162 Trauma in the Gravid Patient
Trauma is the most common nonobstetric cause of death in pregnant women, accounting for 46% of maternal deaths.1 In the United States, 5% to 7% of all pregnancies are complicated by some form of traumatic injury.2 The most common mechanisms of blunt trauma are motor vehicle accidents (55%-70%), assaults (11%-21%) and falls (9%-22%).3,4 Penetrating trauma and burns are less common in most communities. The risk of trauma to the fetus increases as pregnancy progresses and the size of the uterus and fetus increases. The most common causes of fetal death are maternal hemorrhagic shock, abruptio placentae, and uterine rupture. A common maternal injury that results in fetal death is pelvic fracture, frequently leading to fetal skull fracture and intracranial injury. However, even relatively minor injuries to the mother can be devastating to the unborn child.5
The major causes of death from trauma (i.e., head injury and hemorrhage) are similar in gravid and nongravid patients. Patterns of injury are generally the same, based upon mechanism of injury. Hepatic and splenic injuries remain common, though gastrointestinal injuries are less common as the pregnancy progresses and the uterus enlarges.6
The outcome from trauma for the mother and fetus is dependent upon multiple factors, including gestational age of the fetus and the mechanism and severity of injury. The largest contributor to fetal mortality is gestational age less than 28 weeks.5 Scorpio et al.7 found in gravid victims of mostly blunt trauma (80% motor vehicle crashes) that injury severity score and admission serum bicarbonate level were the only independent factors that predicted fetal demise. The serum bicarbonate or base deficit may be important markers of occult hypoperfusion in trauma victims, though serum bicarbonate is normally decreased late in pregnancy. El Kady et al.5 and Schiff et al.8 reported that while the actual injury severity score was not predictive of fetal outcomes, maternal and fetal mortality were highest with internal injuries to the thorax, abdomen, and pelvis. The critical factor for the fetus is the extent to which trauma disrupts normal uterine and fetal physiology. Fetal demise occurs in up to 80% of gravid patients who develop hemorrhagic shock. In addition, however, even minor injuries to the mother can result in abruptio placentae or fetal demise.5 In one study of interpersonal violence as a cause of trauma in pregnancy, 5 of 8 women with fetal losses had no apparent physical injury.9
 Fetal Physiology
Fetal Physiology
On the positive side, amniotic fluid is a cushion for the fetus, but the fetus may still suffer injury as a result of rapid compression, deceleration, or contrecoup injury. Late in pregnancy, however, the head of the fetus is typically in the pelvis. Pelvic fractures may lead to fetal skull fracture and brain injury.4
 Initial Assessment and Resuscitation
Initial Assessment and Resuscitation
In addition to the standard initial assessment, evaluation of the gravid trauma patient should include a focused history and physical examination related to the pregnancy. The obstetric history should include the date of last menstrual period, expected date of delivery, date of first fetal movement, and status of current and previous pregnancies. The physical examination should include measurement of fundal height. Fetal age can be estimated as 1 week for each centimeter fundal height above the symphysis pubis. The abdominal examination should assess uterine tenderness and consistency, presence or absence of contractions, and determination of fetal position and movement. Pelvic examination should evaluate the presence of blood or amniotic fluid, cervical effacement, dilation, and fetal station. Amniotic fluid can be identified using Nitrazine paper to detect pH. A pH of 7 to 7.5 suggests the presence of amniotic fluid. Vaginal bleeding may indicate abruptio placentae. The Kleihauer-Betke (KB) test is used after maternal injury to identify fetal blood in the maternal circulation. When fetomaternal hemorrhage is present, additional doses of Rho(D) immunoglobulin may be given.10 Examination of the fetus beyond 20 weeks should include auscultation of fetal heart tones. Normal range is 120 to 160 bpm.
Radiographic Studies
The effect of radiation during development of the embryo and fetus is dependent upon dose and timing. Previously it was felt that any radiation very early in development of the embryo would be injurious. More recent findings, however, suggest that this is not the case, and that the fetus is most sensitive to the effects at 8 to 15 weeks when brain development is maximum.11 Radiation can be teratogenic and can retard growth or cause postnatal neoplasia, but the risk is low after 15 weeks gestation when organogenesis is nearly complete.
