Child Adolesc Psychiatry. 2002;41:1205-1214.
70 Keller MB, Ryan ND, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: A randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2001;40:762-772.
71 Wagner KD, Robb AS, Findley R, et al: Citalopram treatment of pediatric depression: Results of a placebo controlled trial. Sponsored by Hirschfield RMA. Presented at American College of Neuropsychopharmacology, Waikoloa, HI, 2001.
72 Wagner KD, Wohlberg CJ: Efficacy and Safety of Sertraline in the Treatment of Pediatric Major Depressive Disorder (MDD). Presented at the 155th annual meeting of the American Psychiatric Association, Philadelphia, 2002.
73 Emslie GJ, Findling RL, Rynn MA, et al: Efficacy and safety of nefazodone in the treatment of adolescents with major depressive disorder. Presented at the 42rd annual meeting of the New Clinical Drug Evaluation Unit, Boca Raton, FL, 2002.
74 Ryan ND. Medication treatment for depression in children and adolescents. CNS Spectrums. 2003;8:283-287.
Birmaher B, Brent D, Benson R. Summary of the practice parameters for the assessment and treatment of children and adolescents with depressive disorder. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1998;37:1234-1238.
Bernstein G, Kinlan J. Practice parameters for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 36(suppl), 1997.
Myers K, Winters NC. Ten-year review of rating scales. II: Scales for internalizing disorders. J Child Adolesc Psychopharmacol. 2002;41:634-659.
8D. Evidence-Based Psychological Interventions for Emotional and Behavioral Disorders
Psychological interventions include a wide array of behavioral and psychotherapeutic treatments designed to reduce psychological distress and maladaptive behavior and to increase adaptive behavior, typically through counseling, support, interaction, or instruction. For younger children and adolescents (hereafter referred to collectively as children except when a distinction is necessary), such interventions are conducted with the children themselves, their parents, their teachers, and/or other significant persons in their lives. Psychological treatments have traditionally been administered largely by professionals with specialized therapy training (e.g., psychiatrists, psychologists, clinical social workers) who work in mental health or psychiatric settings (e.g., inpatient psychiatric hospitals, outpatient mental health clinics). Unfortunately, evidence suggests that only a small minority of the estimated 20% of children experiencing significant mental health problems ever receive such treatment.1 Because of this, there is an increasing awareness that access to care can be improved if mental health screening, referral, and even service provision are integrated into settings in which children in need are most likely to be observed (e.g., schools, primary care practices). The objectives of this chapter are to provide a review of the empirical evidence supporting psychological interventions for emotional and behavioral disorders and to encourage informed referral and enhanced care for children seen in pediatric and primary care settings. The chapter begins with a brief introduction to the child psychological treatment literature as a whole and then describes the specific psychological interventions with the strongest evidence base for treating the most common emotional and behavioral problems experienced by children.
OVERVIEW OF PSYCHOLOGICAL INTERVENTION LITERATURE
There is a wealth of scientific literature supporting the efficacy of psychological treatments for mental health problems in children. More than 1500 trials have tested the effects of various psychological treatments for a broad range of childhood problems, including depression, anxiety, and disruptive behavior, and new trials begin each year.2 One method usd to summarize this literature is meta-analysis, in which study results are converted to a common effect size metric in order to combine the results from a group of studies into a single comprehensive analysis. Several meta-analyses have been conducted on this burgeoning evidence base, each demonstrating that psychological treatment is, on average, more effective than no treatment, wait-list, and placebo conditions.3–6 More specifically, the average effect sizes obtained in these meta-analyses were all at or above 0.71, which indicates that the average treated child showed better outcomes than did more than 75% of control children. Weisz and colleagues6 also found that these positive treatment effects endure beyond the end of treatment, at least over the 6-month followup periods typically examined.
