Trauma
Mortality of spine-related trauma in children is higher than in adults and is estimated at 25% to 32%.1 Fortunately, children with incomplete neurologic lesions fare better compared with adults, with up to 90% having partial recovery and 60% having full recovery.1,2
Etiology
Motor vehicle accidents (MVAs), followed by falls and sports injuries, are the most common causes of pediatric spinal trauma. Young athletes are at higher risk for developing stress-related injuries than are adult athletes.3 Gunshot injuries accounted for 22% of injuries in one study of 277 pediatric patients with spinal trauma.4 Congenital spine anomalies such as os odontoideum, block vertebrae, Klippel-Feil syndrome, and Down syndrome increase the risk of cervical spinal injury. Nerve root avulsion with pseudomeningocele formation may result from birth trauma, MVAs, or less often, penetrating injury (Fig. 47-1).5
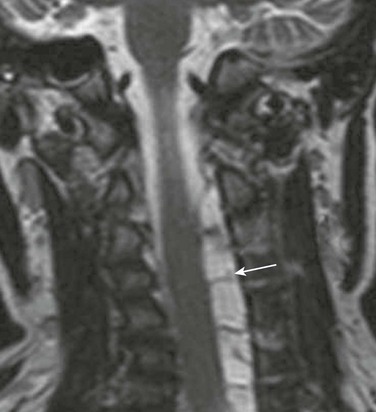
Figure 47-1 Avulsed nerve roots in a 13-year-old girl unable to use her left arm after an all-terrain vehicle accident.
A coronal T2-weighted magnetic resonance image shows an extensive intradural cerebral spinal fluid collection (arrow) shifting the spinal cord (C) to the right due to C2 to T1 nerve root avulsions.
Younger children are more susceptible to upper cervical injuries compared with adults because of their relatively large-sized, heavy craniums and weaker neck muscles.6 This anatomy causes a more cranial fulcrum of movement at C2-C3 in younger children versus C5-C6 in older children and adults.1 Injuries in younger children, especially those under 8 years, differ from those in older children. Because of greater mobility and laxity of ligaments in the cervical spine of younger children, they tend to have higher cervical injuries (occiput to C3). These injuries are more likely associated with a neurologic deficit and to extend through synchondroses.7
SCIWORA
The unique biomechanical properties of young children, including their large-sized heads and higher fulcrum of motion, causes increased occurrence of spinal cord injury without radiographic abnormality (SCIWORA). The acronym SCIWORA was popularized in the early 1980s to describe children with clinical symptoms of cervical cord trauma and normal radiographs.8 With the introduction of magnetic resonance imaging (MRI), injuries in children with SCIWORA could be visualized and the general prognosis predicted on the basis of the findings.9,10 MRI allows for the diagnosis of SCIWORA by easily showing the findings of cord contusion, including hypointensity on T1-weighted imaging and hyperintensity on T2-weighted imaging, cord hemorrhage, or cord transaction (Fig. 47-2).11 The presence of normal cord signal suggests the child will make a complete recovery, whereas intramedullary hemorrhage and transection portend a poor prognosis.8
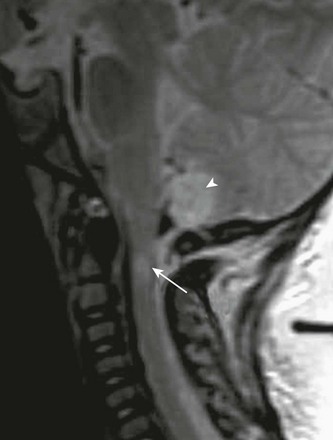
Figure 47-2 Spinal cord injury without radiographic abnormality (SCIWORA) in a 6-year-old boy with paraplegia after a fall from a horse and normal cervical spine radiographs.
Sagittal magnetic resonance image of the craniocervical junction reveals hyperintense T2 contusions within the cervical spinal cord (arrow) and the inferior cervical vermis (arrowhead). Note T2 dark hemorrhage in the cerebral spinal fluid at the level of the foramen magnum just below the vermian contusion.