Mann et al.12 stratified risk of adverse effects of radiation for diagnostic studies. Less than 10 mGy (equivalent to 1 rad) was considered low risk, 10 to 250 mGy as intermediate risk, and over 250 mGy as high risk. In general, a single exposure for a plain radiograph results in an exposure of 2 mGy, whereas computed tomography (CT) may lead to an exposure of 5 mGy per slice and fluoroscopy as much as 10 mGy per minute. Exposure in the low category carries minimal risk of mutations. Though the risk of childhood cancers may be increased, the resultant risk remains less than 0.1%. In the intermediate category, specifically above 150 mGy, teratogenic effects may be seen. In the high category, the risk of teratogenic or carcinogenic effects increases significantly, perhaps to 2% to 3% above that of the normal population.
The greatest exposure to the fetus occurs when it is in the direct beam of the radiograph. To minimize exposure, the lower abdomen and pelvis of the gravid patient can be shielded with lead. Typical radiation exposure for the shielded fetus during a maternal chest radiograph is less than 0.01 mGy. In contrast, a pelvic CT scan for which the fetus cannot be shielded is 20 to 80 mGy.13 The exact efficacy of shielding with lead during these examinations is unclear.
Penetrating Trauma
As gestation progresses, the uterus becomes the most likely organ to be injured. The uterus and amniotic fluid can slow the velocity of missiles, decreasing potential injury to the mother, though not protecting the fetus very well. Approximately 60% to 70% of gunshot wounds to the pregnant abdomen result in fetal injury, with a subsequent fetal mortality of subsequently 40% to 65%.14 Penetrating trauma to the upper abdomen frequently involves multiple loops of bowel, which are compressed above the enlarged uterus, leading to complex injuries. Management of gravid patients with entry wounds below the fundus of the uterus is controversial. Although immediate laparotomy is indicated for most nongravid victims of penetrating abdominal trauma, particularly gunshot wounds, this is not the universal standard in the gravid patient. Nonoperative management can be employed if maternal vital signs and fetal heart rate tracings remain normal, suggesting no evidence of maternal or fetal compromise or intraabdominal hemorrhage.2 Radiographic determination of bullet location may be helpful. Intrauterine bullets may be observed. If laparotomy is performed, all bowel should be carefully explored and wounds repaired. Wounds to the uterus should also be closed. Antibiotics for gram-positive cocci and clostridia should be given as soon as possible.15 Also, tetanus prophylaxis is safe in pregnancy, and the indications for use in penetrating trauma patients are the same for pregnant and nonpregnant patients.
Medications
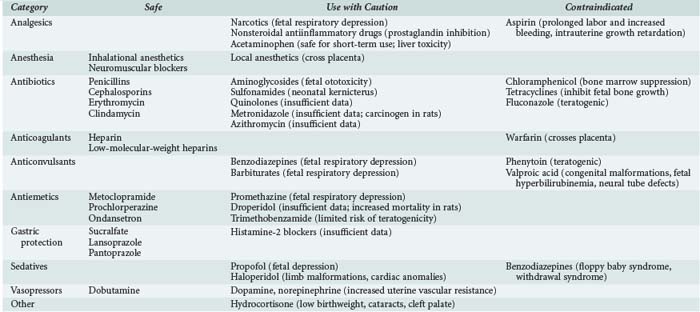
Medications frequently have different effects on the gravid patient and the fetus compared to normal, nongravid females. Table 162-1 lists commonly used medications and the current recommendations regarding their use during pregnancy. Because not all medications, particularly newer ones, have been extensively tested in pregnant women, all medications should be administered with some caution in the gravid patient.
Monitoring
Monitoring of fetal cardiac activity and maternal uterine activity (cardiotocographic monitoring) is indicated if the fetus has reached the point of viability if delivered. Since this complication can occur shortly after injury, monitoring should begin as soon as possible. Almost all patients who develop abruptio placentae have frequent uterine contractions (>8 per hour) during the first few hours after trauma; this is the most frequent finding with abruption. Continuous monitoring of the fetal heart beat can detect fetal distress quickly. Normal fetal heart rate is 120 to 160 beats/min. Signs of fetal distress include an abnormal baseline fetal heart rate, absence of normal accelerations and beat-to-beat variability, and repetitive decelerations. The duration of monitoring is somewhat controversial. Although delayed abruption has been reported,16,17 these patients were not monitored immediately after injury. Monitoring is clearly recommended for gravid patients with frequent uterine activity (>5 contractions per hour), abdominal or uterine tenderness, vaginal bleeding, rupture of amniotic membranes, or hypotension. Some have suggested that patients who are asymptomatic should be observed for at least 4 to 6 hours because approximately 80% of abruptions will occur during this interval.18 Fetal monitoring throughout a 24-hour observation admission may be performed, though the utility of continuous fetal monitoring beyond this point is limited.