Because of the overall efficacy of psychological treatment, complementary efforts have focused on identifying which particular treatments for specific child problems have the strongest research support. Perhaps the most visible of these efforts have been those initiated by the American Psychological Association’s Task Force on the Promotion and Dissemination of Psychological Procedures.7–9 The purpose of the Task Force was to identify effective psychological treatments for mental disorders and psychological aspects of physical disorders and to regularly update and distribute this list to mental health providers and training programs. The Task Force outlined criteria for three distinct levels of empirical support: well-established treatments, probably efficacious treatments, and experimental treatments. Well-established treatments are those with the highest level of supportive evidence, including multiple randomized controlled trials or a large series of well-done single-case design studies demonstrating their efficacy. Well-established treatments must also be clearly described in treatment manuals, and their efficacy must have been established by at least two unrelated investigative teams. Probably efficacious treatments are those supported by results of at least one randomized clinical trial or a small series of well-done single-case design studies, otherwise meeting the well-established criteria. Experimental treatments are those that have not received either level of support.
The original American Psychological Association Task Force reports9,10 focused primarily on adult interventions, but they spawned similar efforts to identify efficacious psychological interventions for children. A special section of the Journal of Clinical Child Psychology11 reported findings for well-established and probably efficacious interventions for depression,12 phobia and anxiety disorders,13 autism,14 conduct disorders,15 and attention-deficit/hyperactivity disorder (ADHD).16 A series of articles published from 1999 to 2001 in the Journal of Pediatric Psychology reported findings for elimination conditions,17,18 sleep problems,19 feeding problems,20 and obesity.21 A number of other reviewers have followed suit, using varied criteria to identify the treatments with the most consistent support for ameliorating a variety of child mental health problems, including child abuse and neglect,22 substance abuse,23,24 and autism and pervasive developmental disorders.25–27
In this chapter, we provide a review of efficacious psychological treatments for the four most common classes of child emotional and behavioral disorders: (1) depression and mood; (2) anxiety and fears; (3) attention problems, impulsivity, and ADHD; and (4) conduct problems and disorders. Coverage of treatments for other childhood disorders is beyond the scope of this chapter, but interested readers are referred to the cited reviews for information regarding evidence-based psychological treatments. For information about pharmacological interventions, readers are referred to Chapter 8C.
Previous reviews of empirically supported (evidence-based) psychological interventions have been criticized for not applying clear standards for how to synthesize positive and negative findings28 or, worse yet, for requiring only a minimum number of positive findings with no consideration of negative findings (e.g., Bickman29). In this chapter, we address these criticisms by including and evaluating both positive and negative findings. We briefly describe all available evidence for each problem and then provide greater detail for the psychological treatments with the most consistent empirical support. We also provide guidance for pediatricians and primary care physicians about factors to consider when making a referral for specialty mental health care. We focus on the treatments that (1) were examined in at least two separate randomized clinical trials and (2) showed an average unweighted effect size at or above 0.50 across all trials and across all outcome measures of the target problem (e.g., measures of anxiety for a study targeting anxiety). We chose an effect size of 0.50 because this is considered a medium effect and one that is large enough to be intuitively obvious; it indicates that the average treated child is better off after treatment than more than 69% of those who did not receive treatment (the control condition).30
To identify psychological treatments, we use data from an ongoing broad-based meta-analysis of the child treatment literature.31 Here we briefly describe that search process, the inclusion criteria that we applied, and the coding system used to characterize the studies. For a more detailed description of these procedures, please see Weisz and associates.2 We searched PsycINFO and Medline, standard computerized databases, for studies beginning in 1965 and continuing through December 2005, using key terms from previous meta-analyses.5,6 We also surveyed published reviews and meta-analyses of the child psychotherapy literature,3,32,33 followed reference trails of reviewed studies, and screened studies suggested by investigators in the field. This search led to a pool of more than 3000 published trials, of which 244 met our inclusion criteria.
PSYCHOLOGICAL MANAGEMENT OF DEPRESSION
The mood disorders that affect children include major depressive disorder, dysthymic disorder, bipolar I and II disorders, and cyclothymic disorder. Rates tend to increase as children age, from about 1.7% among children to 5.6% or higher among adolescents.34 Depression is associated with significant functional impairments and, often, physiological symptoms, such as psychomotor agitation or retardation and hypersomnia or insomnia. It also substantially increases the risk of suicide,35 and thus it is an area for essential clinical attention. For a more thorough review of the prevalence and expression of mood disorders, see Chapter 18A.