Atlanto-Occipital Disassociation
Because of their relatively small occipital condyles and more horizontal atlanto-occipital joint orientation, young children are at increased risk for atlanto-occipital disassociation.2,9,12 Devastating spinal cord injury often occurs, and many cases are fatal. A diagnosis is made by measuring a condylar gap greater than 5 mm (Kaufman condylar gap) or a basion to axis interval (BAI) of greater than 12 mm (Fig. 47-3).2 One pitfall is that in children younger than 13 years, the BAI is less reliable.12 Some helpful measurements to evaluate pediatric cervical spine trauma are listed in Table 47-1.13 Atlanto-occipital dissassociation requires urgent stabilization.
Table 47-1
Cervical Spine Measurements Useful in Evaluation of Pediatric Trauma
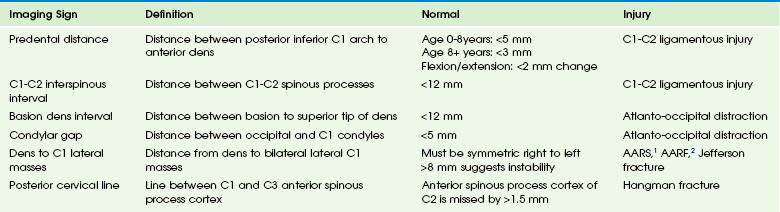
AARS, atlantoaxial rotatory subluxation; AARF, atlantoaxial rotatory fixation.

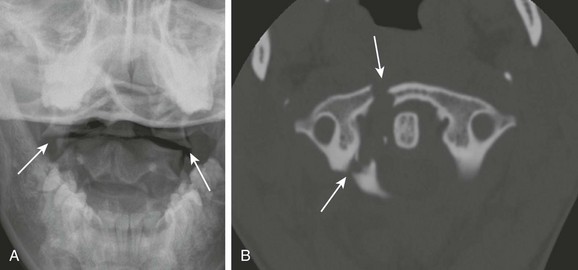
Figure 47-3 Atlantoaxial disassociation in a 5-year-old unrestrained girl after a motor vehicle accident.
Lateral cervical spine radiograph demonstrates abnormally increased basion to dens distance of 15 mm (white line). The C1-C2 interspinous distance is also increased at greater than 12 mm (arrow).
Atlas or Jefferson Fracture
Compression loading forces on the cervical spine can result in a C1 burst fracture, or Jefferson fracture. This injury is most common in adolescents from MVAs and diving accidents. Jefferson fractures show between one and four defects in the C1 ring. The fracture may be stable or unstable, depending on whether or not the transverse ligament is intact or ruptured, respectively. A single defect in the ring is typically stable, whereas three or four defects are typically unstable.9 A dens to C1 lateral mass distance of greater than 8 mm suggests instability. Forty percent of Jefferson fractures have an associated C2 fracture.12 Lateral cervical spine radiographs are of little value, and the diagnosis is made on the open-mouth odontoid view by showing offset of the lateral masses of C1 on C2 (Fig. 47-4).13 Pitfalls to avoid include rotation of the head on the open-mouth view that may cause the lateral mass to appear slightly laterally displaced, hypermobility in young children that may lead to minimal normal lateral displacement of C1 on C2 and finally, the normal developmental bilateral offset of the C1 lateral masses that may occur in children under 2 years of age because of the differential growth of C1 versus C2.9
Atlantoaxial Rotatory Force Injury
The atlantoaxial joint is responsible for 50% of normal range of motion of the neck. Temporary ligamentous laxity following infection or surgery in the head and neck because of hyperemic, inflamed synovial tissues with secondary contractures causes mild atlantoaxial rotatory subluxation (AARS), or Grisel syndrome. A similar situation, sometimes referred to as “wry neck,” occurs in normal children who simply awaken with a stiff neck and are unable to turn their head to one side.9 Grisel syndrome and wry neck represent a mild form of C1 on C2 rotatory subluxation that is caused by muscle spasm and is self-limiting. With frank rotatory dislocation, children present with torticollis, holding their heads in a peculiar “cock robin” position, head rotated to one side and tilted to the other.2 The duration of subluxation is proportional to the risk of recurrence. When rotatory injury is fixed, the term atlantoaxial rotatory fixation (AARF) may be applied. Atlantoaxial rotatory force injury is classified into four types, according to Fielding and Hawkins (Table 47-2).14 Mild rotatory anomalies may be treated with muscle relaxers and physical therapy, but more aggressive management may include traction and, rarely, surgery, to prevent osseous fusion at C1-C2.2 An imaging diagnosis of AARS is suggested by the presence of asymmetry in the dens to C1 lateral mass distance on open-mouth odontoid radiographs and computed tomography (CT) scans (Fig. 47-5). CT signs of rotatory disorders include loss of articulation of the occiput and C1 as well as sclerosis on both sides of the joint with impending fusion (Fig. 47-6).