The utility of ultrasound of the pelvis during initial management of the gravid patient is less clear. It is less accurate than cardiotocographic monitoring for detecting abruptio placentae or fetal distress, with a sensitivity of less than 50%.19 When a CT scan is performed on a pregnant trauma patient to look for abdominal or pelvic injuries, Manriquez et al. found that placental injuries could be diagnosed with 86% sensitivity and 98% specificity.20 On the other hand, ultrasound can also establish gestational age, determine fetal well-being if the cardiac monitoring is equivocal, verify presence or absence of fetal cardiac activity, and estimate the volume of amniotic fluid if rupture of membranes is suspected. Early obstetric consultation is critical so that if fetal distress occurs, rapid intervention, including Cesarean section, can proceed. Neonatology consultation may also be indicated.
 Specific Complications of Pregnancy
Specific Complications of Pregnancy
Fetomaternal Hemorrhage
Following trauma, fetal blood can cross the placenta and enter the maternal circulation. This occurs in 10% to 30% of pregnant trauma patients.15 The volume can be approximated by measuring the ratio of fetal to maternal red blood cells in the maternal circulation with the Kleihauer-Betke (KB) test. Complications include Rh sensitization of the mother, neonatal anemia, cardiac arrhythmias in the fetus, and fetal death from exsanguination. Maternal sensitization may be prevented by administration of Rho(D) immune globulin. Because the KB test may not be sensitive enough to detect the amount of fetal hemoglobin that can sensitize the mother, administration of Rho(D) immune globulin is indicated in almost all Rh-negative mothers unless the injury is relatively minor and far removed from the uterus. In addition, positive KB tests should be repeated in 24 to 48 hours to follow the progression of fetomaternal hemorrhage.18
Premature Labor
Premature uterine contractions associated with cervical dilatation and effacement (i.e., signs of premature labor) are common after trauma. A positive KB test may be one of the most predictive factors for premature labor.18 Fortunately, premature labor is usually self-limited, but some patients require tocolytics. Evidence of abruptio placentae is a contraindication to tocolytic therapy.
Cardiac Arrest
During resuscitation, standard algorithms should be applied initially. The uterus can be manually displaced toward the left side, off the inferior vena cava. Optimizing cardiac output and perfusion of the uterus via left thoracotomy and open cardiac massage along with emergency Cesarean section should be considered. By the time the mother has suffered a cardiac arrest from trauma, the fetus has already suffered severe hypoxia. Cesarean delivery may be indicated if the fetus is thought to be viable and the procedure can be performed within 5 minutes of the loss of pulse in the mother.2 If fetal vital signs persist, delivery may be performed after 5 minutes, though survival becomes less likely as time passes. Cardiopulmonary resuscitation must be continued until delivery is accomplished. Delivery has also been reported to allow successful maternal resuscitation. Decision to proceed with postmortem delivery must be made quickly by the traumatologist and obstetrician; hemostasis and antisepsis become secondary issues. Perimortem Cesarean delivery is performed via a midline incision through all layers of the uterus. Neonatologists must be available.
 Prevention
Prevention
Ikossi et al. revealed that 19.6% of pregnancy-related trauma was associated with illicit drug use, and 12.9% involved alcohol.22 Education about the risks of drug and alcohol use during pregnancy is needed for all women, especially those in high-risk situations.
Proper seat belt use improves survival after motor vehicle crashes by preventing ejection from the vehicle. According to the National Highway Traffic Safety Administration, the lap belt should cross over the bony pelvis as low as possible under the pregnant belly, with the shoulder belt between the breasts and away from the neck.15 The shoulder belt can help dissipate the force of deceleration and prevent severe flexion at the waist. Although standard seat belt and shoulder harnesses were not specifically designed for the gravid patient, it is estimated that up to 50% of fetal losses following motor vehicle collisions could be prevented if seat belts are used correctly.23
Violent trauma is a major cause of maternal and fetal death that is most likely quite under-reported.15,18 Approximately 17% to 32% of gravid trauma patients have reported being injured by another person, and up to 60% of these are repeated cases of domestic violence.3 Factors that should raise concern about domestic violence include injuries inconsistent with the history, diminished self-image, depression, history of self-abuse or suicide attempts, substance abuse, self-blame for injuries, and frequent visits. One should also be concerned if the partner insists upon being present for the examination and monopolizes the conversation. Physicians have a responsibility to identify these injuries and document them with the appropriate authorities.