In our review, we sought randomized clinical trials of psychological treatments for children with a diagnosed mood disorder or subclinical depressive symptoms. Reflecting the relatively recent recognition that children and adolescents can experience depression, the treatment studies here are both newer (1986 to 2005) and fewer (20 studies testing 29 treatment conditions) than the other problem areas we describe later. In 15 (75%) of these studies, investigators used a no-treatment or wait-list control condition; of the remainder, 4 (20%) used an attention control condition and 1 (5%) used a placebo control condition. Three types of psychological interventions have shown consistently positive effects across two or more controlled trials: relaxation training; cognitive-behavioral therapy (CBT), including child-focused CBT, child CBT plus parent CBT, and family-focused CBT; and interpersonal therapy (Table 8D-1). All targeted unipolar depression and related symptoms. Other interventions have not yet been examined in multiple studies (e.g., self-modeling of positive affect and attachment-based family therapy for unipolar depression; multifamily psychoeducation groups for bipolar disorder).
Relaxation Training
Relaxation training is a class of techniques that include slow, controlled breathing; deep muscle relaxation (wherein the major muscle groups are tensed and relaxed); and guided imagery (e.g., the child is encouraged to imagine a calm, soothing scene). It has been examined in two studies36,37 for children with elevated levels of depressive symptoms; both studies showed significant decreases in depressive symptoms in comparison to no treatment. Relaxation training has not yet been examined in children with diagnosed depressive disorders. Furthermore, these two studies included only white children. Thus, although such techniques may well be worthwhile for children experiencing mild to moderate levels of distress, it remains to be seen whether these techniques alone would suffice for those experiencing diagnosable levels of depression.
Cognitive-Behavioral Therapy
As shown in Table 8D-1, CBT has received the most research attention. CBT has been supported across numerous clinical trials, some targeting just the children for intervention and others targeting both the children and their parents. CBT has demonstrated positive effects across a wide range of ages, across diverse racial and ethnic groups, and both with children who demonstrate elevated levels of depression symptoms and with those who meet diagnostic criteria for major depressive disorder, dysthymic disorder, or depression not otherwise specified. It been administered successfully in both individual and group formats. In addition to showing beneficial effects when tested in research settings, CBT has also been used effectively in school settings.36,38,39 It has also been examined as bibliotherapy (i.e., having children learn about the therapy components through reading, rather than interaction with a therapist) but with little success.40 To date, the successful CBT trials have all involved mental health professionals as therapists, and most of the investigators provided them with additional training, supervision, and a manual to guide the intervention.
CBT treats depression by addressing emotional, behavioral, and cognitive skill deficits linked with the onset and maintenance of depression. Several different CBT manuals have been examined. The Adolescent Coping with Depression Course developed by Clarke and colleagues41,42 has been used successfully across the greatest number of trials. For children, manuals include Taking Action43 and Primary and Secondary Control Enhancement Training.44 The manuals for children and adolescents vary in developmental level, but they share many core components:
 Affective education and mood monitoring (the child learns to recognize and label his or her own feelings and the feelings of others, and to monitor and chart his or her mood).
Affective education and mood monitoring (the child learns to recognize and label his or her own feelings and the feelings of others, and to monitor and chart his or her mood). Pleasant activity scheduling (the child learns to increase pleasant activities and decrease unpleasant and solitary activities).
Pleasant activity scheduling (the child learns to increase pleasant activities and decrease unpleasant and solitary activities). Cognitive restructuring (the child learns to identify and challenge irrational, negative thoughts and replace them with realistic, positive thoughts).
Cognitive restructuring (the child learns to identify and challenge irrational, negative thoughts and replace them with realistic, positive thoughts). Thought stopping or interruption (the child learns to distract himself or herself to stop ruminating, or obsessively thinking, about depressing topics).