Table 47-2
Fielding Classification of Atlantoaxial Rotatory Subluxation
| Type | Description |
| I | Rotatory displacement of C1 on dens without anterior displacement; most common type |
| II | 3-5 mm of anterior C1 displacement with rotation centered on the lateral facets possibly disrupting the transverse ligaments |
| III | >5 mm anterior C1 displacement with rotation centered on lateral facets possibly disrupting the transverse ligament, alar ligament, and facet capsule |
| IV | Posterior C1 displacement on C2 of both lateral facets; rarely seen in adults with rheumatoid arthritis |

Figure 47-5 Atlantoaxial rotatory subluxation in a 13-year-old girl with torticollis for 2 weeks and no history of infection or trauma.
A coronal reconstructed cervical spine computed tomography image shows widening of the atlantodental distance on the left (arrow) compared with the normal right side. This distance widened and narrowed when turning the head to the left and the right, respectively (dynamic CT not shown).
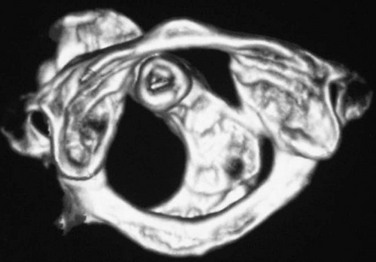
Figure 47-6 Atlantoaxial rotatory fixation (Fielding type 1) in a 15-year-old girl with rigid torticollis for 4 weeks following spinal manipulation.
An axial three-dimensional cervical computed tomography image reveals rotation of C1 on C2 with loss of articulation of the condyles, but without anterior displacement of C1. Note normal distance between C1 and dens, which indicates a Fielding type 1 injury.
Odontoid (Dens) Fractures
Dens fractures, or odontoid fractures, are common in all age groups. The rigid, upright nature of dens makes it susceptible to a variety of flexion, loading, and extension forces.9 In young children, the odontoid is separated from the body of C2 by a cartilaginous synchondrosis, which fuses between the ages of 5 and 7 years.9 The presence of the synchondrosis in infants and young children allows fractures to occur frequently through this growth plate, but fortunately, these fractures heal readily (Fig. 47-7). However, in adults, these fractures often interfere with blood supply to the odontoid, causing the fractures to be complicated by nonunion or pseudoarthroses.1 Dens fractures are classified into three types, with only type 2 being unstable. Type 1 is through the tip of the dens, type 2 is through the base of the dens, and type 3 is through the body of C2.2,9
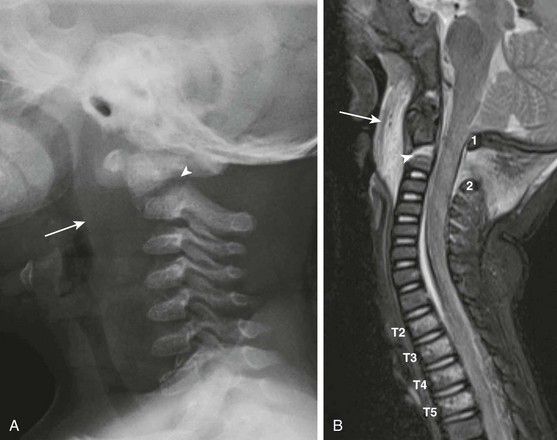
Figure 47-7 Odontoid fracture in a 12-month-old girl after a motor vehicle accident.
A, Lateral cervical radiograph shows prevertebral soft tissue swelling (arrow), widening of the C2 synchondrosis (arrowhead), and anterior subluxation of the dens on the body of C2. B, Sagittal T2-weighted fat suppressed magnetic resonance image confirms the radiographic findings and also reveals additional vertebral contusions as hyperintense marrow signal of T2-T5. Ligamentous injury is seen as increase in the C1-C2 interspinous interval, which is filled with T2 bright soft tissue edema.