Key Points
Sosa ME. The pregnant patient in the intensive care unit: collaborative care to ensure safety and prevent injury. J Perinat Neonatal Nurs. 2008;22:33-38.
Pearlman MD, Tintinalli JE, Lorenz RP. Blunt trauma during pregnancy. N Engl J Med. 1990;23:1609-1613.
Cusick SS, Tibbles CD. Trauma in pregnancy. Emerg Med Clin North Am. 2007;25:861-872.
Weiss HB, Songer T, Fabio A. Fetal deaths related to maternal injury. JAMA. 2001;286:1863-1868.
Brent RL. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Am J Obstet Gynecol. 2009;200:4-24.
1 National Vital Statistics Reports, Volume 53, Number 16. http://www.cdc.gov/nchs/data/nvsr/nvsr53/nvsr53_16.pdf, March 7, 2005. Available at
2 Muench MV, Canterino JC. Trauma in pregnancy. Obstet Gynecol Clin North Am. 2007;34(3):555-583.
3 Mattox KL, Goetzl L. Trauma in pregnancy. Crit Care Med. 2005;33:S385-S389.
4 Weiss HB, Songer T, Fabio A. Fetal deaths related to maternal injury. JAMA. 2001;286:1863-1868.
5 El Kady D. Perinatal outcomes of traumatic injuries during pregnancy. Clin Obstet Gynecol. 2007;50(3):582-591.
6 Brooks DC, Oxford C. The pregnant surgical patient. ACS surgery: principles and practice, 6th ed. New York: WebMD Professional Publishing; 2007. 1-21
7 Scorpio RJ, Esposito TJ, Smith LG, Gens DR. Blunt trauma during pregnancy: Factors affecting fetal outcome. J Trauma. 1992;32:213-216.
8 Schiff MA, Holt VL. Pregnancy outcomes following hospitalization for motor vehicle crashes in Washington State from 1989 to 2001. Am J Epidemiol. 2005;161:503-510.
9 Poole GV, Martin JN, Perry KG, et al. Trauma in pregnancy: The role of interpersonal violence. Am J Obstet Gynecol. 1996;174:1873-1877.
10 Mirza FG, Devine PC, Gaddipati S. Trauma in pregnancy: A systematic approach. Am J Perinatol. 2010. Epub ahead of print
11 Patel SJ, Reede DL, Katz DS, Subramaniam R, Amorosa JK. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose consideration. Radiographics. 2007;27(6):1705-1722.
12 Mann FA, Nathens A, Langer SG, Goldman SM, Blackmore CC. Communicating with the family: The risks of medical radiation to conceptuses in victims of major blunt-force torso trauma. J Trauma. 2000;48:354-357.
13 Kusama T, Oka K. Radiologic protection for diagnostic examination of pregnant women. Congenital Anomalies. 2002;42:10-14.
14 Petrone P, Asensio JA. Trauma in pregnancy: assessment and treatment. Scand J Surg. 2006;95(1):4-10.
15 Hill CC, Pickinpaugh J. Trauma and surgical emergencies in the obstetric patient. Surg Clin North Am. 2008;88(2):421-440.
16 Lavin JP, Miodovnik M. Delayed abruption after maternal trauma as a result of an automobile accident. J Reprod Med. 1981;26:621-624.
17 Higgins SD, Garite TJ. Late abruption placenta in trauma patients: implications for monitoring. Obstet Gynecol. 1984;63:10S-12S.
18 Oxford CM, Ludmir J. Trauma in pregnancy. Clin Obstet Gynecol. 2009;52(4):611-629.
19 Glantz C, Purnell L. Clinical utility of sonography in the diagnosis and treatment of placental abruption. J Ultrasound Med. 2002;21:837-840.
20 Manriquez M, Srinivas G, Bollepalli S, Britt L, Drachman D. Is computed tomography a reliable diagnostic modality in detecting placental injuries in the setting of acute trauma? Am J Obstet Gynecol. 2010. Epub ahead of print
21 Powner DJ, Bernstein IM. Extended somatic support for pregnant women after brain death. Crit Care Med. 2003;31:1241-1249.
22 Ikossi DG, Lazar AA, Morabito D, et al. Profile of mothers at risk: An analysis of injury and pregnancy loss in 1195 trauma patients. Am Coll Surg. 2005;200:49-56.
23 Klinich KD, Rupp JD. Fetal outcomes in motor-vehicle crashes: effects of crash characteristics and maternal restraint. Am J Obstet Gynecol. 2008;198:450e1-450e9.