Thought stopping or interruption (the child learns to distract himself or herself to stop ruminating, or obsessively thinking, about depressing topics). Social skills and assertive communication (the child learns strategies to make friends, improve his or her social support system and resolve interpersonal conflicts).
Social skills and assertive communication (the child learns strategies to make friends, improve his or her social support system and resolve interpersonal conflicts). Problem solving skills (the child learns to generate and evaluate potential solutions to problems and to make plans to implement the chosen solution).
Problem solving skills (the child learns to generate and evaluate potential solutions to problems and to make plans to implement the chosen solution). Reinforcement and self-reinforcement (the child is rewarded, and learns to reward himself or herself, for a variety of behaviors, including increasing activity level, problem solving, and social interaction).
Reinforcement and self-reinforcement (the child is rewarded, and learns to reward himself or herself, for a variety of behaviors, including increasing activity level, problem solving, and social interaction).In CBT, parents are often involved in their child’s treatment. Typically, parents are (1) informed of the skills their child is learning, (2) taught to reinforce their child’s efforts and behavior changes, and (3) encouraged to communicate better with their child via negotiation and problem solving. In most programs, this parent involvement occurs when one or both parents join the child’s session for a few minutes at the end of each appointment or, occasionally, attend an entire session together with the child or alone with the therapist. In other programs, parent involvement is more intense, including a series of parent or family sessions in addition to the sessions with the child. Two of the CBT studies actually tested the benefit of combined child CBT plus parent CBT versus child-focused CBT.45,46 Neither study found the combined treatment significantly better than child-focused CBT.
Interpersonal Therapy for Adolescents
Interpersonal therapy has been examined in two studies, each focused on adolescents with a diagnosis of a depressive disorder.47,48 Interpersonal therapy has been tested primarily with Hispanic adolescents, but non-Hispanic adolescents made up one third of the sample in the trial by Mufson and colleagues.48 Mufson and colleagues also included adolescents with comorbid anxiety and were able to treat them successfully. Interpersonal therapy for adolescents has been administered only in an individual format. In both trials, mental health professionals were employed as therapists and were provided with additional training, supervision, and a manual to guide intervention.
Interpersonal therapy for adolescents is designed to reduce depressive symptoms by focusing on important interpersonal relationships, including the parent-child relationship, peer friendships, and romantic relationships. It stems from research indicating that significant interpersonal difficulties often both precipitate and maintain depression.49–51 Some features of interpersonal therapy for adolescents are reminiscent of CBT, but the overarching focus is the interpersonal problem associated with the onset of depression. Interpersonal therapy includes the following:
Summary and Recommendations
The evidence for the treatment of depression in children supports three psychological interventions: relaxation training, CBT, and interpersonal therapy. Of these, CBT currently has the most consistent evidence across a wide range of ages, ethnicities, and symptom severity levels. CBT has thus far been administered only by mental health professionals, the majority of whom received additional specialty training in those techniques. Therefore, we recommend referral to a child mental health provider specializing in CBT for depression. If trained providers are available, the clinician might consider referring Hispanic adolescents for interpersonal therapy, as this appears to be an effective treatment for that group, perhaps because of the fit between the principles of interpersonal therapy and the collectivist nature of Hispanic culture.48
PSYCHOLOGICAL MANAGEMENT OF ANXIETY AND FEARS
Anxiety disorders in children consist of anxiety that is excessive in its frequency, duration, and/or intensity so that it significantly interferes with functioning or causes distress. The anxiety disorders that affect children include separation anxiety disorder, generalized anxiety disorder, social phobia, specific phobia, panic disorder, agoraphobia, posttraumatic stress disorder, acute stress disorder, and obsessive-compulsive disorder. Estimates of the prevalence of anxiety disorders in childhood have varied widely, from 1.0% to 19.7%.52–34 There is evidence that more than 30% of the children seen in primary care settings have anxiety symptoms associated with some level of impairment, and as much as 15% meet diagnostic criteria for an anxiety disorder.54 For a more thorough review of the prevalence and expression of anxiety, see Chapter 18B.