A pitfall to consider when searching for odontoid fractures is the presence of an os odontoideum, an oval or round ossicle of variable size with a smooth cortical border located in the expected position of the odontoid process. Small os odontoideums at the tip of the dens may be normal variants of no significance; however, when they are large enough to extend below the annular ligament, they could be unstable and susceptible to traumatic injury.9 The etiology is controversial, but they are likely both posttraumatic and congenital in origin.2,15
Hangman Fracture
Hyperextension forces may cause fractures through the C2 pars intraarticularis, known as the hangman fracture. Often, these fractures are more complex in morphology being associated with combined flexion and extension forces in the same patient.9 The C2 fracture lucency is diagnostic but may be difficult to visualize on neutral lateral radiographs (Fig. 47-8). It is more easily detected with flexion views. Application of the posterior cervical line (see Table 47-1) is helpful to diagnose the injury.9 Hangman fractures may be unilateral or bilateral, in which case they are stable or unstable, respectively. In infants, one must be aware of the pitfall of congenital defects of C2 being confused with a hangman fracture. Congenital defects are distinguished by smooth, sclerotic, narrow margins. When hangman fractures are caused by airbag injuries, a high association with facial fractures exists.9,16
Thoracic and Lumbar Spine Fractures
Cervicothoracic junction injury is associated with breech deliveries, many of which present as SCIWORA or brachial plexus injuries, as previously discussed.2 Associated findings also include T1 and T2 transverse process fractures.
Lower thoracic and upper lumbar spine injuries are most often caused by MVAs, with up to 50% having associated small bowel injury from seat-belt trauma.2,17 Common lower thoracic and lumbar fractures include anterior column compressions, which are typically stable, and posterior column burst fractures, which are typically unstable (Fig. 47-9). Burst fractures occur with axial compression forces, causing endplate fracture extending into the anterior and posterior column (Fig. 47-10). Chance or seatbelt fractures are caused by flexion injury with horizontal extension through the posterior vertebral body, pedicles, and spinous processes (Fig. 47-11).2

Figure 47-9 Cervical spine compression fractures and cord contusion in a 17-year-old male after an all-terrain vehicle accident.
A sagittal T2-weighted magnetic resonance image shows hyperintense signal and decreased height of the anterior C4 and C5 vertebral bodies (arrows). T2 bright signal cord contusion is seen at the C5 level (arrowhead).
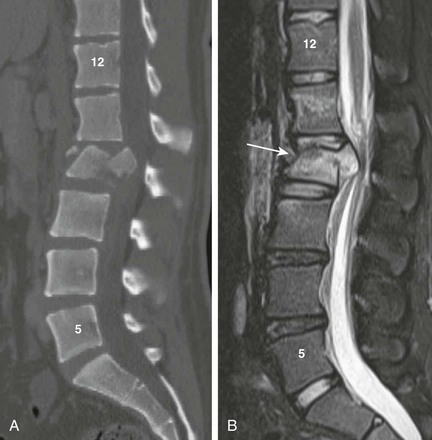
Figure 47-10 Burst fracture in a 16-year-old male with leg pain and weakness after a motor vehicle accident.
A, A sagittal reformatted computed tomography image identifies a comminuted L2 fracture with a retropulsed fragment in the spinal canal. B, A sagittal FLAIR (fluid attenuated inversion recovery) magnetic resonance image confirms the fracture with retropulsed fragment compressing the cauda equina (arrow). In addition, T2 bright signal contusions in the adjacent L1 and L3 vertebral bodies are present.

Figure 47-11 Chance fracture in a 5-year-old-boy unable to move his legs after a motor vehicle accident.
A sagittal T2-weighted magnetic resonance image shows a horizontal fracture through the superior endplate and pedicles of L4 (arrow). Associated surrounding T2 bright soft tissue edema is also seen.
Spondylolysis
Spondylolysis may be a congenital deformity or an acquired stress fracture extending through the pars interarticularis. It is thought to be most likely caused by repetitive flexion and extension in the adolescent spine and is often seen in athletes, having been reported in 11% of female gymnasts.18 Lucency extends through the pars on radiography and CT, with MRI showing T2 bright signal in stress reactions and acute cases. Spondylolysis without spondylolisthesis is treated conservatively. Spondylolisthesis may require orthopedic stabilization depending on severity.
Spinal Cord Contusions and Transections
Spinal cord contusions and transections are a continuum of cord injuries that occur alongside fractures, ligamentous injuries, or both. Contusions are thought to occur secondary to shearing injuries, with rupture of the small intramedullary vessels resulting in focal petechia and edema, which, in some cases, progress to larger areas of hemorrhage in the cord and vascular compromise.17 Complete cord transection, which has a very poor prognosis, typically results from extreme distraction or severe transverse shear injury (Fig. 47-12).10

Figure 47-12 Cord transection in a newborn with distractive birth injury.
A sagittal short tau inversion recovery magnetic resonance image shows disruption of the cervical vertebral column at C5-C6, transection of the spinal cord, and focal hyperintense signal within cord consistent with hyperacute edema and hemorrhage (arrow).
Egloff, AM, Kadom, N, Vezina, G, et al. Pediatric cervical spine trauma imaging: a practical approach. Pediatr Radiol. 2009;39:447–456.
Gore, PA, Chang, S, Theodore, N. Cervical spine injuries in children: attention to radiographic differences and stability compared to those in the adult patient. Semin Pediatr Neurol. 2009;16:42–58.
Lustrin, ES, Karakas, SP, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539–560.
References
1. Arvin, B, Fournier-Gosselin, MP, Fehlings, MG. Os odontoideum: etiology and surgical management. Neurosurgery. 2010;66(3 suppl):22–31.
2. Roche, C, Carty, H. Spinal trauma in children. Pediatr Radiol. 2001;31(10):677–700.
3. Maxfield, BA. Sports-related injury of the pediatric spine. Radiol Clin North Am. 2010;48(6):1237–1248.
4. Haffner, DL, Hoffer, MM, Wiedbusch, R. Etiology of children’s spinal injuries at Rancho Los Amigos. Spine (Phila Pa 1976). 1993;18(6):679–684.
5. Freedy, RM, Miller, KD, Jr., Eick, JJ, et al. Traumatic lumbosacral nerve root avulsion: evaluation by MR imaging. J Comput Assist Tomogr. 1989;13(6):1052–1057.
6. Junewick, JJ. Pediatric craniocervical junction injuries. AJR Am J Roentgenol. 2011;196:1003–1010.
7. Khanna, G, El-Khoury, GY. Imaging of cervical spine injuries of childhood. Skelet Radiol. 2007;36(6):477–494.
8. Pang, D, Wilberger, JE, Jr. Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1982;57(1):114–129.
9. Swischuk, LE. Imaging of the cervical spine in children. In: Swischuk LE, ed. Imaging of the cervical spine in children. New York: Springer; 2002:112–113.
10. Grabb, PA, Pang, D. Magnetic resonance imaging in the evaluation of spinal cord injury without radiographic abnormality in children. Neurosurgery. 1994;35(3):406–414. [discussion 414].
11. Georgy, BA, Hesselink, JR. MR imaging of the spine: recent advances in pulse sequences and special techniques. AJR Am J Roentgenol. 1994;162(4):923–934.
12. Harris, JH, Jr., Carson, GC, Wagner, LK, et al. Radiologic diagnosis of traumatic occipitovertebral dissociation: 2. Comparison of three methods of detecting occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162(4):887–892.
13. el-Khoury, GY, Kathol, MH, Daniel, WW. Imaging of acute injuries of the cervical spine: value of plain radiography, CT, and MR imaging. AJR Am J Roentgenol. 1995;164(1):43–50.
14. Fielding, JW, Hawkins, RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am. 1977;59(1):37–44.
15. Arvin, B, Fournier-Gosselin, MP, Fehlings, MG. Os odontoideum: etiology and surgical management. Neurosurgery. 2010;66:22–31.
16. Giguere, JF, St-Vil, D, Turmel, A, et al. Airbags and children: a spectrum of C-spine injuries. J Pediatr Surg. 1998;33(6):811–816.
17. Green, NE, Swiontkowski, MF. Skeletal trauma in children, 4th ed. Philadelphia, PA: Saunders; 2009.
18. Ogden, JA. Skeletal injury in the child, 2nd ed. Philadelphia, PA: Saunders; 1990.