We reviewed treatments for children with anxiety disorders and significant anxiety-related problems that did not meet full diagnostic criteria. We located randomized clinical trials in which psychological treatments for anxiety were examined, dating as early as 1967 and totaling 84 trials (testing 140 treatment conditions) by the end of 2005. In 52 (61.9%) of these studies, investigators used a no-treatment or wait-list control condition; of the remainder, 27 (32.1%) used an attention control condition, 1 (1.2%) used a placebo control condition, and 4 (4.8%) used standard case management, such as study skills training for children with test anxiety or incarceration. Several psychological interventions have shown positive effects across two or more controlled trials (Table 8D-2), including relaxation training, exposure, CBT, and client-centered therapy. Other interventions have not yet been examined in multiple studies (e.g., interventions targeting the parent only; insight-oriented therapies).
Exposure with Reinforcement, Relaxation, and/or Modeling
The majority of supported interventions involve controlled exposure to the feared object or situation (e.g., a specific object such as a spider or dog; public speaking; social interaction; separation from parents). Exposure has been tested as a stand-alone intervention in 29 studies; exposure is also a key component of CBT for anxiety (see later discussion). It has demonstrated positive effects across a wide range of ages, across diverse racial and ethnic groups, and both with children who show elevated levels of anxiety symptoms and those who meet diagnostic criteria for specific phobia55–57 and posttraumatic stress disorder (see Table 8D-2).58 One trial of exposure involved participants who had comorbid depression and enuresis and found that the presence or absense of comorbidity was unrelated to treatment outcomes.55
Exposure therapy has been administered successfully in both individual and group formats. In addition to producing beneficial effects when tested in research settings, it has also been used effectively in school settings58–63 and, once, in a dental practice.64 In one study, the investigators conducted exposure through videotaped modeling without the involvement of a therapist, but they achieved little success.65 The majority of successful trials of exposure therapy have employed mental health professionals; however, researchers in one study of children with dental fears successfully trained dental students to implement the procedures.64 In addition, most investigators have not reported extensive additional training, supervision, or manuals to guide intervention, but it is not clear from the published reports whether these efforts were unnecessary or simply not described.
Cognitive-Behavioral Therapy
CBT has received the greatest empirical attention in treating anxiety-related problems and disorders. CBT has been supported in versions targeting just the child for intervention (40 studies) and in versions targeting both the child and his or her parent or parents together (4 studies) and separately (9 studies). Two studies also included a teacher consultation component.66,67 This component has demonstrated positive effects across a wide range of ages, across diverse racial and ethnic groups, and both with children who show elevated levels of anxiety symptoms and with those who meet diagnostic criteria for social phobia,55,68–70 generalized anxiety disorder,70–77 separation anxiety,71–77 posttraumatic stress disorder,78 and obsessive-compulsive disorder.79–81 Several trials have revealed positive treatment effects even when participants have comorbid conditions in addition to their anxiety.55,67,68,72–74,76–82
CBT for anxiety has been successfully administered in both individual and group contexts. In addition to showing beneficial effects in research settings, it has also been used effectively in jail83 and school settings.61,75,84–86 In the majority of successful trials of CBT, the investigators have employed mental health professionals; however, two groups successfully trained college students to implement the procedures.87,88 The amount of additional specialty training and supervision has varied across studies, but in most, therapists were provided with a manual to guide intervention.
CBT for anxiety and CBT for depression share a focus on emotions, behaviors, and cognitions. However, exposure, which is not present in CBT for depression, is a core component of CBT for anxiety. Several different CBT manuals have been examined and shown success, including Coping Cat,89,90 FRIENDS,91–93 social effectiveness training,94 and family anxiety management.95
CBT for child anxiety typically involves the following:
 Cognitive restructuring (discussed previously; in this situation, anxiety-provoking thoughts are targeted).
Cognitive restructuring (discussed previously; in this situation, anxiety-provoking thoughts are targeted). Thought stopping or interruption (described previously; in this situation, anxious rumination is targeted).
Thought stopping or interruption (described previously; in this situation, anxious rumination is targeted). Fear hierarchy and planning for success (the child learns to generate a fear hierarchy to break down a big problem into smaller steps and to plan ahead for how he or she will successfully navigate anxiety-provoking situations).
Fear hierarchy and planning for success (the child learns to generate a fear hierarchy to break down a big problem into smaller steps and to plan ahead for how he or she will successfully navigate anxiety-provoking situations). Skill building (the child learns to improve skills that may contribute to his or her anxiety, such as social skills and problem-solving).
Skill building (the child learns to improve skills that may contribute to his or her anxiety, such as social skills and problem-solving). Reinforcement and self-reinforcement (described previously; in this situation, the rewards are for using coping skills and engaging in feared activities).
Reinforcement and self-reinforcement (described previously; in this situation, the rewards are for using coping skills and engaging in feared activities).As in CBT for child depression, parents of anxious children are often involved in their child’s treatment. During occasional check-in or complete sessions, parents are educated about the treatment their child is receiving and are provided with the necessary skills to implement intervention components with their child at home. In 15 studies, parents were provided with a more extensive intervention. For example, in family anxiety management training,95 parents are provided with a CBT program to help them deal with their own anxiety and to help them more effectively assist their child with the treatment program. The parents attend a group that covers essentially the same therapeutic content as in the child’s sessions (described previously). In addition, parents are taught to act as role models to show their children how to manage anxiety successfully. They also learn to provide reinforcement to their child for completing exposures and engaging in feared activities outside of sessions. Finally, parents learn to discourage repeated displays of anxiety through planned selective ignoring (e.g., the parent intentionally fails to notice their child’s whining or clinging, rather than responding by allowing the child to avoid a feared situation). Some of these studies directly tested the benefit of this additional parent involvement by comparing the effects of traditional child-focused CBT with child-focused CBT plus parent CBT. The results of these studies have been mixed, some indicating superior effects of combined treatments (e.g., Deblinger et al78) and others finding no differences (e.g., King et al67 and Nauta et al96).
PSYCHOLOGICAL MANAGEMENT OF INATTENTION, IMPULSIVITY, AND HYPERACTIVITY
ADHD includes three types of difficulties: (1) inattention, characterized by difficulty sustaining attention in tasks or play activities; (2) hyperactivity, characterized by excessive energy; and (3) impulsivity, characterized by difficulty controlling one’s actions, such as interrupting conversations or having difficulty waiting in line. Prevalence estimates of ADHD range from 0.9% to 8.0%.34,52,97 For a more thorough review of ADHD, please see Chapter 16.
Our review included treatment studies of children meeting diagnostic criteria for ADHD and those experiencing attention, impulsivity, or hyperactivity problems that do not meet full criteria for ADHD diagnosis. We found a total of 40 randomized clinical trials for ADHD and related problems (testing 73 treatment conditions) dating as far back as 1968 and as recently as the end of 2005. In 27 (67.5%) of these studies, investigators used an attention control group; of the remainder, 13 (32.5%) used a no-treatment or wait-list control condition; studies lacking a control condition, such as the Multimodal Treatment Study of ADHD study, were not included. Several types of psychological interventions—including client-centered therapy; modeling (e.g., the child observes a model demonstrating how to approach tasks in a careful, deliberate manner); and cognitively and behaviorally oriented interventions targeting only the child, the parent, or the teacher—have been examined for children with ADHD, but most have failed to show substantial benefits. However, we found some support for child-focused relaxation training in children with ADHD-related symptoms. In addition, although child-focused CBT, behavioral parent training (BPT), and teacher-focused consultation and classroom management training did not meet our effect size cutoff when administered in isolation, their use in combination showed quite positive effects for children with ADHD (Table 8D-3).
TABLE 8D-3 Evidence-Based Psychological Treatments for Attention-Deficit/Hyperactivity Disorder and Related Problems in Children
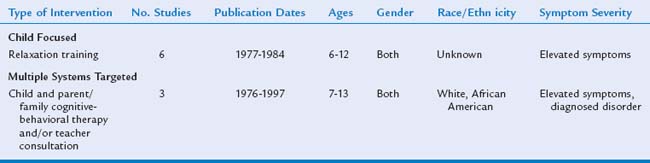
Relaxation Training
Relaxation training, including controlled breathing and muscle relaxation, was tested in six studies for children with inattention, impulsivity, and/or hyperactivity. It has been successfully implemented in both individual and group formats and has been used with success in school settings.98–101 Interestingly, despite the relative simplicity of these techniques, relaxation training for ADHD has been tested only with trained mental health professionals as therapists. Thus far, it has been examined only in children aged 6 to 12 who exhibited symptoms of inattention, impulsivity, and/or hyperactivity but who had no diagnosis of ADHD and no comorbid conditions. Furthermore, the studies are quite old in comparison with the rest of the evidence base (the newest one is dated 1984), and the samples are poorly described (e.g., no information is provided about the ethnicity of the clients). Thus, although relaxation training may be a worthwhile recommendation for children who show somewhat greater activity levels than others, it is unclear whether it would provide benefit for children with a diagnosis of ADHD.
Multimodal Cognitive and Behavioral Intervention
The most promising psychological intervention for children with ADHD is a combination of child-focused CBT, BPT, and/or teacher consultation or classroom management training (CMT). Some combination of these treatments has been tested in three trials: one trial involved CBT and CMT,102 and two trials involved CBT and BPT.103,104 These multitargeted interventions showed positive effects with both white and African American children between the ages of 7 and 13. They have been used successfully with children who had a diagnosis of ADHD, as well as undiagnosed hyperactivity problems. Furthermore, one trial successfully used this intervention with participants whose comorbid conditions included conduct disorder, oppositional defiant disorder, anxiety disorders, and dysthymic disorder.104 In each trial, mental health professionals were employed as therapists and were provided with either ongoing supervision or a manual to guide intervention.
In these multitargeted interventions, the children are taught self-control skills while parents and teachers are taught behavioral child management skills. Child CBT generally focuses on teaching children how to use self-instruction to reduce impulsivity, increase reflection and control, and improve performance on tasks requiring concentration. BPT is aimed at helping parents create contingencies in the home that will make appropriate, on-task behavior more rewarding than less desirable behavior. Iindividual or group sessions with the parents focus on learning and applying behavioral principles and methods. Coverage usually includes maximizing parental attention and praise in response to appropriate child behavior, withholding attention (and praise) when behavior is inappropriate, developing reward and incentive systems (e.g., charts, points, tokens) to encourage desired behavior, and using time-out and mild punishment (e.g., losing a point or privilege) for noncompliance. Parents are also taught how to issue commands aligned with the child’s ability to respond (e.g., issuing one directive at a time). Like BPT, teacher-focused CMT is aimed at helping teachers to establish and maintain contingencies at school that will reinforce self-control, attention to schoolwork, and appropriate social behavior with teachers and peers. Similar to BPT, coverage usually includes such behavioral interventions as developing reward and incentive systems (e.g., charts, points, tokens) to encourage desired behavior, issuing more appropriate instructions or commands, and organizing the classroom to help the child attend (e.g., seating the child near the front, removing distractions).
Summary and Recommendations
The evidence for the treatment of ADHD and associated symptoms supports two psychological interventions: relaxation training and multitargeted cognitive and behavioral treatment. Relaxation training has not been examined with children meeting diagnostic criteria for ADHD, and neither intervention has been examined in a controlled trial with children older than 13 years. In contrast, pharmacological interventions, and psychostimulants in particular, have shown consistently positive effects for children with ADHD (see Chapter 8C). Indeed, stimulant medication has repeatedly demonstrated superiority to psychological treatment (e.g., “Multimodal Treatment Study of Children with ADHD”105 and Abikoff et al106), although controversy still exists regarding whether a combination of medication and multimodal psychological treatment may be superior to medication alone (e.g., Pelham et al107), especially in children with comorbid anxiety and behavior problems108 or in children from more highly educated families.109 In view of the available evidence, medications are currently the treatment of choice for ADHD. Cognitive and behavioral interventions for the child, parent, and teacher may provide a helpful complement but are not recommended as the sole treatment for children with ADHD.